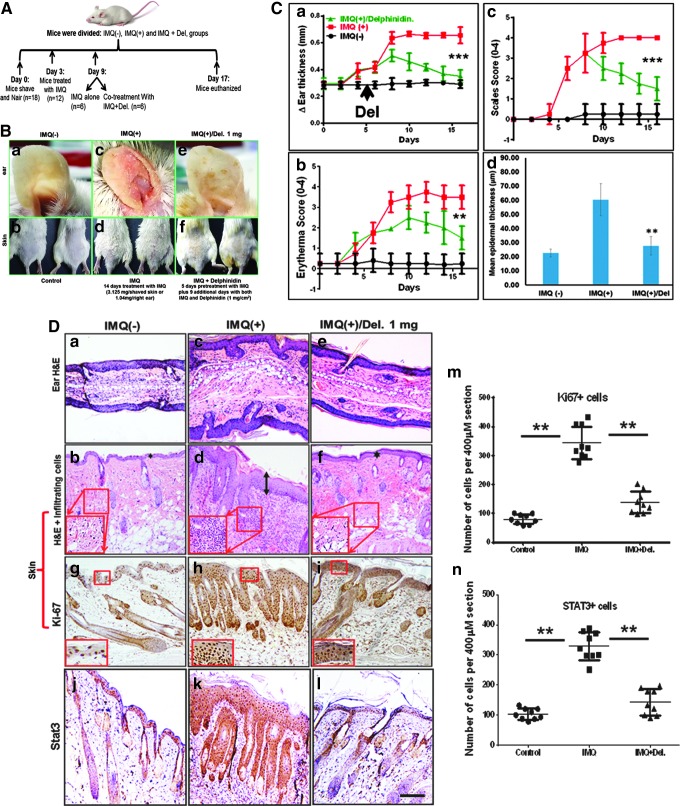
FIG. 6.
Effect of Del treatment on pathological markers of IMQ-induced psoriasiform lesions in Balb/c mouse skin. Treatment with IMQ induces phenotypic skin changes resembling human psoriasis, and topical application of Del significantly alleviates these changes, including inhibition of epidermal hyperproliferation, decreases acanthosis, and reduces the severity of IMQ-induced psoriasis-like skin disease in Balb/c mice. Shown are macroscopic phenotypical presentation and histological analysis of inflamed mouse ear and back skin after 14 days of topical treatment with IMQ with or without cotreatment with Del. (A) Schematic representation of the treatment and experimental setup protocol before and after IMQ-induced lesion and/or Del treatment. Breifly, 6–8-week-old mice were topically treated for 14 consecutive days with 5% IMQ-containing cream (Aldara; 3.125 (skin−1) and 1.63 mg ear−1 day-1) or IMQ cream alone for 5 days, followed by cotreatment with IMQ cream and Del (1 mg cm−2 day−1) for further 9 days or control Vaseline cream. Fourteen days after the mice were sacrificed, samples were taken for further analyses. (c, d–m) Macroscopic views of ear (a, c, e) and back skin (b, d, f) from mice after 14 days. (B) Morphological analysis of inflamed ear and skin treated with IMQ alone (c, d), combination of IMQ and Del (e, f) compared with control (a, b). IMQ treatment induces inflammation and increased scales in ear and skin (c, d), Del treatment of inflamed IMQ-induced skin lesions markedly reduced both inflammation and scaling (e, f) to almost near normal phenotype observed in vehicle-treated control ear and skin (a, b). (C) Quantitative histological/severity assessment of changes in (a) ear thickness (measured in millimeters), (b) inflammation score, and (c) scales score throughout the 14-day experimental period, as well as (d) epidermal thickness after 14-day treatment in mice treated with vehicle control cream (Vaseline), compared with IMQ-alone (IMQ+) and IMQ and Del (IMQ+Del) therapy. Measure of epidermal thickness of the ear and back skin of mice shows that Del is effective in reducing IMQ-induced increases in epidermal thickness (d). For (a–c), each data point represents the mean of 6 random mice per group per time point measured. **denotes p < 0.01, ***denotes p < 0.001. (D) Hematoxylin and eosin (H&E) staining of mouse ear (a, c, e) and skin (b, d, f) of control (a, b), IMQ alone treated (c, d), and cotreated with IMQ and Del (e, f). (c, d) IMQ alone treated (middle panels) reflecting the hallmarks of psoriasis with abnormally thickened epidermis, parakeratosis (nucleated keratinocytes in the stratum corneum), thickened keratinized upper layer (hyperkeratosis (double-headed arrow), increased epidermal rete ridges, and increased immune cell influx (insets in H&E) compared with control (a, b). Data show that in addition to effectively reducing epidermal thickness, Del also reduces infiltration of immune cells in skin (e, f, and insets). Immunohistochemical staining for epidermal proliferation marker Ki67 (g–I, m) and Stat3 (j–l, n) (dark brown staining) expression shows increases in IMQ-treated section (h, k) and decrease of these markers after 9 days of consecutive treatment with Del. (m, n) Quantitative data are representative of the control group vs. IMQ-treated group vs. Del+IMQ-treated group. Symbols represent sections analyzed, and horizontal lines indicate averages of groups. **p ≤ 0.01. (magnification, × 200). IMQ, imiquimod. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/ars