Abstract
Hepatitis B virus (HBV) and hepatitis C virus (HCV) are hepatotropic viruses that establish chronic persistent infection by effectively escaping the host immune response and can cause immune-mediated liver injury. It has recently become apparent that regulatory T (Treg) cells, specifically CD4+CD25+Foxp3+ Treg cells, modulate viral diseases by suppressing antiviral immune responses and regulating inflammatory host injury. The roles of Treg cells in HBV and HCV infections range from suppressing antiviral T cell responses to protecting the liver from immune-mediated damage. This review describes Treg cells and subpopulations and focuses on the roles of these cells in HBV and HCV infections.
Keywords: Regulatory T cell, Hepatitis B virus, Hepatitis C virus
INTRODUCTION
Hepatitis B virus (HBV) is a member of the family Hepadnaviridae, whereas hepatitis C virus (HCV) is a member of the family Flaviviridae. Both HBV and HCV are hepatotropic viruses that cause liver inflammation (1,2,3). These viruses can establish chronic persistent infections that are accompanied by immune-mediated liver injury in the infected host. The infection evolves to chronic persistent infection in more than 70% of HCV-infected adults and approximately 90% of HBV-infected neonates due to vertical transmission (4). Infected patients have a high risk of developing liver cirrhosis and hepatocellular carcinoma once a chronic persistent infection is established by either HBV or HCV (5).
It has been demonstrated that virus-specific T cell responses are critical for the control of virus during HBV or HCV infection (6). In particular, adequate T cell responses are essential for spontaneous resolution of acute HBV or HCV infection and to prevent chronic persistent infection (3,7). Indeed, depletion of either CD4+ or CD8+ T cells disturbs viral clearance in challenge experiments with HBV or HCV in chimpanzees (8,9,10). However, T cells also contribute to liver injury during HBV and HCV infection. In particular, the finding that intrahepatic infiltration of T cells coincides with the increase of serum alanine aminotransferase (ALT) levels during acute HBV or HCV infection supports the important role of T cells in liver injury (4,7,11). However, the exact mechanism of T cell-mediated liver injury has not been elucidated.
CD4+CD25+Foxp3+ regulatory T (Treg) cells constitute a specialized T cell population that suppresses the activation, proliferation, differentiation, and effector functions of many types of immune cells, including T cells, B cells, NK cells, and dendritic cells (12,13,14,15). Treg cells play an important role in the maintenance of immunologic tolerance by suppressing autoreactive T cells. In addition, Treg cells control excessive immune activation after infection with various pathogens. Indeed, Treg cells play an important role in the modulation of antiviral T cell responses and immune-mediated host injury in the acute and chronic phases of viral infection (16,17,18). This review summarizes the current knowledge on Treg cells and their subpopulations and describes their role in HBV and HCV infections.
CD4+CD25+FOXP3+ TREG CELLS AND SUBPOPULATIONS
Although the concept of immune-suppressing T cell subsets was introduced in 1985 on the basis of their critical role in preventing autoimmunity (19), research on this T cell subset was hampered by the lack of a defining marker. In 1995, Sakaguchi et al. described a Treg population that constitutively expressed the interleukin 2 receptor α-chain (CD25) (20). In that study, the adoptive transfer of lymphocytes depleted of CD4+CD25+ T cells into athymic mice induced the development of autoimmune diseases. Interestingly, reconstitution with CD4+CD25+ T cells prevented autoimmune progression in these mice, suggesting a role for CD4+CD25+ T cells in the control of self-tolerance. CD4+CD25+ T cells in humans were found to have a similar function. Foxp3 was subsequently identified as the master regulator that determines the phenotype and function of CD4+CD25+ Treg cells (21).
Treg cells are classified based on their mechanism of development. CD4+CD25+Foxp3+ Treg cells are divided into natural Treg (nTreg) cells or thymus-derived Treg cells and induced Treg (iTreg) cells or peripherally derived Treg cells (22,23). nTreg cells develop during the process of T cell maturation in the thymus under T cell receptor engagement with self-antigens. nTreg cells suppress the activation and proliferation of T cells through contact-dependent mechanisms and have a key role in the maintenance of self-tolerance (24). Conversely, iTreg cells are generated de novo from conventional mature CD4+ T cells in the periphery in response to TGF-β and continuous exposure to low-dose antigen or systemic antigen (24,25,26,27). In addition to CD4+CD25+Foxp3+ Treg cells, CD4+ T cells producing IL-10 (Tr1) or TGF-β (Th3) and CD4+FoxA1+ T cells are considered regulatory cells (28,29). Furthermore, CD8+ Treg cells have been described in both humans and mice (30,31).
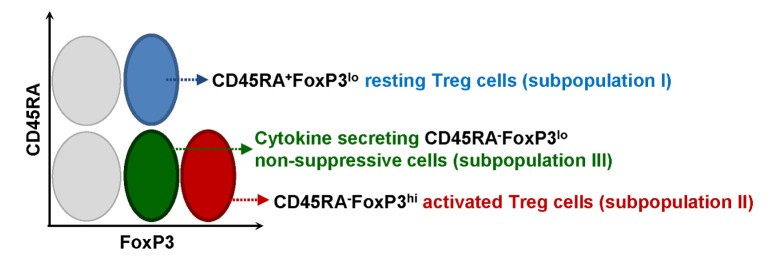
In humans, Miyara et al. described three distinct subpopulations of CD4+CD25+Foxp3+ Treg cells that could be classified into the following populations based on their expression levels of CD45RA and Foxp3: CD45RA+Foxp3low resting Treg cells (subpopulation I), CD45RA−Foxp3high activated Treg cells (subpopulation II), and CD45RA−Foxp3low cytokine-secreting non-suppressive cells (subpopulation III) (Fig. 1) (32). A recent study has suggested CD15s as a new marker in the detailed analysis of Treg cell subpopulations. CD15shigh Treg cells are activated and terminally differentiated; thus, these cells are the most suppressive type of Foxp3+ effector Treg cells (33). A recent study showed that the frequency of CD45RA–Foxp3high activated Treg cells was increased in patients with chronic active hepatitis B and acute-on-chronic liver failure and correlated with HBV DNA titer (34). In addition, the frequency of CD45RA−Foxp3low cytokine-secreting non-suppressive cells was increased in patients with acute-on-chronic liver failure and correlated with severe liver injury (34). These data indicate that analyses of the Treg cell subpopulation better delineate disease status than analyses of the total Treg cell population.
Figure 1. The subpopulation of human Treg cells. Three distinct subpopulations of human Treg cells are defined based on the expression level of CD45RA and Foxp3 as follows: CD45RA+Foxp3low resting Treg cells (subpopulation I), CD45RA−Foxp3high activated Treg cells (subpopulation II), and CD45RA−Foxp3low cytokine-secreting non-suppressive cells (subpopulation III) (32).
TREG CELLS IN VIRAL INFECTION
Treg cells play a crucial role in suppressing immune responses to self-antigens and in controlling autoimmune diseases. However, Treg cells also modulate immune responses to infectious pathogens, including bacteria, viruses, parasites, and fungi (35).
It has been shown that Treg cells regulate effector T cell responses against viruses such as herpes simplex virus (HSV), human immunodeficiency virus (HIV), and simian immunodeficiency virus (SIV) (17,36,37). Effective virus-specific T cell responses are critical for eliminating the virus. However, several viruses can escape the T cell response and promote viral persistence. Treg cells play a role in the suppression of antiviral T cell responses during this process and aid the establishment of viral persistence. In viral infection, Treg cells also contribute to host protection by preventing excessive immunopathological host damage caused by sustained immune activation and inflammation (38,39). For example, the role of Treg cells was clearly described in a murine model of corneal HSV infection (16). In this study, depletion of Treg cells prior to HSV challenge resulted in more severe eye inflammation by enhanced effector T cell infiltration. Furthermore, adoptive transfer of Treg cells reduced the severity of eye inflammation, indicating that Treg cells play a beneficial role by suppressing immunopathology and inflammation during viral infection.
TREG CELLS IN HBV INFECTION
Most studies of Treg cells in HBV infection have focused on the chronic phase of the infection, and it remains controversial whether the circulating CD4+CD25+ Treg cell population is expanded in patients with chronic HBV infection (40). Several studies have found a higher frequency of CD4+CD25+ Treg cells in HBV-infected individuals than in spontaneously recovered individuals or healthy controls (41,42) although another study reported similar Treg cell frequencies in patients with chronic HBV infection and healthy controls (43). One study analyzed Treg cells in detail at each stage of HBV infection, including the acute, chronic, and chronic severe hepatitis B stages, and the patients with chronic severe hepatitis B showed a significantly higher frequency of circulating CD4+CD25+ Treg cells than those with chronic mild hepatitis B or acute hepatitis B (44). Furthermore, the patients with chronic severe hepatitis B also showed more CD4+CD25+Foxp3+ Treg cells in the liver (44). Interestingly, the frequency of circulating Treg cells was positively correlated with the serum HBV load in patients with chronic hepatitis B. This result suggests that the expanded Treg cell population suppresses antiviral immune responses during chronic HBV infection (44,45).
The mechanisms underlying the increase in Treg cell frequency in patients with chronic HBV infection have not been clearly elucidated. One hypothesis is that iTreg cells are induced by cytokines or continuous exposure to HBV antigens. A previous study proposed that TGF-β increases the frequency of Treg cells in patients with chronic HBV infection and that the serum TGF-β level is positively correlated with Treg cell frequency (46). TGF-β is known to promote the peripheral conversion of conventional CD4+ T cells to Treg cells (47). The major source of TGF-β in the liver is hepatic stellate cells (HSCs), which are activated during chronic inflammation (48). Therefore, persistent infection with HBV might lead to TGF-β production from HSCs and contribute to the differentiation of conventional CD4+ T cells into iTreg cells.
TREG CELLS IN HCV INFECTION
There are limited data describing Treg cells in acute HCV infection, which commonly leads to persistent infection. One study compared circulating Treg cells in patients with acute HCV infection who progressed to chronic infection with those in patients who spontaneously resolved the infection (49). The results demonstrated that chronic progression was associated with long-term maintenance of Treg cells, whereas spontaneous recovery in the acute stage was associated with temporal loss of the suppressive function of Treg cells. This result suggests that Treg cells are key determinants of spontaneous resolution vs chronic progression of acute HCV infection.
Several studies of patients with chronic HCV infection revealed an increased frequency of CD4+CD25+ Treg cells in the peripheral blood compared with spontaneously resolving patients or healthy controls (50,51,52). Increased Treg cell frequencies in the liver have also been observed in chronically infected patients (53,54). However, it is uncertain whether these Treg cells are nTreg or iTreg cells induced by HCV antigens. Interestingly, Treg cells from chronically infected patients exhibit significantly higher suppressive activity against T cell proliferation and IFN-γ secretion (55). However, Treg cells from HCV-infected individuals inhibit CD8+ T cells in an antigen-nonspecific manner and suppress not only HCV-specific T cells but also influenza-, CMV-, and EBV-specific T cells (53,55).
Ward et al. studied the distribution of Treg cells within the HCV-infected liver by defining Treg cells as Foxp3+ and CD4+ cells, and the results showed a large amount of Treg cell infiltration in persistently HCV-infected patients than in healthy individuals. This finding suggests the involvement of CD4+Foxp3+ cells in intrahepatic immune regulation (54). Another studies have demonstrated that CD4+Foxp3+ Treg cells play a pivotal role in the protection against tissue damage by suppressing excessive HCV-induced immune activation (56). In this study, there was an increased number of Treg cells in chronic HCV-infected livers with limited fibrosis. In addition, HCV-specific CD4+CD25+ Treg cells from chronic HCV patients with normal serum ALT levels produced consistently higher amounts of TGF-β than Treg cells from chronic HCV patients with elevated ALT levels (57). These results suggest a role for these cells in controlling the chronic inflammatory response and hepatic damage.
One study showed that CD4+CD25+Foxp3+ Treg cells suppress not only IFN-γ production and the proliferation of HCV-specific T cells but also activation-induced cell death of HCV-specific T cells in HCV-exposed chimpanzees, including both hosts spontaneously recovered from HCV infection and hosts with chronic HCV infection (58). Therefore, it was suggested that Treg cells might control HCV-specific memory T cell responses by limiting their activation and preventing apoptosis in hosts who have recovered from HCV infection. A detailed analysis of the CD4+CD25+ Foxp3+ population in chimpanzees revealed that Treg cells from chronically infected and recovered chimpanzees displayed fewer T cell receptor excision circles than Treg cells from HCV-naïve chimpanzees, indicating that the cells underwent more proliferation as a result of HCV infection.
In addition to CD4+CD25+Foxp3+ Treg cells, CD8+ T cells with regulatory functions have been studied in patients with HCV infection. HCV-specific CD8+ T cells that produce IL-10 were identified in the livers of chronically infected patients by in situ immunostaining (59). Previous studies have demonstrated that IL-10-producing CD8+ T cells protect against liver cirrhosis by reducing hepatocellular apoptosis, indicating their role in decreasing liver damage (59). Accapezzato et al. showed that the anti-viral function of HCV-specific effector CD8+ T cells infiltrating the liver was not efficient in patients with chronic HCV infection because of the concomitant presence of virus-specific CD8+ T cells producing considerable amounts of IL-10 (60). This finding suggests that IL-10-producing CD8+ T cells contribute to viral persistence by controlling hepatic effector CD8+ T cell responses. TGF-β-secreting, HCV-specific CD8+ T cells were also identified in the blood of patients with chronic HCV infection (61). When TGF-β secretion was blocked, the peripheral HCV-specific T cell responses were enhanced despite the presence of HIV co-infection.
CONCLUSIONS
The function of Treg cells may be a double-edged sword in hepatitis viral infections. Although Treg cells suppress T cell responses directed against the hepatitis viruses, they also play a protective role by downregulating immune-mediated mechanisms of liver damage. However, it is unclear whether these different roles are attributed to identical Treg populations or distinct Treg subpopulations. In addition, it remains to be elucidated whether these two different roles are mediated by identical suppression mechanisms or by distinct mechanisms. A more detailed understanding of Treg cells in hepatitis viral infections will broaden our knowledge of immune responses and immunopathology in viral hepatitis and may provide new therapeutic targets for clinical applications.
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF-2014R1A1A3050293).
Abbreviations
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- Tregs
Regulatory T cells
Footnotes
CONFLICTS OF INTEREST: All authors have no conflicts of interest to declare.
References
- 1.Bowen DG, Walker CM. Adaptive immune responses in acute and chronic hepatitis C virus infection. Nature. 2005;436:946–952. doi: 10.1038/nature04079. [DOI] [PubMed] [Google Scholar]
- 2.Dustin LB, Rice CM. Flying under the radar: the immunobiology of hepatitis C. Annu Rev Immunol. 2007;25:71–99. doi: 10.1146/annurev.immunol.25.022106.141602. [DOI] [PubMed] [Google Scholar]
- 3.Wieland SF, Chisari FV. Stealth and cunning: hepatitis B and hepatitis C viruses. J Virol. 2005;79:9369–9380. doi: 10.1128/JVI.79.15.9369-9380.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guidotti LG, Chisari FV. Immunobiology and pathogenesis of viral hepatitis. Annu Rev Pathol. 2006;1:23–61. doi: 10.1146/annurev.pathol.1.110304.100230. [DOI] [PubMed] [Google Scholar]
- 5.Rehermann B, Bertoletti A. Immunological aspects of antiviral therapy of chronic hepatitis B virus and hepatitis C virus infections. Hepatology. 2015;61:712–721. doi: 10.1002/hep.27323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shin EC, Sung PS, Park SH. Immune responses and immunopathology in acute and chronic viral hepatitis. Nat Rev Immunol. 2016;16:509–523. doi: 10.1038/nri.2016.69. [DOI] [PubMed] [Google Scholar]
- 7.Rehermann B, Nascimbeni M. Immunology of hepatitis B virus and hepatitis C virus infection. Nat Rev Immunol. 2005;5:215–229. doi: 10.1038/nri1573. [DOI] [PubMed] [Google Scholar]
- 8.Grakoui A, Shoukry NH, Woollard DJ, Han JH, Hanson HL, Ghrayeb J, Murthy KK, Rice CM, Walker CM. HCV persistence and immune evasion in the absence of memory T cell help. Science. 2003;302:659–662. doi: 10.1126/science.1088774. [DOI] [PubMed] [Google Scholar]
- 9.Shoukry NH, Grakoui A, Houghton M, Chien DY, Ghrayeb J, Reimann KA, Walker CM. Memory CD8+ T cells are required for protection from persistent hepatitis C virus infection. J Exp Med. 2003;197:1645–1655. doi: 10.1084/jem.20030239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thimme R, Wieland S, Steiger C, Ghrayeb J, Reimann KA, Purcell RH, Chisari FV. CD8(+) T cells mediate viral clearance and disease pathogenesis during acute hepatitis B virus infection. J Virol. 2003;77:68–76. doi: 10.1128/JVI.77.1.68-76.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park SH, Rehermann B. Immune responses to HCV and other hepatitis viruses. Immunity. 2014;40:13–24. doi: 10.1016/j.immuni.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shevach EM, DiPaolo RA, Andersson J, Zhao DM, Stephens GL, Thornton AM. The lifestyle of naturally occurring CD4+ CD25+ Foxp3+ regulatory T cells. Immunol Rev. 2006;212:60–73. doi: 10.1111/j.0105-2896.2006.00415.x. [DOI] [PubMed] [Google Scholar]
- 13.Zhao DM, Thornton AM, DiPaolo RJ, Shevach EM. Activated CD4+CD25+ T cells selectively kill B lymphocytes. Blood. 2006;107:3925–3932. doi: 10.1182/blood-2005-11-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghiringhelli F, Menard C, Martin F, Zitvogel L. The role of regulatory T cells in the control of natural killer cells: relevance during tumor progression. Immunol Rev. 2006;214:229–238. doi: 10.1111/j.1600-065X.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 15.Mahnke K, Enk AH. Dendritic cells: key cells for the induction of regulatory T cells? Curr Top Microbiol Immunol. 2005;293:133–150. doi: 10.1007/3-540-27702-1_7. [DOI] [PubMed] [Google Scholar]
- 16.Suvas S, Azkur AK, Kim BS, Kumaraguru U, Rouse BT. CD4+CD25+ regulatory T cells control the severity of viral immunoinflammatory lesions. J Immunol. 2004;172:4123–4132. doi: 10.4049/jimmunol.172.7.4123. [DOI] [PubMed] [Google Scholar]
- 17.Suvas S, Kumaraguru U, Pack CD, Lee S, Rouse BT. CD4+CD25+ T cells regulate virus-specific primary and memory CD8+ T cell responses. J Exp Med. 2003;198:889–901. doi: 10.1084/jem.20030171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi YS, Lee J, Lee HW, Chang DY, Sung PS, Jung MK, Park JY, Kim JK, Lee JI, Park H, Cheong JY, Suh KS, Kim HJ, Lee JS, Kim KA, Shin EC. Liver injury in acute hepatitis A is associated with decreased frequency of regulatory T cells caused by Fas-mediated apoptosis. Gut. 2015;64:1303–1313. doi: 10.1136/gutjnl-2013-306213. [DOI] [PubMed] [Google Scholar]
- 19.Sakaguchi S, Fukuma K, Kuribayashi K, Masuda T. Organ-specific autoimmune diseases induced in mice by elimination of T cell subset. I. Evidence for the active participation of T cells in natural self-tolerance; deficit of a T cell subset as a possible cause of autoimmune disease. J Exp Med. 1985;161:72–87. doi: 10.1084/jem.161.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 21.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 22.Bluestone JA, Abbas AK. Natural versus adaptive regulatory T cells. Nat Rev Immunol. 2003;3:253–257. doi: 10.1038/nri1032. [DOI] [PubMed] [Google Scholar]
- 23.Abbas AK, Benoist C, Bluestone JA, Campbell DJ, Ghosh S, Hori S, Jiang S, Kuchroo VK, Mathis D, Roncarolo MG, Rudensky A, Sakaguchi S, Shevach EM, Vignali DA, Ziegler SF. Regulatory T cells: recommendations to simplify the nomenclature. Nat Immunol. 2013;14:307–308. doi: 10.1038/ni.2554. [DOI] [PubMed] [Google Scholar]
- 24.Curotto de Lafaille MA, Lafaille JJ. Natural and adaptive foxp3+ regulatory T cells: more of the same or a division of labor? Immunity. 2009;30:626–635. doi: 10.1016/j.immuni.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Chen W, Jin W, Hardegen N, Lei KJ, Li L, Marinos N, McGrady G, Wahl SM. Conversion of peripheral CD4+CD25− naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamagiwa S, Gray JD, Hashimoto S, Horwitz DA. A role for TGF-beta in the generation and expansion of CD4+CD25+ regulatory T cells from human peripheral blood. J Immunol. 2001;166:7282–7289. doi: 10.4049/jimmunol.166.12.7282. [DOI] [PubMed] [Google Scholar]
- 27.Kretschmer K, Apostolou I, Hawiger D, Khazaie K, Nussenzweig MC, von BH. Inducing and expanding regulatory T cell populations by foreign antigen. Nat Immunol. 2005;6:1219–1227. doi: 10.1038/ni1265. [DOI] [PubMed] [Google Scholar]
- 28.Shevach EM. From vanilla to 28 flavors: multiple varieties of T regulatory cells. Immunity. 2006;25:195–201. doi: 10.1016/j.immuni.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Weiner HL. Induction and mechanism of action of transforming growth factor-beta-secreting Th3 regulatory cells. Immunol Rev. 2001;182:207–214. doi: 10.1034/j.1600-065x.2001.1820117.x. [DOI] [PubMed] [Google Scholar]
- 30.Billerbeck E, Blum HE, Thimme R. Parallel expansion of human virus-specific FoxP3- effector memory and de novo-generated FoxP3+ regulatory CD8+ T cells upon antigen recognition in vitro. J Immunol. 2007;179:1039–1048. doi: 10.4049/jimmunol.179.2.1039. [DOI] [PubMed] [Google Scholar]
- 31.Endharti AT, Rifa'I M, Shi Z, Fukuoka Y, Nakahara Y, Kawamoto Y, Takeda K, Isobe K, Suzuki H. Cutting edge: CD8+CD122+ regulatory T cells produce IL-10 to suppress IFN-gamma production and proliferation of CD8+ T cells. J Immunol. 2005;175:7093–7097. doi: 10.4049/jimmunol.175.11.7093. [DOI] [PubMed] [Google Scholar]
- 32.Miyara M, Yoshioka Y, Kitoh A, Shima T, Wing K, Niwa A, Parizot C, Taflin C, Heike T, Valeyre D, Mathian A, Nakahata T, Yamaguchi T, Nomura T, Ono M, Amoura Z, Gorochov G, Sakaguchi S. Functional delineation and differentiation dynamics of human CD4+ T cells expressing the FoxP3 transcription factor. Immunity. 2009;30:899–911. doi: 10.1016/j.immuni.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 33.Miyara M, Chader D, Sage E, Sugiyama D, Nishikawa H, Bouvry D, Claer L, Hingorani R, Balderas R, Rohrer J, Warner N, Chapelier A, Valeyre D, Kannagi R, Sakaguchi S, Amoura Z, Gorochov G. Sialyl Lewis x (CD15s) identifies highly differentiated and most suppressive FOXP3high regulatory T cells in humans. Proc Natl Acad Sci U S A. 2015;112:7225–7230. doi: 10.1073/pnas.1508224112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang M, Zhou J, Zhao T, Huang G, Tan Y, Tan S, Fu X, Niu W, Meng G, Chen X, Shang X, Liu D, Ni B, Wang L, Wu Y. Dissection of a circulating and intrahepatic CD4(+)Foxp3(+) T-cell subpopulation in chronic hepatitis B virus (HBV) infection: a highly informative strategy for distinguishing chronic HBV infection states. J Infect Dis. 2012;205:1111–1120. doi: 10.1093/infdis/jis011. [DOI] [PubMed] [Google Scholar]
- 35.Yamaguchi T, Wing JB, Sakaguchi S. Two modes of immune suppression by Foxp3(+) regulatory T cells under inflammatory or non-inflammatory conditions. Semin Immunol. 2011;23:424–430. doi: 10.1016/j.smim.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Benito JM, Lopez M, Soriano V. The role of CD8+ T-cell response in HIV infection. AIDS Rev. 2004;6:79–88. [PubMed] [Google Scholar]
- 37.Goulder PJ, Watkins DI. HIV and SIV CTL escape: implications for vaccine design. Nat Rev Immunol. 2004;4:630–640. doi: 10.1038/nri1417. [DOI] [PubMed] [Google Scholar]
- 38.Belkaid Y, Rouse BT. Natural regulatory T cells in infectious disease. Nat Immunol. 2005;6:353–360. doi: 10.1038/ni1181. [DOI] [PubMed] [Google Scholar]
- 39.Mills KH. Regulatory T cells: friend or foe in immunity to infection? Nat Rev Immunol. 2004;4:841–855. doi: 10.1038/nri1485. [DOI] [PubMed] [Google Scholar]
- 40.Manigold T, Racanelli V. T-cell regulation by CD4 regulatory T cells during hepatitis B and C virus infections: facts and controversies. Lancet Infect Dis. 2007;7:804–813. doi: 10.1016/S1473-3099(07)70289-X. [DOI] [PubMed] [Google Scholar]
- 41.TrehanPati N, Kotillil S, Hissar SS, Shrivastava S, Khanam A, Sukriti S, Mishra SK, Sarin SK. Circulating Tregs correlate with viral load reduction in chronic HBV-treated patients with tenofovir disoproxil fumarate. J Clin Immunol. 2011;31:509–520. doi: 10.1007/s10875-011-9509-7. [DOI] [PubMed] [Google Scholar]
- 42.Stoop JN, van der Molen RG, Baan CC, van der Laan LJ, Kuipers EJ, Kusters JG, Janssen HL. Regulatory T cells contribute to the impaired immune response in patients with chronic hepatitis B virus infection. Hepatology. 2005;41:771–778. doi: 10.1002/hep.20649. [DOI] [PubMed] [Google Scholar]
- 43.Franzese O, Kennedy PT, Gehring AJ, Gotto J, Williams R, Maini MK, Bertoletti A. Modulation of the CD8+-T-cell response by CD4+ CD25+ regulatory T cells in patients with hepatitis B virus infection. J Virol. 2005;79:3322–3328. doi: 10.1128/JVI.79.6.3322-3328.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu D, Fu J, Jin L, Zhang H, Zhou C, Zou Z, Zhao JM, Zhang B, Shi M, Ding X, Tang Z, Fu YX, Wang FS. Circulating and liver resident CD4+CD25+ regulatory T cells actively influence the antiviral immune response and disease progression in patients with hepatitis B. J Immunol. 2006;177:739–747. doi: 10.4049/jimmunol.177.1.739. [DOI] [PubMed] [Google Scholar]
- 45.Stoop JN, van der Molen RG, Kuipers EJ, Kusters JG, Janssen HL. Inhibition of viral replication reduces regulatory T cells and enhances the antiviral immune response in chronic hepatitis B. Virology. 2007;361:141–148. doi: 10.1016/j.virol.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 46.Yang G, Liu A, Xie Q, Guo TB, Wan B, Zhou B, Zhang JZ. Association of CD4+CD25+Foxp3+ regulatory T cells with chronic activity and viral clearance in patients with hepatitis B. Int Immunol. 2007;19:133–140. doi: 10.1093/intimm/dxl130. [DOI] [PubMed] [Google Scholar]
- 47.Fantini MC, Becker C, Monteleone G, Pallone F, Galle PR, Neurath MF. Cutting edge: TGF-beta induces a regulatory phenotype in CD4+CD25− T cells through Foxp3 induction and down-regulation of Smad7. J Immunol. 2004;172:5149–5153. doi: 10.4049/jimmunol.172.9.5149. [DOI] [PubMed] [Google Scholar]
- 48.Ichikawa S, Mucida D, Tyznik AJ, Kronenberg M, Cheroutre H. Hepatic stellate cells function as regulatory bystanders. J Immunol. 2011;186:5549–5555. doi: 10.4049/jimmunol.1003917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smyk-Pearson S, Golden-Mason L, Klarquist J, Burton JR, Jr, Tester IA, Wang CC, Culbertson N, Vandenbark AA, Rosen HR. Functional suppression by FoxP3+CD4+CD25(high) regulatory T cells during acute hepatitis C virus infection. J Infect Dis. 2008;197:46–57. doi: 10.1086/523651. [DOI] [PubMed] [Google Scholar]
- 50.Ebinuma H, Nakamoto N, Li Y, Price DA, Gostick E, Levine BL, Tobias J, Kwok WW, Chang KM. Identification and in vitro expansion of functional antigen-specific CD25+ FoxP3+ regulatory T cells in hepatitis C virus infection. J Virol. 2008;82:5043–5053. doi: 10.1128/JVI.01548-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sugimoto K, Ikeda F, Stadanlick J, Nunes FA, Alter HJ, Chang KM. Suppression of HCV-specific T cells without differential hierarchy demonstrated ex vivo in persistent HCV infection. Hepatology. 2003;38:1437–1448. doi: 10.1016/j.hep.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 52.Li S, Gowans EJ, Chougnet C, Plebanski M, Dittmer U. Natural regulatory T cells and persistent viral infection. J Virol. 2008;82:21–30. doi: 10.1128/JVI.01768-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rushbrook SM, Ward SM, Unitt E, Vowler SL, Lucas M, Klenerman P, Alexander GJ. Regulatory T cells suppress in vitro proliferation of virus-specific CD8+ T cells during persistent hepatitis C virus infection. J Virol. 2005;79:7852–7859. doi: 10.1128/JVI.79.12.7852-7859.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ward SM, Fox BC, Brown PJ, Worthington J, Fox SB, Chapman RW, Fleming KA, Banham AH, Klenerman P. Quantification and localisation of FOXP3+ T lymphocytes and relation to hepatic inflammation during chronic HCV infection. J Hepatol. 2007;47:316–324. doi: 10.1016/j.jhep.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 55.Boettler T, Spangenberg HC, Neumann-Haefelin C, Panther E, Urbani S, Ferrari C, Blum HE, von WF, Thimme R. T cells with a CD4+CD25+ regulatory phenotype suppress in vitro proliferation of virus-specific CD8+ T cells during chronic hepatitis C virus infection. J Virol. 2005;79:7860–7867. doi: 10.1128/JVI.79.12.7860-7867.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Claassen MA, de Knegt RJ, Tilanus HW, Janssen HL, Boonstra A. Abundant numbers of regulatory T cells localize to the liver of chronic hepatitis C infected patients and limit the extent of fibrosis. J Hepatol. 2010;52:315–321. doi: 10.1016/j.jhep.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 57.Bolacchi F, Sinistro A, Ciaprini C, Demin F, Capozzi M, Carducci FC, Drapeau CM, Rocchi G, Bergamini A. Increased hepatitis C virus (HCV)-specific CD4+CD25+ regulatory T lymphocytes and reduced HCV-specific CD4+ T cell response in HCV-infected patients with normal versus abnormal alanine aminotransferase levels. Clin Exp Immunol. 2006;144:188–196. doi: 10.1111/j.1365-2249.2006.03048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Manigold T, Shin EC, Mizukoshi E, Mihalik K, Murthy KK, Rice CM, Piccirillo CA, Rehermann B. Foxp3+CD4+CD25+ T cells control virus-specific memory T cells in chimpanzees that recovered from hepatitis C. Blood. 2006;107:4424–4432. doi: 10.1182/blood-2005-09-3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abel M, Sene D, Pol S, Bourliere M, Poynard T, Charlotte F, Cacoub P, Caillat-Zucman S. Intrahepatic virus-specific IL-10-producing CD8 T cells prevent liver damage during chronic hepatitis C virus infection. Hepatology. 2006;44:1607–1616. doi: 10.1002/hep.21438. [DOI] [PubMed] [Google Scholar]
- 60.Accapezzato D, Francavilla V, Paroli M, Casciaro M, Chircu LV, Cividini A, Abrignani S, Mondelli MU, Barnaba V. Hepatic expansion of a virus-specific regulatory CD8(+) T cell population in chronic hepatitis C virus infection. J Clin Invest. 2004;113:963–972. doi: 10.1172/JCI20515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alatrakchi N, Graham CS, van d, Sherman VKE, Exley MA, Koziel MJ. Hepatitis C virus (HCV)-specific CD8+ cells produce transforming growth factor beta that can suppress HCV-specific T-cell responses. J Virol. 2007;81:5882–5892. doi: 10.1128/JVI.02202-06. [DOI] [PMC free article] [PubMed] [Google Scholar]