Abstract
Portal vein thrombosis (PVT) is a thrombosis that develops in the trunk of the portal vein which can extend to its branches. It results from a combination of local and systemic prothrombotic factors. Anticoagulation is generally considered in PVT patients as long as the risk of bleeding is low. Limited data have been published regarding spontaneous resolution of PVT. We describe two cases of asymptomatic PVT who were not given anticoagulation in view of several factors, who, on repeat scans, showed resolution of their thrombus.
Keywords: portal vein thrombosis, PVT and cirrhosis, PVT and intraabdominal abscess, spontaneous resolution of PVT
The portal vein is formed by the confluence of the splenic vein (which drains the spleen) and superior mesenteric veins (which drain the small intestine). Portal vein thrombosis (PVT) is a thrombosis that develops in the trunk of the portal vein which can extend to its branches. It results from a combination of local and systemic prothrombotic factors.1 Anticoagulation is generally considered in PVT patients as long as the risk of bleeding is low. Limited data have been published regarding the spontaneous resolution of PVT.
We describe two cases of asymptomatic PVT who were not given anticoagulation in view of several factors, and on repeat scans, showed resolution of their thrombus.
Case Report 1
A 77-year-old male patient was admitted at Tan Tock Seng Hospital, Singapore for a 2-week history of progressive jaundice associated with tea-colored urine. He reported one episode of nonbloody and nonbilous vomiting. He also had chills for the past 2 days, before his admission. There was no fever, diarrhea, abdominal pain, pale stools, hematochezia or melena noted. He had a background history of hypertension and appendectomy.
On admission, he was febrile with temperature of 37.9°C, blood pressure 120/80 mm Hg, heart rate 80/min. Examination revealed the presence of icteric sclerae. Abdomen was soft and nontender. Murphy sign was negative. The rest of the examination was unremarkable. The blood results are shown in Tables 1, 2, and 3.
Table 1. Results showing the hemogram and renal panel of case 1.
| Normal values | ||
|---|---|---|
| White blood cell | 23 × 109/L | 3.6–9.39/L |
| Neutrophil | 91.6% | |
| Hemoglobin | 11.7 g/dL | 13–17 g/dL |
| Platelet | 147 × 109/L | 170–4209/L |
| Sodium | 133 mmol/L | 134–144 mmol/L |
| Potassium | 3.8 mmol/L | 3.5–5.0 mmol/L |
| Creatinine | 125 µmol/L | 60–105 µmol/L |
| Urea | 6.5 mmol/L | 2.9–9.3 mmol/L |
Table 2. Results showing the liver function test and amylase of case 1.
| Normal Values | ||
|---|---|---|
| ALT | 111 U/L | 14–54 U/L |
| AST | 113 U/L | 15–41 U/L |
| ALP | 237 U/L | 38–126 U/L |
| GGT | 525 U/L | 7–50 U/L |
| Total Bilirubin | 184 umol/L | 7–31 umol/L |
| Albumin | 33 g/L | 35–48 g/L |
| Amylase | 641 U/L | 36–128 U/L |
Abbreviations: ALT, alanine transaminase; AST, aspartate transaminase; ALP, alkaline phosphatase; GGT, gamma glutamyl transferase.
Table 3. Results showing the hepatitis screen of case 1.
| Anti-HAV IgM | Nonreactive |
|---|---|
| Anti-HBs | < 10 IU/L |
| HbsAg | Nonreactive |
| Anti-HCV | Nonreactive |
Abbreviations: HAV, hepatitis A virus; HBs; hepatitis B surface; HbsAg; hepatitis B surface antigen; HCV, hepatitis C virus.
An abdominal computed tomography (CT) was done which showed hyperdensity in the distal most common bile duct suggestive of calculi; mild dilatation and wall enhancement of the biliary tree suggestive of cholangitis and wall-enhancing hypodense lesion in segment four of the liver likely abscess; and thrombosis of the segmental branches of the right portal vein (Fig. 1). He was treated with antibiotics and suggested to withhold anticoagulation for the meantime. His thrombophilia screen was done (Table 4).
Fig. 1.
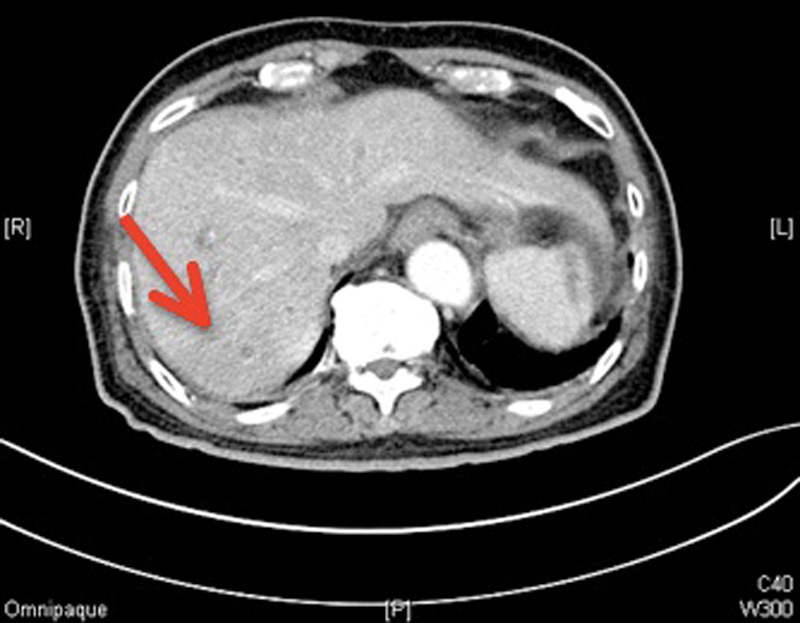
CT scan showing an incidental thrombus of the segmental branches of the right portal vein (arrow). CT, computed tomography.
Table 4. Results showing the thrombophilia screen and PT/INR results of case 1.
| Normal values | ||
|---|---|---|
| Factor V Leiden | Normal | |
| Anticardiolipin IgG | 9 GPL U/mL | < 10 U/mL |
| Anticardiolipin IgM | 1 MPL U/mL | < 10 U/mL |
| APC resistance test | 1.09 | 1.0–1.3 |
| Antithrombin III | 70% | 80–130% |
| Lupus anticoagulant | Absent | |
| Protein C activity | 55% | 70–150% |
| Protein S activity | 67% | 65–130% |
| PT | 13.7 s | 11.7–14.0 s |
| APTT | 31.1 s | 25–36 s |
| INR | 1.08 |
Abbreviations: APC, activated protein C; APTT, activated partial thromboplastin time; INR, international normalized ratio; PT, prothrombin time.
Progress
He was given a 1-week course of antibiotics (ceftriaxone and metronidazole). He then underwent endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy. Two mixed stones were removed with a balloon catheter.
Postremoval occlusive cholangiogram showed a complete ductal clearance. Post-ERCP showed clinical and biochemical improvement. No anticoagulation was recommended as the PVT was thought to be due to an underlying inflammation/infection intra-abdominally. The repeat abdominal CT scan done 6 months later showed clearance of the PVT (Fig. 2).
Fig. 2.

CT scan showing resolution of the previously thrombosed segments of the portal vein (arrow). CT, computed tomography.
Case Report 2
A 60-year-old female patient with child's B cryptogenic liver cirrhosis was admitted on 30 April, 2012 for gastroenteritis and a left breast lump. She also has a background of diabetes mellitus, hypertension, and stroke. She presented with watery, nonbloody, nonmucoid stools of 2-day duration associated with abdominal bloatedness. No fever was noted. On physical examination, vitals were stable, she was noted to have a left breast mass and distended abdomen with ascites.
Her investigations are shown in Tables 5 and 6. She underwent CT scan of the abdomen which showed the presence of nonocclusive portal vein thrombus (Fig. 3).
Table 5. Hemogram, renal panel, and CRP results of case 2.
| Normal values | ||
|---|---|---|
| White blood cell | 6.2 × 109/L | 3.6–9.39/L |
| Neutrophil | 91.6% | |
| Hemoglobin | 9.1 g/dL | 13–17 g/dL |
| Platelet | 116 × 109/L | 170–4209/L |
| CRP | 15.5 mg/L | 0.0–5.0 mg/L |
| Sodium | 133 mmol/L | 134–144 mmol/L |
| Potassium | 4.6 mmol/L | 3.5–5.0 mmol/L |
| Creatinine | 115 µmol/L | 60–105 µmol/L |
| Urea | 8.6 mmol/L | 2.9–9.3 mmol/L |
Abbreviation: CRP, C-reactive protein.
Table 6. Liver function tests and PT/INR results of case 2.
| Normal values | ||
|---|---|---|
| APTT | 33.4 s | 25–36 s |
| PT | 16.2 s | 11.7–14.0 s |
| INR | 1.34 | |
| ALT | 27 U/L | 17–63 U/L |
| AST | 42 U/L | 15–41 U/L |
| ALP | 60 U/L | 38–126 U/L |
| GGT | 64 U/L | 7–50 U/L |
| Total bilirubin | 25 µmol/L | 7–31 U/L |
| Albumin | 29 g/L | 35–48 g/L |
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; APTT, activated partial thromboplastin time; AST, aspartate transaminase; GGT, gamma glutamyl transferase; INR, international normalized ratio; PT, prothrombin time.
Fig. 3.

CT scan showing an incidental finding of a nonocclusive portal vein thrombosis (arrow). CT, computed tomography.
Patient was given intravenous ceftriaxone and underwent bedside ascitic fluid drainage. Results of the ascitic fluid showed, fluid culture no growth, nucleated cells 112, neutrophils 6%, and protein 18.
Stool analysis was negative for any bacterial growth or any presence of leukocytes. Her diarrhea eventually resolved in 4 to 5 days.
No anticoagulation was given as the presence of nonocclusive PVT is likely secondary to underlying cirrhosis.
Ultrasound breast was done which showed dominant solid mass lesion in the left breast 11 to 12 o'clock position with several other smaller satellite nodules in the left breast upper outer quadrant and enlarged axillary lymph nodes. Mammography was subsequently done which showed findings that are highly worrisome for a left breast lower inner quadrant malignancy with nodal disease to the left axilla. Patient was referred to the general surgery breast team and bedside core biopsy of left breast mass and fine-needle aspiration biopsy of left axillary lymph node showed invasive ductal carcinoma. The patient subsequently underwent left simple mastectomy with axillary clearance.
Progress
Patient underwent peritoneal drainage and was given antibiotics. No anticoagulation was given due to low platelet count. After 11 months, an ultrasound Doppler of the hepatobiliary system revealed no evidence of vascular thrombosis (Fig. 4).
Fig. 4.
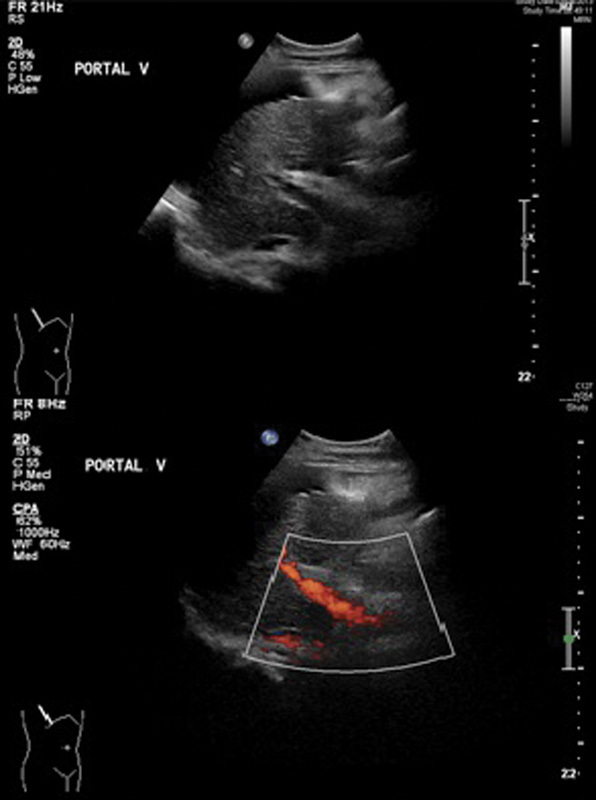
US HBS Doppler showing resolution of the portal vein thrombus. US HBS, ultrasound hepatobiliary system.
Discussion
PVT can occur in both cirrhotic and noncirrhotic patients and it can be an acute or a chronic episode. PVT in noncirrhotics can be due to intra-abdominal inflammatory lesions, intra-abdominal malignancy, or any injury to the portal venous system. Its incidence in patients without cirrhosis is not well described in the literature, but accounts for approximately 5 to 10% of all cases of portal hypertension in the Western hemisphere.
In cirrhotics, it has been well established that the prevalence of PVT increases with the severity of the cirrhosis. In those with well-compensated cirrhosis, the incidence of thrombosis reportedly varies between 0.6 and 16%. The incidence is higher in patients with advanced hepatic dysfunction, particularly those with hepatocellular cancer, in whom it reaches approximately 35%.2
Most of the time, noncirrhotic patients noted to have PVT without any bleeding risk factors are better managed with anticoagulation. Limited data are available for the management of PVT in cirrhotic patients.
Transient PVT has been reported in 23% of patients with acute pancreatitis and 57% in those with pancreatic necrosis.
Spontaneous recanalization (in 16.7% of patients) without treatment has also been documented. It has been said in multiple literature that, frequently, spontaneous PVT resolution is associated with a self-limiting underlying pathology or minimal thrombus extension.3
Conclusion
The decision to anticoagulate a patient with PVT depends on several factors. Spontaneous resolution is possible, as seen in the two cases, especially in setting of intra-abdominal infection treated with antibiotics. It is wise to hold off anticoagulation in a setting of intra-abdominal infection and PVT. Anticoagulation benefits versus risks should be considered. Anticoagulation is useful if there are worsening of symptoms or extension of thrombus in a setting where the bleeding risk is low.
References
- 1.DeLeve L D Valla D C Garcia-Tsao G; American Association for the Study Liver Diseases. Vascular disorders of the liver Hepatology 20094951729–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sameer P, Riddhi S, Prashant K. Review article: portal vein thrombosis. Am J Med. 2010;123(2):111–119. doi: 10.1016/j.amjmed.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Chawla Y, Duseja A, Dhiman R K. Review article: the modern management of portal vein thrombosis. Aliment Pharmacol Ther. 2009;30(9):881–894. doi: 10.1111/j.1365-2036.2009.04116.x. [DOI] [PubMed] [Google Scholar]


