Abstract
Objective
To examine neuromuscular risk factors for the incidence and progression of knee instability symptoms in older adults with or at high risk for knee osteoarthritis.
Methods
At the 60-month clinic visit of the Multicenter Osteoarthritis Study participants underwent evaluation of quantitative vibratory sense at the knee and isokinetic quadriceps muscle strength. Participants were also asked about knee buckling and sensations of knee shifting or slipping without buckling in the past 3 months at this 60 month visit and then asked the same questions at the 72 and 84 month follow up visits. We performed a person-based analyses using Poisson regression with robust error variance to estimate adjusted relative risk for the association of vibratory sense and muscle strength with the incidence and worsening of knee slipping/shifting, buckling, and overall knee instability symptoms (either buckling or knee shifting/slipping), with adjustment for relevant confounders.
Results
1803 participants (61% women) were included. Approximately one-third reported incident or worsening of instability symptoms over the study period. Adjusting for relevant confounders, better vibratory acuity (adjusted RR:0.78, 95 %CI: 0.56,1.09), p=0.020 for trend) and greater quadriceps strength (adjusted RR:0.53, 95%CI:0.38,0.75, p<0.001) protected against incident knee instability symptoms. Greater quadriceps strength (adjusted RR:0.73, 95%CI:0.58,0.92, p=0.008) also protected against worsening of knee instability symptoms.
Conclusion
Vibratory acuity and quadriceps muscle strength are important predictors of knee instability incidence and worsening over 2 years. These neuromuscular factors are potentially modifiable and should be considered in interventional studies of instability in persons with or at risk for knee osteoarthritis.
Introduction
Knee instability symptoms are extremely prevalent in osteoarthritis (OA), self-reported in up to 65% of participants in some studies and significantly associated with activity limitations and worse physical function(1, 2). Knee instability frequently manifests as buckling, defined as the sudden loss of postural support from ‘giving way’ of the knee due to mechanical failure during weight bearing activities. Knee buckling may lead to increased falls in older adults with OA which may further result in early morbidity and mortality, a reduced quality of life, and early disability(3).
Due to its significant clinical implications in OA, several studies have searched for potential associations or risk factors for knee instability so that therapeutic interventions could be implemented to help improve these symptoms. Considering the importance of sensory and motor input for joint movement and function as well as previous studies that have shown the presence of neuromuscular deficits in OA, deficiencies in these factors may contribute to knee instability. Quadriceps muscle weakness is well recognized in OA and has been associated with knee instability in previous studies(4, 5). Proprioception, the sensation of movement or position in space, has been shown to be affected in knee OA; however, investigators have examined knee proprioception and knee laxity but were unable to find an association with knee instability(5). Another sensory measure, vibratory acuity, appears to travel through similar neurological pathways as proprioception, and has been shown to be altered in lower extremity OA(6, 7). Vibratory perception has also been associated with dynamic loading at the knee, thus supporting its potential mechanical role in knee OA pathogenesis (8); as of yet, its association with knee instability has not been investigated. Unfortunately, previous studies of instability have mostly been cross-sectional and therefore, have been unable to establish whether these risk factors preceded the occurrence of instability which would suggest they might be causally related. As a result, the etiology and pathogenesis of knee instability remain unclear; it is important to continue to identify risk factors for instability, particularly those that may be modifiable with interventions.
The use of varied reporting criteria for knee instability has made it difficult to synthesize data in the available literature(1, 2, 4). Persons with knee OA may not experience mechanical failure of the knee resulting in loss of postural support (knee buckling or giving way), however, they may experience less severe sensations of knee instability, such as slipping or shifting without the knee actually giving way(3). Studies have defined knee instability by self-report of either “knee buckling”, actual giving away of the knee and loss of postural support(4), or more broadly as either knee buckling, shifting or slipping (2, 5, 9). It is not clear if the sensation of shifting or slipping without buckling is a less severe or earlier manifestation of knee instability on a spectrum with buckling, or is a more unrelated outcome with different risk factors.
The goal of the current study was to evaluate the association of muscle strength (quadriceps) and sensory alterations (vibratory acuity), with the incidence and worsening of knee instability in a large cohort of participants with knee OA or at high risk of disease. Knee instability included both knee buckling as well as the sensation of knee slipping or shifting without buckling. However, knee buckling and sensation of knee slipping or shifting were analyzed separately as well as together to evaluate if the risk factors may be different for these conditions.
Methods
Population
The Multicenter Osteoarthritis Study (MOST) is a longitudinal study of people either with or at high risk of knee OA. Details of MOST have been published previously(10, 11). The MOST study protocol was approved by the Institutional Review Boards at the University of Alabama at Birmingham, the University of Iowa, the University of California, San Francisco, and Boston University Medical Center. In brief, MOST included community-dwelling participants between 50 and 79 years of age at baseline who lived in the areas surrounding Birmingham, Alabama, or Iowa City, Iowa. The definition of being at elevated risk for OA included age 50 or older, presence of knee symptoms on most days of the month, previous knee injury or surgery, or high body weight. Baseline examinations occurred between April 2003 and April 2005 and participants were followed at the 15, 30, 60, 72 and 84 months visits. We utilized data from participants who came for a 60 month clinic visit as the baseline for this inquiry, since that was the examination at which subjects were first asked about knee instability, and data from the 72 and 84 month visits for follow up evaluation of these outcomes. Those participants who did not come for the 60 month visit or did not have 72 and 84 month follow up information were excluded.
Exposures of interest (assessed at baseline, 60 months)
Quadriceps muscle strength
At the 60-month visit, participants underwent evaluation of isokinetic knee extensor strength. Quadriceps strength was evaluated as the maximum torque during active isokinetic extension using a Cybex 350 computerized dynamometer (HUMAC software version 4.3.2/Cybex 300 for Windows 98, Avocent, Huntsville, AL). Strength measurements were performed at 60 degrees/second with the chair back at 85 degrees. After 3 practice trials, 4 measurements were recorded at maximum effort and the highest torque measurement was recorded. Measurements (Newton meters (Nm)) were normalized to body size by dividing the maximum torque by BMI. Most participants had strength testing of one leg (right leg). In a small number of participants, quadriceps strength was measured of both legs. In the cases of bilateral evaluations, the lower strength measurement was taken for analyses.
Vibratory perception
Vibratory perception threshold (VPT) was evaluated using a biothesiometer (Bio-Medical Instrument Co., Newberry, Ohio) at the 60 month visit in accordance with previously published methods(6). The applicator tip of the instrument was placed on preselected anatomic bony prominences. In this study measurements from the tibial tuberosity were used. The voltage was initially set at “0” and then increased by 1 volt/second until the participant acknowledged sensation and this was defined as the VPT. Two sequential measurements were performed and if there was greater than 6 volts difference in these measurements, then 2 more trials were performed. The average of the two trials was recorded as the VPT. The mean VPT between the limbs was used for analyses.
Baseline covariates
Knee pain was assessed with the 5 item Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index (pain range 0 to 20) for pain over the past 30 days(12). Participants provided pain scores for each knee and the maximum score was used in the analyses. For other lower extremity joints, participants were asked about pain “on most days of the past 30 days” at both hips, ankles and feet (for the purposes of this study, knee pain was not included here) by referring to predefined locations on a distal lower extremity diagram, which yields a count of the number of locations (0–6). Radiographic knee OA severity was based on the Kellgren and Lawrence (KL) grade in the worse knee at 60 months, using previously described methods(13).
Knee Instability Symptoms: Buckling and Sensations of Shifting or Slipping without Buckling
To assess episodes of knee buckling or giving way (we use these two terms interchangeably), participants were asked “In the past 3 months, has either of your knees buckled or given way at least once?” We defined knee buckling as present if subjects answered ‘yes’ to this question on knee buckling. To assess whether participants experienced a sensation of knee shifting or slipping that did not involve the knee actually buckling, just after the question about knee buckling, we asked all participants “In the past 3 months, has either knee felt like it was shifting, slipping, or going to give way but didn’t actually do so?” We defined knee shifting/slipping as present in those who answered ‘yes’ to this question. A combined category of “knee instability” included both buckling and/or sensation of slipping or shifting without buckling. It was considered present in those that answered “yes” to at least one of these questions.
Frequency of symptoms was evaluated with the question “Counting all times and both knees, how many times in the past 3 months have your knees buckled?” The categories included: 1 time, 2 to 5 times, 6 to 10 times,11 to 24 times and more than 24 times. A similar question was asked about the sensation of slipping or shifting without buckling.
Primary outcomes (assessed at 60, 72, and 84 months)
Incident knee shifting/slipping without buckling
An individual was considered to have incident knee shifting/slipping without buckling if they answered “no” to both the questions about buckling and about shifting/slipping at 60 months and answered “yes” to shifting/slipping at 72 or 84 months.
Worsening (increased frequency) of sensations of knee slipping or shifting without buckling
Worsening in slipping or shifting was defined among subjects who did not report ceiling level (greater than 24 times) of this symptom at 60 months. Participants without this specific symptom at 60 months were considered as having frequency zero and eligible for worsening in frequency. Worsening in slipping or shifting frequency in past 3 months was defined as having occurred if a subject reported higher frequency at either 72 months or 84 months.
Incident knee buckling
An individual was considered to have incident buckling if they answered “no” to the question about buckling at 60 months, and answered “yes” to buckling at 72 or 84 months.
Worsening (increased frequency) of knee buckling
Worsening in buckling frequency was defined among subjects who did not report ceiling level (greater than 24 times) of buckling at 60 months. Participants without buckling at 60 months were considered as having frequency zero and eligible for worsening in frequency. Worsening in buckling frequency in past 3 months was defined as having occurred if a subject reported higher buckling frequency at either 72 months or 84 months.
Incident knee instability (buckling and/or shifting/slipping)
An individual was considered to have incident knee instability if they answered “no” to both the questions about buckling and about shifting/slipping at 60 months, and answered “yes” to either (or both) buckling or shifting/slipping without buckling at 72 or 84 months.
Worsening of knee instability
Worsening of knee instability was considered to be present if participants worsened in either (or both) buckling OR slipping/shifting frequency as defined above for “worsening of knee buckling” and “worsening of sensations of shifting or slipping without buckling”.
Statistical analyses
All analyses were performed using Statistical Analyses Systems (v9.2) software.
For all analyses, VPT and quadriceps muscle strength were categorized into sex-specific groups based on ±1 SD of the mean of the sample as “low”, “middle”, and “high”.
The primary analyses was a person-based analyses using Poisson regression with robust error variance to estimate adjusted relative risk for the association of VPT and muscle strength with knee buckling, sensation of slipping and shifting without buckling and overall knee instability incidence as well as worsening of each of these symptoms. Covariates that were adjusted for in the analyses included age, sex, BMI, race, KL grade, hip/ankle/foot pain and baseline WOMAC knee pain as well as the other exposure (VPT or strength). A test for trend also using Poisson regression was performed using the median VPT or strength in the three categories to evaluate for a dose-response relationship between exposure and knee instability outcomes. Sensitivity analyses for incident outcomes were performed using a knee-based model. Sensitivity analyses were also performed using maximum quadriceps strength (instead of minimum) when both knee data were available as well as using the “worse” VPT value of the two knee instead of mean value.
Results
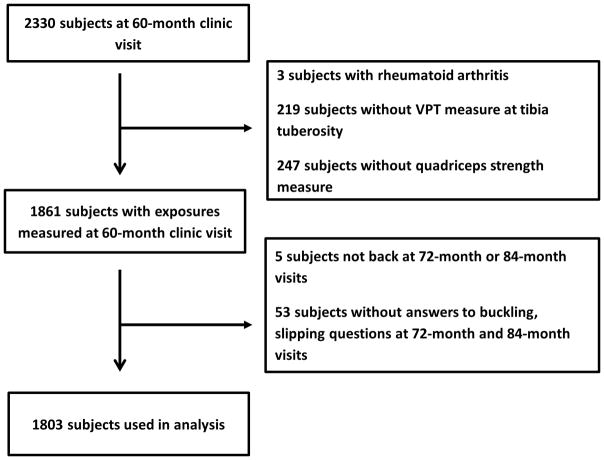
Baseline data and follow up data for the variables of interest were available for 1803 participants (Figure 1). General demographic data and baseline measures and frequency of risk factors and outcomes are summarized in Table 1 for study participants as well as those participants that were not included in the study due to missing data (n=507). Overall, 28% reported sensations of shifting or slipping, 16% of participants reported buckling, and 36% reported instability (buckling and/or slipping/shifting without buckling) in the past 3 months at the 60-month visit. Over the follow-up period 24% developed incident sensations of shifting or slipping, 20% incident buckling, and 32% developed incident instability. Similarly, 26% had worsening of sensations of shifting or slipping, 20% had worsening of buckling, and 36% had worsening of overall instability.
Figure 1.
Study participant flow chart
Table 1.
Characteristics of participants
| Participants in the study | Participants excluded | |
|---|---|---|
| Age (years±SD) | 67.6 (7.7) | 68.9 (8.1) |
| Gender, n female(%) | 1095(61%) | 314(60%) |
| Body Mass Index (kg/m2±SD) | 31±6 | 31±6 |
| Race, n Whites (%) | 1556(86%) | 407(77%) |
| Summary of WOMAC knee pain (mean±SD) | 5.6 (6.1) | 6.4 (6.7) |
| Number of painful joints in hips, ankles, feet (mean±SD) | 1.5 (1.7) | 1.6 (1.7) |
| Kellgren & Lawrence grade, n(%) | ||
| 0 | 517(30%) | 222(44%) |
| 1 | 287(16%) | 59(12%) |
| 2 | 359(21%) | 66(13%) |
| 3–4 | 584(33%) | 157(31%) |
| Worst corrected quadriceps strength (mean Nm/BMI±SD) | ||
| Men | 3.9 (1.4) | 3.4 (1.4) |
| Women | 2.3 (0.9) | 1.8 (0.8) |
| Average VPT at tibial tuberosity (mean volts±SD) | ||
| Men | 26.6 (11.9) | 28.5 (13.1) |
| Women | 20.3 (9.8) | 21.5 (10.8) |
| Prevalence with buckling in past 3 months, n(%) | 283(15.8%) | 104(20.2%) |
| Prevalence of slipping/shifting in past 3 months, n(%) | 509(28.3%) | 161(31.1%) |
| Prevalence of knee instability in past 3 months, n(%) | 652(36.3%) | 203(39.2%) |
| Frequency of buckling in past 3 months | ||
| 1 time | 57(3.2%) | 12(2.4%) |
| 2–5 times | 164(9.1%) | 65(12.8%) |
| 6–10 times | 43(2.4%) | 9(1.8%) |
| 11–24 times | 16(0.9%) | 3(0.6%) |
| More than 24 times | 3(0.2%) | 7(1.4%) |
| Frequency of slipping in past 3 months | ||
| 1 time | 1289(71.7%) | 357(68.9%) |
| 2–5 times | 509(28.3%) | 161(31.1%) |
| 6–10 times | 1344(75.4%) | 376(74.6%) |
| 11–24 times | 301(16.9%) | 80(15.9%) |
| More than 24 times | 138(7.7%) | 48(9.5%) |
| Incidence of buckling from 60 to 84 months, n(%) | 304(20.2%) | 72(20.5%) |
| Incidence of slipping/shifting from 60 to 84 months, n(%) | 258(24.1%) | 63(26.1%) |
| Incidence of knee instability from 60 to 84 months, n(%) | 345(31.8%) | 87(35.1%) |
| Worsening of buckling from 60 to 84 months, n(%) | 365(20.5%) | 94(22.1%) |
| Worsening of slipping/shifting from 60 to 84 months, n(%) | 436(26.3%) | 104(27.7%) |
| Worsening of knee instability from 60 to 84 months, n(%) | 651(36.1%) | 164(37.7%) |
Overall, there was some overlap/co-occurrence of slipping and shifting symptoms with buckling, but several participants reported only one type of symptom. Nearly half of participants experienced incident or progressive buckling without experiencing similar onset or progression of symptoms of slipping or shifting. For example, for those that had neither symptom at baseline, 41% those that developed incident buckling did so without experiencing symptoms of shifting or slipping. Further, 48% experienced progression of buckling without progression of slipping. Slipping or shifting symptoms appeared to more commonly occur alone, with 67% developing incident symptoms of slipping or shifting without experiencing incident buckling and 63% experiencing worsening symptoms without experiencing worsening buckling.
The primary results are summarized in Tables 2 through 4.
Table 2.
Association of vibratory acuity and quadriceps muscle strength with knee slipping/shifting symptoms
| INCIDENT KNEE SHIFTING/SLIPPING | WORSENING KNEE SHIFTING/SLIPPING | |||||
|---|---|---|---|---|---|---|
| Adjusted RR (95%CI) | p value | Adjusted RR (95%CI) | p value | |||
| Vibratory sense at tibial tuberosity* | Lower n=52/175 (29.7%) | 1.23 (0.94, 1.62) | 0.1323 | Lower n=89/276 (32.2%) | 1.13 (0.92, 1.39) | 0.247 |
| Middle n=180/758 (23.7%) | 1 | Middle n=299/1168 (25.6%) | 1 | |||
| Greater n=26/137 | 0.84 (0.57, 1.22) | 0.3522 | Greater n=48/213 (22.5%) | 0.91 (0.69, 1.20) | 0.504 | |
|
| ||||||
| p for linear trend | 0.064 | p for linear trend | 0.175 | |||
|
| ||||||
| Quadriceps muscle strength** | Lower n=39/128 (30.5%) | 0.83 (0.61, 1.14) | 0.2542 | Lower n=84/255 (32.9%) | 0.92 (0.74, 1.14) | 0.4431 |
| Middle n=195/728 (26.8%) | 1 | Middle n=311/1119 (27.8%) | 1 | |||
| Greater n=24/214 (11.2%) | 0.48 (0.32, 0.73) | <0.001 | Greater n=41/283 (14.5%) | 0.64 (0.47, 0.88) | 0.006 | |
|
| ||||||
| p for linear trend | <0.001 | p for linear trend | 0.047 | |||
Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and vibratory sense
Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and quadriceps strength
Table 4.
Association of vibratory acuity and quadriceps muscle strength with overall knee instability symptoms.
| INCIDENT KNEE INSTABILITY (BUCKLING AND/OR SLIPPING) | WORSENING KNEE INSTABILITY (BUCKLING AND/OR SLIPPING) | |||||
|---|---|---|---|---|---|---|
| Adjusted RR (95%CI) | p value | Adjusted RR (95%CI) | p value | |||
| Vibratory sense at tibial tuberosity* | Lower n=72/178 (40.4%) | 1.21 (0.97, 1.50) | 0.091 | Lower n=127/310 (41%) | 1.05 (0.89, 1.24) | 0.573 |
| Middle n=241/768 (31.4%) | 1 | Middle n=456/1261 (36.2%) | 1 | |||
| Greater n=32/138 (23.2%) | 0.78 (0.56, 1.09) | 0.141 | Greater n=68/231 (29.4%) | 0.81 (0.65, 1.01) | 0.061 | |
|
| ||||||
| p for linear trend | 0.020 | p for linear trend | 0.149 | |||
|
| ||||||
| Quadriceps muscle strength** | Lower n=59/131 (45%) | 1.01 (0.80, 1.28) | 0.913 | Lower n=134/291 (46%) | 1.01 (0.86, 1.18) | 0.923 |
| Middle n=253/739 (34.2%) | 1 | Middle n=451/1218 (37%) | 1 | |||
| Greater n=33/214 (15.4%) | 0.53 (0.38, 0.75) | <0.001 | Greater n=66/293 (22.5%) | 0.73 (0.58, 0.92) | 0.008 | |
|
| ||||||
| p for linear trend | <0.001 | p for linear trend | 0.010 | |||
Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and vibratory sense
Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and quadriceps strength
Sensations of shifting or slipping
For sensations of slipping and shifting alone, greater quadriceps strength was strongly associated both with a lower incidence of developing these symptoms during the follow up period (RR: 0.48 95% CI: 0.32, 0.73) and it protected against worsening of these symptoms (RR: 0.64, 95% CI: 0.47, 0.88) (Table 2). For vibratory acuity, there was no significant relationship with either incidence or worsening of these symptoms during the study period.
Buckling
For buckling alone, better vibratory acuity was associated with a decreased risk of incident buckling (RR: 0.67, 95%CI: 0.46, 0.98) as well as worsening of buckling symptoms over 24 months (RR: 0.65, 95% CI:0.47, 0.92)(Table 3). For quadriceps strength, there were significant linear trends for better strength to protect against incident (p=0.030) and worsening buckling (p=0.045) symptoms.
Table 3.
Association of vibratory acuity and quadriceps muscle strength with knee buckling symptoms
| INCIDENT KNEE BUCKLING | WORSENING KNEE BUCKLING | |||||
|---|---|---|---|---|---|---|
| Adjusted RR (95%CI) | p value | Adjusted RR (95%CI) | p value | |||
| Vibratory sense at tibial tuberosity* | Lower n=58/251 (23.1%) | 1.09 (0.82, 1.45) | 0.560 | Lower n=70/305 (23%) | 1.01 (0.78, 1.31) | 0.918 |
| Middle n=217/1065 (20.4%) | 1 | Middle n=260/1245 (20.9%) | 1 | |||
| Greater n=29/190 (15.3%) | 0.67 (0.46, 0.98) | 0.039 | Greater n=35/228 (15.4%) | 0.65 (0.47, 0.92) | 0.015 | |
|
| ||||||
| p for linear trend | 0.133 | p for linear trend | 0.219 | |||
|
| ||||||
| Quadriceps muscle strength** | Lower n=70/222 (31.5%) | 1.29 (1.00, 1.68) | 0.054 | Lower n=86/288 (29.9%) | 1.21 (0.95, 1.53) | 0.127 |
| Middle n=199/1020 (19.5%) | 1 | Middle n=240/1202(20%) | 1 | |||
| Greater n=35/264 (13.3%) | 0.86 (0.61, 1.21) | 0.381 | Greater n=39/288 (13.5%) | 0.85 (0.61, 1.18) | 0.324 | |
|
| ||||||
| p for linear trend | 0.030 | p for linear trend | 0.045 | |||
Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and vibratory sense ** Adjusted model includes age, sex, BMI, race, sum WOMAC knee pain, max KL grade, hip/ankle/foot pain, and quadriceps strength
Knee instability
For overall knee instability (either buckling or slipping and shifting), greater quadriceps strength was strongly protective against both incident (RR: 0.53, 95% CI: 0.38, 0.75) and worsening knee instability symptoms (RR: 0.73, 95% CI: 0.58, 0.92)(Table 4). There was a significant linear trend (p=0.020) for better vibratory acuity to protect against incident knee instability but no association with worsening knee instability symptoms during the study period.
Sensitivity analyses (results not shown)
Knee based analyses for incident outcomes showed similar results to the primary analyses. Similar results were also observed when performing sensitivity analyses using the highest strength measure of two knees or using the worst VPT measure of two knees.
Discussion
This study is unique in that it is a longitudinal evaluation of neuromuscular risk factors for incidence and worsening of knee instability symptoms and it evaluates knee instability as both a combination of knee buckling symptoms and sensations of slipping and shifting without buckling symptoms. It suggests that as quadriceps strength increases, the risk of buckling diminishes and also that better vibratory acuity protects against development and worsening of knee buckling.
Previous studies have shown that knee instability is prevalent in older adults. The prevalence varies depending on the population and definitions of knee instability. For example, in the general Framingham cohort, prevalence of buckling alone was 12% over a 3 month period (4) while in studies of persons with knee OA , knee instability prevalence is reported to be as high as 65%(1, 2, 5). The MOST cohort, evaluated in the current investigation is unique in that it includes older adults that have knee OA or are at high risk for knee OA. In light of these differences, prevalence numbers were in line with previous studies in the general population with 16% prevalence of buckling and 36% prevalence of overall knee instability over 3 months at the study baseline. Further it appears that in this cohort, development of instability symptoms in those that did not report them at baseline is common, with up to one-third of participants developing these symptoms or experiencing worsening of these symptoms over two years.
This study supports the role for quadriceps muscle strength in knee instability. In previous cross-sectional evaluations, quadriceps strength has been associated with knee buckling(4) and overall knee instability(5). In the current study, greater quadriceps strength was associated with decreased incidence and lower risk of worsening of knee instability symptoms. Furthermore, quadriceps strength appeared to have stronger associations with sensations of shifting and slipping without buckling than it did with actual buckling or giving way of the knee. The reasons for this are not clear. Muscles have been proposed to provide stability to the joint, however, the relationship of muscle function to joint stability may be complex. These results suggest that actual muscle strength may be an important factor. Nevertheless, muscle activation patterns and dynamic muscle function during ambulation may be additional factors that were not assessed in the current investigation. Muscle weakness has also been associated with poorer function and activity limitations(1), which may be related to knee instability and fear of falling (3). Thus, the current study’s results provide further support for the importance of muscle strengthening in a rehabilitation program for knee OA.
Sensory deficits including proprioceptive(14–16) and vibratory sense deficits(6) have been observed in OA. Proprioception in knee OA has been evaluated using various methods, most evaluating detection of movement with flexion and extension of the knee. Previous studies have reported a lack of association between proprioception measured in this manner and self-reported knee instability(5). Standard methods for testing proprioception in knee OA are subject to a variety of biases: they require movement of the arthritic knee and may therefore be confounded by disease severity and pain independent of any true lower extremity sensory deficits; they depend on patients’ reaction times, and may be confounded by delayed reflexes and participant comprehension, concentration, and memory. Vibratory perception travels through similar neurological pathways to proprioception and has been shown to be decreased in hip and knee OA. Vibratory perception is sensory measure that is commonly used to evaluate diabetic neuropathy(17, 18), and has been associated with neuropathic arthropathy(19, 20). Previous studies have shown generalized deficits at both upper and lower extremities in participants with lower extremity OA(6, 7) and suggested a mechanical role for vibratory acuity by demonstrating that worse vibratory perception was associated with higher dynamic joint loading in OA(8). In a study by Kavchak and colleagues, decreased vibratory acuity was associated with increased perceived knee instability during a functional task(9), supporting our results in this study. In the current investigation, better vibratory acuity had its strongest association with incidence and worsening of buckling symptoms alone rather than overall knee instability symptoms. The reasons for this are not clear. Nevertheless, the current study’s results support the potential mechanical implications of sensory deficits in OA.
The consequences of knee instability can be significant. Previous studies have shown that knee instability leads to loss of confidence, fear of falling and decreased function(1, 3, 4). Knee instability may also lead to falls and injuries(4). The current study has several clinical implications in regards to expanding our understanding of risk factors for knee instability and in designing and implementing future interventions for the management of these symptoms. Vibratory sense and muscle strength could both be considered important variables for neuromuscular control of the joint and therefore, it is not surprising that they were important risk factors for knee instability. We found that strength was more strongly associated with slipping and shifting without the knee giving way while vibratory acuity was more consistently associated with actual knee buckling. These slight variations in association may just be random, however, future studies may help clarify if there are underlying neuromechanical etiologies for these findings. It is not clear if these symptoms are on a spectrum of knee instability severity or whether they may be independent unrelated manifestations of instability with some overlapping risk factors. In this study, 40% of participants reported incident buckling without reporting previous slipping or shifting symptoms and without developing incident slipping symptoms, suggesting that not all people will experience slipping or shifting as a precedent to buckling symptoms.
Neuromuscular risk factors for knee instability may be modifiable. Quadriceps muscle strength is an established and modifiable risk factor for knee OA(21, 22) and now for knee instability as well. In a controlled trial of participants with knee instability, Knoop et al, randomized participants to receive knee stabilization training along with muscle strengthening versus muscle strengthening alone. Both groups demonstrated improvements in pain, function and knee instability(23).On the other hand, Fitzgerald et al. were not able to show improvements in self-reported knee instability in either group of their randomized controlled trial of exercise therapy(24). Others have shown that sensory deficits, in most cases proprioceptive acuity, may be altered with various exercise (25, 26) and kinesthetic interventions(27). However, it is not yet clear if vibratory deficits in OA are modifiable with interventions. More controlled trials with neuromuscular interventions in OA are necessary to evaluate potential improvements in knee instability.
In this study we performed a person based analyses, which we believe provides valuable information about the associations of interest. A limb does not function in isolation and therefore, overall neuromuscular health is likely a relevant and perhaps most appropriate measure to evaluate as any when asking the questions in this study. Studies have shown that sensory deficits in OA (both proprioception and vibratory sense) are likely generalized and affect both knees and even upper extremity sites. Thus, we averaged the VPT of both knees to provide an overall assessment of vibratory acuity in the participants. Similarly, muscle impairments in persons with knee OA have been shown not only to affect bilateral quadriceps, but other lower extremity muscle groups as well(28). In the MOST study, a majority of participants only had data on the right knee quadriceps for strength. However, the correlation of one limb’s quadriceps strength with contralateral limb strength was high (r=0.84) (which is only slightly lower than repeated strength assessment of the same limb). This suggests that for quadriceps strength measurements, when you know the measurement in one limb, you can estimate with considerable accuracy the value of the contralateral limb. We did perform sensitivity analyses looking at maximum quadriceps strength amongst two knees as well as looking at the worst vibratory sense measure amongst the knees and results were similar. Finally, although we could perform an incident analyses based on knee (primarily right knee only), we did not have information separated by side for worsening in frequency of buckling symptoms. We performed a sensitivity analyses looking at knee based incident outcomes and results were similar.
This study has additional limitations. First, these analyses were based on self-report of instability symptoms rather than objective measurements of instability. Self-report is susceptible to recall bias and subjective variability in interpretation and identification of symptoms. This may be particularly relevant for distinction between buckling and knee slipping and shifting symptoms. In addition, information was gathered on symptoms over the past 3 months. So there is a possibility that participants could have had symptoms prior to the 3 month time point at the baseline visit and could still be included as “incident” symptoms according to this study’s definitions at the follow up visits. Next, we expected the risk factors (vibratory sense and quadriceps strength) would affect study outcomes among subjects exposed to extreme low or high levels and so we used a standard deviation from the mean to stratify our risk factors. In addition, it should be noted that our “worsening” outcomes definition included participants who reported worsening in frequency of symptoms at least once during the two follow up visits, so some of these participants may have improved or stayed the same during one visit. However, we feel any signal of worsening in frequency over the study period identifies a group of interest for evaluation. Finally, our approach of looking at baseline strength and vibratory acuity with longitudinal outcomes of knee instability was well suited for our aims in the current study. In future studies in which longitudinal data of all variables are available, it may be worthwhile to examine relationship between concurrent changes in strength, vibration and instability.
In summary, this study suggests that vibratory acuity and quadriceps strength are important risk factors for knee instability. Considering the significant clinical consequences of knee instability, these factors should be strongly considered in interventional studies for the management of knee OA.
Acknowledgments
This study was supported by the NIH and NIA under the following grant numbers: AG18820, AG18832, AG18947, and AG19069.
Footnotes
COMPETING INTERESTS
No authors declare financial or personal relationships with other people or organizations that could potentially inappropriately influence (bias) their work and conclusions.
References
- 1.Van der Esch M, Knoop J, Van der Leeden M, Voorneman R, Gerritsen M, Reiding D, et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clin Rheumato. 2012;31(10):1505–10. doi: 10.1007/s10067-012-2025-1. [DOI] [PubMed] [Google Scholar]
- 2.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51(6):941–6. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen US, Felson DT, Niu J, White DK, Segal NA, Lewis CE, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527–34. doi: 10.1016/j.joca.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felson DT, Niu J, McClennan C, Sack B, Aliabadi P, Hunter DJ, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147(8):534–40. doi: 10.7326/0003-4819-147-8-200710160-00005. [DOI] [PubMed] [Google Scholar]
- 5.Knoop J, Van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, et al. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res. 2012;64(1):38–45. doi: 10.1002/acr.20597. [DOI] [PubMed] [Google Scholar]
- 6.Shakoor N, Agrawal A, Block JA. Reduced lower extremity vibratory perception in osteoarthritis of the knee. Arthritis Rheum. 2008;59(1):117–21. doi: 10.1002/art.23241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shakoor N, Lee KJ, Fogg LF, Block JA. Generalized vibratory deficits in osteoarthritis of the hip. Arthritis Rheum. 2008;59(9):1237–40. doi: 10.1002/art.24004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shakoor N, Lee KJ, Fogg LF, Wimmer MA, Foucher KC, Mikolaitis RA, et al. The relationship of vibratory perception to dynamic joint loading, radiographic severity, and pain in knee osteoarthritis. Arthritis Rheum. 2012;64(1):181–6. doi: 10.1002/art.30657. [DOI] [PubMed] [Google Scholar]
- 9.Kavchak AJ, Fernandez-de-Las-Penas C, Rubin LH, Arendt-Nielsen L, Chmell SJ, Durr RK, et al. Association between altered somatosensation, pain, and knee stability in patients with severe knee osteoarthrosis. Clin J Pain. 2012;28(7):589–94. doi: 10.1097/AJP.0b013e31823ae18f. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56(9):2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 11.Segal NA, Nevitt MC, Gross KD, Hietpas J, Glass NA, Lewis CE, et al. The Multicenter Osteoarthritis Study: opportunities for rehabilitation research. PMR. 2013;5(8):647–54. doi: 10.1016/j.pmrj.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 13.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35(10):2047–54. [PMC free article] [PubMed] [Google Scholar]
- 14.Pai YC, Rymer WZ, Chang RW, Sharma L. Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum. 1997;40(12):2260–5. doi: 10.1002/art.1780401223. [DOI] [PubMed] [Google Scholar]
- 15.Sharma L. Proprioceptive impairment in knee osteoarthritis. Rheum Dis Clinics. 1999;25(2):299–314. doi: 10.1016/s0889-857x(05)70069-7. [DOI] [PubMed] [Google Scholar]
- 16.Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73(1):53–6. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- 17.Davis EA, Jones TW, Walsh P, Byrne GC. The use of biothesiometry to detect neuropathy in children and adolescents with IDDM. Diabetes Care. 1997;20(9):1448–53. doi: 10.2337/diacare.20.9.1448. [DOI] [PubMed] [Google Scholar]
- 18.Olsen BS, Nir M, Kjaer I, Volund A, Mortensen HB. Elevated vibration perception threshold in young patients with type 1 diabetes in comparison to non-diabetic children and adolescents. Diabetic Med. 1994;11(9):888–92. doi: 10.1111/j.1464-5491.1994.tb00374.x. [DOI] [PubMed] [Google Scholar]
- 19.Foltz KD, Fallat LM, Schwartz S. Usefulness of a brief assessment battery for early detection of Charcot foot deformity in patients with diabetes. J Foot Ankle Surg. 2004;43(2):87–92. doi: 10.1053/j.jfas.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Rajbhandari SM, Jenkins RC, Davies C, Tesfaye S. Charcot neuroarthropathy in diabetes mellitus. Diabetologia. 2002;45(8):1085–96. doi: 10.1007/s00125-002-0885-7. [DOI] [PubMed] [Google Scholar]
- 21.Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127(2):97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 22.Bennell KL, Kyriakides M, Metcalf B, Egerton T, Wrigley TV, Hodges PW, et al. Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial. Arthritis Rheumatol. 2014;66(4):950–9. doi: 10.1002/art.38317. [DOI] [PubMed] [Google Scholar]
- 23.Knoop J, Dekker J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, et al. Knee joint stabilization therapy in patients with osteoarthritis of the knee: a randomized, controlled trial. Osteoarthritis Cartilage. 2013;21(8):1025–34. doi: 10.1016/j.joca.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452–69. doi: 10.2522/ptj.20100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11(6):303–10. doi: 10.1097/01.rhu.0000191213.37853.3d. [DOI] [PubMed] [Google Scholar]
- 26.Zhou J, Chang S, Hong Y, Sun W, Cong Y, Qin M, et al. Effects of 24-week Tai Chi exercise on the knee and ankle proprioception of older women. Res Sports Med. 2016;24(1):84–93. doi: 10.1080/15438627.2015.1126281. [DOI] [PubMed] [Google Scholar]
- 27.Cho HY, Kim EH, Kim J, Yoon YW. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: a randomized controlled trial. Am J Phys Med Rehabil. 2015;94(3):192–200. doi: 10.1097/PHM.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 28.Alnahdi AH, Zeni JA, Snyder-Mackler L. Muscle impairments in patients with knee osteoarthritis. Sports Health. 2012;4(4):284–92. doi: 10.1177/1941738112445726. [DOI] [PMC free article] [PubMed] [Google Scholar]