Abstract
Purpose
Traumatic cardiac injury (TCI) is a challenge for trauma surgeons as it provides a short therapeutic window and the management is often dictated by the underlying mechanism and hemodynamic status. The current study is to evaluate the factors influencing the outcome of TCI.
Methods
Prospectively maintained database of TCI cases admitted at a Level-1 trauma center from July 2008 to June 2013 was retrospectively analyzed. Hospital records were reviewed and statistical analysis was performed using the SPSS version 15.
Results
Out of 21 cases of TCI, 6 (28.6%) had isolated and 15 (71.4%) had associated injuries. Ratio between blunt and penetrating injuries was 2:1 with male preponderance. Mean ISS was 31.95. Thirteen patients (62%) presented with features suggestive of shock. Cardiac tamponade was present in 12 (57%) cases and pericardiocentesis was done in only 6 cases of them. Overall 19 patients underwent surgery. Perioperatively 8 (38.1%) patients developed cardiac arrest and 7 developed cardiac arrhythmia. Overall survival rate was 71.4%. Mortality was related to cardiac arrest (p = 0.014), arrhythmia (p = 0.014), and hemorrhagic shock (p = 0.04). The diagnostic accuracy of focused assessment by sonography in trauma (FAST) was 95.24%.
Conclusion
High index of clinical suspicion based on the mechanism of injury, meticulous examination by FAST and early intervention could improve the overall outcome.
Keywords: Heart injuries, Cardiac tamponade, Thoracic injuries
Introduction
Traumatic cardiac injury (TCI) is not a common occurrence following chest trauma, which is an important cause of mortality in trauma victims.1 TCI may manifest as cardiac tamponade (CT), which is an immediate life threatening condition and requires early recognition and management. Pericardium facilitates ventriculo-atrial coupling, and regulate coronary tone by prostaglandin release and neuronal innervation.2, 3 Pericardium is a fibrous tissue, which limits its expansion with sudden accumulation of fluid and exerts resistance for immediate expansion leading to diastolic dysfunction.4 In cases of CT following TCI, progressive accumulation of blood within the pericardial sac causes reduction in size of cardiac chambers and their diastolic compliance limits cardiac output.5 Blood accumulated within the pericardium gets clotted and it becomes more difficult for pericardiocentesis resulting in incomplete drainage. Definitive surgical procedure to manage CT is surgical drainage of pericardial blood and repair of underlying cardiac injury.6 Clinical features depend on type of mechanism of injury (blunt or penetrating), and the size of the wound in the cardia or the pericardium. Unlike blunt cardiac injury (BCI), penetrating cardiac injury (PCI) is often dramatic in their presentation and some of them present with cardiac arrest requiring cardiopulmonary resuscitation.7, 8 Narrow pulse pressures with distended jugular vein is often seen in cases of TCI without shock, and all the classical features of cardiac tamponade (Beck's triad and Kussmaul's sign) are rarely witnessed in the hypovolaemic cases especially in the presence of associated injuries. A refractory hypotension in absence of tachycardia may be the presenting feature of cardiac tamponade following blunt injury chest. Administration of intravenous fluids may be more harmful in these patients as it may precipitate tamponade.9, 10 One of the earliest means to detect cardiac tamponade is focused assessment by sonography in trauma (FAST) to visualize fluid in the pericardium. The purpose of this study is to evaluate the factors influencing the outcome following TCI.
Material and methods
Data repository and study design
Prospectively maintained database of TCI patients admitted at a Level-1 Trauma Center, All India Institute of Medical Sciences, New Delhi from July 2008 through June 2013 was retrospectively analyzed. Emergency records, operative details, and outcomes of the intervention were reviewed to obtain data on patient demographics, mechanism of injuries, operative procedures, and autopsy details. Statistical analyses were performed using the SPSS version 15. Mechanism of injuries was categorized into blunt (motor vehicle crash, road traffic injury and fall from height) and penetrating injury (gunshot and stab injuries).
Operative procedure
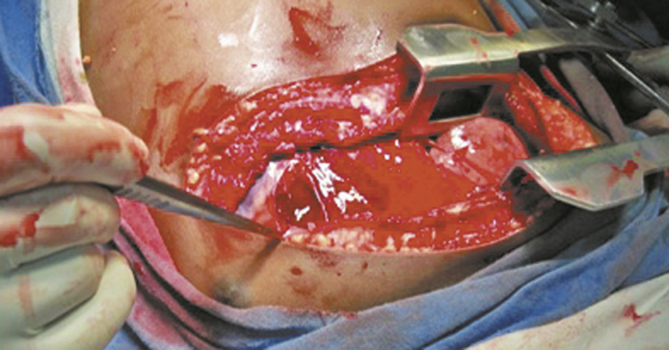
Patients were operated upon under general anesthesia with single lumen endotracheal tube. Heart lung machine was not used in any patient. Patients were explored using bilateral anterolateral thoracotomy approach for better visualization of mediastinum and both hemithorax (Fig. 1, Fig. 2). After opening the pericardial sac, bleeding from cardiac injury was controlled by digital pressure. All the cardiac injuries were repaired using 3-0 polypropylene sutures. Chest tubes were placed in both the hemithorax before closure of thorax. All patients were managed in intensive care unit in postoperative period.
Fig. 1.
Bilateral anterolateral thoracotomy.
Fig. 2.
Digital tamponade.
Results
A total of 1798 patients with predominantly thoracic injuries were admitted during the study period. Mode of injury was blunt trauma in 1529 (85%) cases and penetrating in 263 (15%) cases. Twenty-one patients (1.16%) were diagnosed to have TCI at presentation, of which 18 were men and 3 were women. Blunt and penetrating injuries were noted in 14 and 7 cases respectively. Isolated cardiac injury was seen in 6 cases and rest 15 cases had associated injuries. Out of 14 cases of BCI, only 2 patients had isolated cardiac injury where 4 patients had isolated cardiac injury in PCI group. Mean ISS was 31.95 (range 16–75). Thirteen patients presented with tachycardia (heart rate >100/minute) and 12 presented with hypotension (systolic blood pressure <90 mmHg). FAST was positive (pericardial window) in 20 cases. One patient of blunt chest trauma was FAST negative and was diagnosed to have TCI later on computed tomography scan (CT scan). The diagnostic accuracy of FAST was 95.24%. Contrast enhanced CT scan (CECT scan) of thorax was done only in 9 hemodynamically stable patients and all of them showed pericardial fluid. Cardiac tamponade was present in 12 cases only and they were subjected to surgery without CT scan. However pericardiocentesis was performed in 6 cases prior to surgery. Disposition time from emergency department (ED) to the operation theater ranged from 19 to 36 min in cardiac tamponade group. All 7 patients with PCI underwent surgery while 12 cases (86%) of BCI underwent surgery. Overall 19 out of 21 cases underwent surgery and two cases were managed nonoperatively (Table 1). Overall patients 10 had sustained isolated injury to one cardiac chamber. Three cases sustained injury to more than one cardiac chamber and 4 patients had cardiac injury with great vessel injury. Isolated pericardial injury (with no cardiac chamber injury) was seen in 2 cases (Table 2). Out of 21 cases of TCI, 6 had isolated cardiac injury and 15 had associated injuries (Table 3). Overall the mortality following TCI was 28.5%. Mortality was high in patients who presented with hypotension or had perioperative cardiac arrest or arrhythmias and the differences were statistically significant (Table 1). Cardiac tamponade was not significantly related to mortality (p = 1.000), and pericardiocentesis did not show any survival benefit in our series (p = 1.000). The overall mean hospital stay was 25 days (range 15–46 days).
Table 1.
Demographics and outcome of traumatic cardiac injury patients.
| Variables | Total | Death | Survival | p value |
|---|---|---|---|---|
| Age | Mean = 28.52 | Mean = 32.17 | Mean = 27.07 | 1.000 |
| Gender | Male = 18 | Male = 5 | Male = 13 | 1.000 |
| Female = 3 | Female = 1 | Female = 2 | ||
| Mechanism of injury | Blunt = 14 | Blunt = 3 | Blunt = 11 | 0.354 |
| Penetrating = 7 | Penetrating = 3 | Penetrating = 4 | ||
| ISS | Mean = 31.95 | Mean = 37.00 | Mean = 29.93 | 0.074 |
| HR | >100 = 13 | >100 = 4 | >100 = 9 | 1.000 |
| <100 = 8 | <100 = 2 | <100 = 6 | ||
| SBP | <90 mm Hg = 12 | <90 mm Hg = 3 | <90 mm Hg = 9 | 0.04 |
| >90 mm Hg = 9 | >90 mm Hg = 3 | >90 mm Hg = 6 | ||
| FAST | Positive = 20 | Positive = 6 | Positive = 14 | 1.000 |
| Negative = 1 | Negative = 0 | Negative = 1 | ||
| Cardiac tamponade | Present = 12 | Present = 3 | Present = 9 | 1.000 |
| Absent = 9 | Absent = 3 | Absent = 6 | ||
| Pericardiocentesis | Performed = 6 | Performed = 1 | Performed = 5 | 0.623 |
| Not performed = 15 | Not performed = 5 | Not performed = 10 | ||
| Cardiac arrest | Yes = 8 | Yes = 5 | Yes = 3 | 0.014 |
| No = 13 | No = 1 | No = 12 | ||
| Arrhythmia | Yes = 7 | Yes = 5 | Yes = 2 | 0.001 |
| No = 14 | No = 1 | No = 13 | ||
| Associated injury | Isolated = 6 | Isolated = 2 | Isolated = 4 | 1.000 |
| Associated = 15 | Associated = 4 | Associated = 11 | ||
| Treatment | Surgery = 19 | Surgery = 6 | Surgery = 13 | 1.000 |
| NOM = 2 | NOM = 0 | NOM = 2 | ||
| Total outcome | 21 cases | 6 | 15 |
HR: heart rate, SBP: systolic blood pressure, FAST: focused assessment sonography in trauma, ISS: Injury severity score, NOM: nonoperative management.
Table 2.
Details of cardiac injuries noted intraoperatively.
| Cardiac injuries | Blunt cardiac injury (n = 12) | Penetrating cardiac injury (n = 7) |
|---|---|---|
| RA | 2 | – |
| RV | 4 | 2 |
| LV | 0 | 2 |
| More than one cardiac chamber | 1 (RA + RV) | 2 (RV + LV) |
| One cardiac chamber + vascular injuries | 3 (RA + IMA, RA + SVC, RA + PH) | 1 (LA + PV) |
| Isolated pericardial injury with hemopericardium | 2 | – |
RA: right atrium, RV: right ventricle, LV: left ventricle, IMA: internal mammary artery, SVC: superior vena cava, PH: pulmonary hilum, LA: left atrium, PV: pulmonary vein.
Table 3.
Details of associated injuries in 15 patients with TCI.
| Associated injuries | Number |
|---|---|
| Brain injury | 1 |
| Lung injury | 4 |
| Rib fractures | 4 |
| Diaphragmatic rupture | 1 |
| Abdominal solid organ injury | 7 |
| Hollow viscus injury | 2 |
| Vertebral injury | 1 |
| Long bone fracture | 4 |
Discussion
The prevalence of TCI varies from region to region and institution to institution. It depends on amount of violence in society, volume of motor vehicle crashes, and access to medical facility, etc.11, 12 The incidence of TCI in our study was 1.16% (21/1798), which is comparable to the retrospective population based on the study done by Rhee et al.13 We observed that the incidence of PCI (2.7%, 7/263) was more common than BCI (0.91%, 14/1529). Mandal et al14 reviewed a single institution's 24 year experience and found that cardiac injuries occurred in 6.4% of penetrating thoracic injuries. The difference between PCI in our series and the literature is because the incidence of penetrating thoracic trauma is more common in western countries. The occurrence of TCI was predominantly in men (86%) in our study that is comparable to the incidence reported in the literature.15 In our study cardiac arrhythmia and cardiac arrest were significantly responsible for high mortality in patients with TCI. Survival rate following TCI has been reported from 19% to 74% in the literature.13, 16 The survival rate has improved in recent years due to rapid transportation of trauma to the hospital, rapid assessment in the ED, early surgical intervention and better intensive care.13, 16 In our study 62% patients had hypotension at presentation and 75% of them survived. In the present study, hypotension at presentation in the ED was significantly related to high mortality (p = 0.004) and this is in accordance with the published literature.16
Trauma victims who sustain severe cardiac injury such as valvular injury, septal injury or multiple cardiac chamber injuries usually do not reach to the hospital and succumb to cardiac injuries at the scene. Patients with TCI who survive to reach the hospital usually have sustained injuries limited to one cardiac chamber that can be repaired by trauma surgeons without cardiopulmonary bypass.17 In our series trauma surgeons operated all the patients of TCI without using heart lung machine. Acute pericardial tamponade following trauma requires immediate intervention for better outcome.18, 19, 20 But we did not find cardiac tamponade as an independent risk factor for high mortality (p = 1.000). Therefore trauma surgeons managing TCI should not consider pericardiocentesis as a definitive treatment for CT.17 Moreover pericardiocentesis did not show any survival benefit (p = 1.000) in our series of TCI. Pericardiocentesis will remain a temporizing measure to buy time while preparing the patient for surgery.18, 19, 20 The management and outcome of TCI are often dictated by the mechanism of injury, hemodynamic status and clinical features.20 Patients with BCI without features of cardiac tamponade and with minimal hemopericardium on CT scan may be treated nonoperatively by doing serial physical examination and echocardiography.21 PCI patients often require surgery.12, 17 In our series 100% PCI patients underwent surgery, while 86% cases required surgery in BCI group. Associated injuries were more often seen with blunt injury than in penetrating injury in our series. But associated injuries did not affect the survival rate significantly (p = 1.000). FAST is a good investigating tool to detect fluid in the pericardial sac. In our study, diagnostic accuracy of FAST was 95.24%, and sensitivity and negative predictive values were 100%, which are in accordance with a prospective, multicentre study of ultrasound in patients with possible cardiac injuries by Rozycki et al and others who reported 100% sensitivity and 97% accuracy.22, 23, 24 We observed that most frequently injured cardiac chamber was right ventricle followed by right atrium and left ventricle respectively. These findings are in accordance with the published literature.25, 26
Conclusion
Possibility of occult cardiac injury must always be kept in patients who sustained torso trauma without obvious reason for shock. FAST has good diagnostic accuracy for detecting fluid in pericardium. Acute pericardial tamponade requires immediate drainage for better outcome. Cardiac tamponade is not an independent risk factor of mortality in TCI, and pericardiocentesis will not improve the survival in TCI. Emergency thoracotomy for acute traumatic pericardial tamponade and repair of underlying cardiac injury by trauma surgeon could improve the survival rate. Cardiac arrhythmia needs to be addressed promptly, as they are significantly related to mortality in survivors of TCI.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Durham L.A., 3rd, Richardson R.J., Wall M.J., Jr. Emergency centre thoracotomy: impact of pre-hospital resuscitation. J Trauma. 1992;32:775–779. doi: 10.1097/00005373-199206000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Hoit B.D. Pericardial disease and pericardial tamponade. Crit Care Med. 2007;35:S355–S364. doi: 10.1097/01.CCM.0000271159.84639.2B. [DOI] [PubMed] [Google Scholar]
- 3.Namai A., Sakurai M., Fujiwara H. Five cases of blunt traumatic cardiac rupture: success and failure in surgical management. Gen Thorac Cardiovasc Surg. 2007;55:200–204. doi: 10.1007/s11748-007-0106-x. [DOI] [PubMed] [Google Scholar]
- 4.Reddy P.S., Curtiss E.I., O'Toole J.D. Cardiac tamponade: hemodynamic observations in man. Circulation. 1978;58:265–272. doi: 10.1161/01.cir.58.2.265. [DOI] [PubMed] [Google Scholar]
- 5.Roy C.L., Minor M.A., Brookhart M.A. Does this patient with a pericardial effusion have cardiac tamponade? J Am Med Assoc. 2007;297:1810–1818. doi: 10.1001/jama.297.16.1810. [DOI] [PubMed] [Google Scholar]
- 6.Maisch B., Seferovic P.M., Ristic A.D. Guidelines on the diagnosis and management of pericardial diseases executive summary; the Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587–610. doi: 10.1016/j.ehj.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Degiannis E., Loogna P., Doll D. Penetrating cardiac injuries: recent experience in South Africa. World J Surg. 2006;30:1258–1264. doi: 10.1007/s00268-005-0463-5. [DOI] [PubMed] [Google Scholar]
- 8.Tyburski J.G., Astra L., Wilson R.F. Factors affecting prognosis with penetrating wounds of the heart. J Trauma. 2000;48:587–590. doi: 10.1097/00005373-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Cogswell T.L., Bernath G.A., Keelan M.H., Jr. The shift in the relationship between intrapericardial fluid pressure and volume induced by acute left ventricular pressure overload during cardiac tamponade. Circulation. 1986;74:173–180. doi: 10.1161/01.cir.74.1.173. [DOI] [PubMed] [Google Scholar]
- 10.Hashim R., Frankel H., Tandon M. Fluid resuscitation-induced cardiac tamponade. J Trauma. 2002;53:1183–1184. doi: 10.1097/00005373-200212000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Inkinen J., Kirjasuo K., Gunn J. Penetrating trauma; experience from Southwest Finland between 1997 and 2011, a retrospective descriptive study. Eur J Trauma Emerg Surg. 2015;41:429–433. doi: 10.1007/s00068-014-0445-0. [DOI] [PubMed] [Google Scholar]
- 12.Soto J.R., Murry J.S., Truitt M.S. Penetrating cardiac injuries at a Level II trauma center: a 15 year review. Am Surg. 2015;81:324–325. [PubMed] [Google Scholar]
- 13.Rhee P.M., Foy H., Kaufmann C. Penetrating cardiac injuries: a population-based study. J Trauma. 1998;45:366–370. doi: 10.1097/00005373-199808000-00028. [DOI] [PubMed] [Google Scholar]
- 14.Mandal A., Sanusi M. Penetrating chest wounds: 24 years experience. World J Surg. 2001;25:1145–1149. doi: 10.1007/BF03215862. [DOI] [PubMed] [Google Scholar]
- 15.Naughton M.J., Brissie R.M., Bessey P.Q. Demography of penetrating cardiac trauma. Ann Surg. 1989;209:676–681. doi: 10.1097/00000658-198906000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodrigues A.J., Furlanetti L.L., Faidiga G.B. Penetrating cardiac injuries: a 13-year retrospective evaluation from a Brazilian trauma center. Interact Cardiovasc Thorac Surg. 2005;4:212–215. doi: 10.1510/icvts.2004.099952. [DOI] [PubMed] [Google Scholar]
- 17.Heus C., Mellema J.J., Giannakopoulos G.F., Zuidema W.P. Outcome of penetrating chest injuries in an urban level I trauma center in the Netherlands. Eur J Trauma Emerg Surg. 2015 Apr 25 doi: 10.1007/s00068-015-0533-9. (Epub ahead of print) PMID: 26038051. [DOI] [PubMed] [Google Scholar]
- 18.Lee T.H., Ouellet J.F., Cook M. Pericardiocentesis in trauma: a systematic review. J Trauma Acute Care Surg. 2013;75:543–549. doi: 10.1097/TA.0b013e3182a1fea2. [DOI] [PubMed] [Google Scholar]
- 19.Callaham M. Acute traumatic cardiac tamponade: diagnosis and treatment. JACEP. 1978;7:306–312. doi: 10.1016/s0361-1124(78)80194-4. [DOI] [PubMed] [Google Scholar]
- 20.Spondick D.H. Acute cardiac tamponade. Pathologic physiology, diagnosis and management. Prog Cardiovasc Dis. 1967;10:64–96. doi: 10.1016/s0033-0620(67)80006-9. [DOI] [PubMed] [Google Scholar]
- 21.El-Menyar A., Al Thani H., Zarour A. Understanding traumatic blunt cardiac injury. Ann Card Anaesth. 2012;15:287–295. doi: 10.4103/0971-9784.101875. [DOI] [PubMed] [Google Scholar]
- 22.Rozycki G.S., Feliciano D.V., Ochsner M.G. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma. 1999;46:543–551. doi: 10.1097/00005373-199904000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Patel A.N., Brennig C., Cotner J. Successful diagnosis of penetrating cardiac injury using surgeon-performed sonography. Ann Thorac Surg. 2003;76:2043–2046. doi: 10.1016/s0003-4975(03)01057-9. [DOI] [PubMed] [Google Scholar]
- 24.Tayal V.S., Beatty M.A., Marx J.A. FAST (focused assessment with sonography in trauma) accurate for cardiac and intraperitoneal injury in penetrating anterior chest trauma. J Ultrasound Med. 2004;23:467–472. doi: 10.7863/jum.2004.23.4.467. [DOI] [PubMed] [Google Scholar]
- 25.Wall M.J., Mattox K.L., Chen C.D. Acute management of complex cardiac injuries. J Trauma. 1997;42:905–912. doi: 10.1097/00005373-199705000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Kaljusto M.L., Skaga N.O., Pillgram-Larsen J. Survival predictor for penetrating cardiac injury; a 10-year consecutive cohort from a Scandinavian trauma center. Scand J Trauma Resusc Emerg Med. 2015;23:41. doi: 10.1186/s13049-015-0125-z. [DOI] [PMC free article] [PubMed] [Google Scholar]