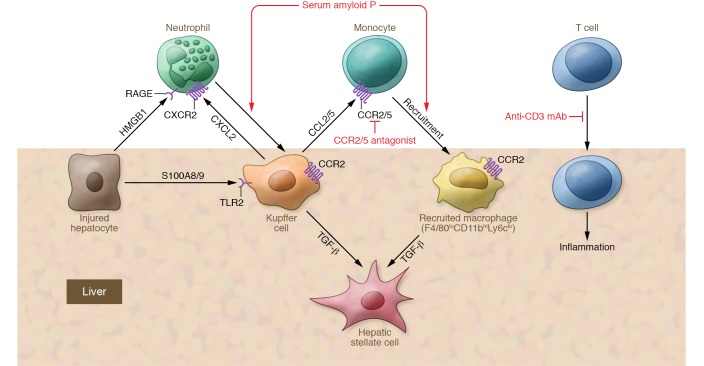
Figure 2. Interaction of immune cells and the liver.
The initiation of inflammation results in the trafficking and localization of immune cells to the site of injury, including neutrophils, recruited macrophages, and Tregs. Generation of an intravascular chemokine gradient (e.g., CXCL12) directs neutrophil migration toward damage foci. HMGB1 released by necrotic hepatocytes also mediates the recruitment of neutrophils through interaction with the HMGB1 receptor RAGE. Monocyte infiltration into the liver is primarily controlled by CCR2 and its ligand CCL2, which may serve as therapeutic targets in nonalcoholic steatohepatitis (NASH). Serum amyloid P binds to neutrophils and decreases TNF-α– and IL-8–induced neutrophil adhesion to extracellular matrix proteins, attenuates profibrotic macrophages, activates the complement pathway, and promotes phagocytosis of cell debris. Oral administration of an anti-CD3 mAb induces Tregs and has been shown to be effective in a NASH animal model; this antibody is currently in clinical trials. The CCR2/5 antagonist cenicriviroc is now in clinical trials.