Abstract
We report the case of a woman in her 60s with confirmed multiple self-healing squamous epitheliomas (MSSE) Ferguson-Smith. After recurrences following surgery and radiotherapy, the patient was successfully treated with minimal surgical intervention combined with intralesional injections of triamcinolone acetate. The histological comparison between mature and regressed keratoacanthomas (KA) revealed an increased inflammatory infiltrate with numerous plasmacytoid dendritic cells in the regressed KA in comparison to the mature one, speaking in favor of an inflammation-mediated regression process. Corticosteroids injection in MSSE may have paradoxical effects with action on the proliferation phase rather than the inflammatory regression phase of the KA. Our case confirms previous reports showing that radiotherapy may exacerbate MSSE and should be avoided. Intralesional triamcinolone acetate injection is a safe and easy to use method also effective for multiple lesions. Our case underlines the difference between squamous cell carcinoma and KA, responding differently to therapies like imiquimod or radiotherapy.
Key Words: Keratoacanthoma, Squamous cell carcinoma, Radiation therapy, Steroids
Case Report
A woman in her 60s was referred to our clinic after the fourth recurrence in 3 months of a histologically confirmed keratoacanthoma (KA). The lesion had been resected three times and grafted. Examination revealed a firm, skin-coloured, centrally keratin-filled dome-shaped nodule on the back of the left hand (fig 1a). The patient was Fitzpatrick skin type II with marked bilateral photodamage on forearms and hands. Histology of previous biopsies showed well-differentiated squamous cell carcinomas (SCCs) reminiscent of KA with acanthotic epidermis, enlarged keratinocytes in the basal and spinous layers and keratinized areas with a pale glassy cytoplasm and hyperkeratosis surrounded by inflammatory infiltrates of neutrophils and eosinophils (fig 2).
Fig. 1.

Clinical pictures before and after treatment. a Patient at presentation with the fourth recurrence in 3 months of a skin lesion on the back of the left hand. b Recurrence after radiotherapy. c Cure after intralesional injections of triamcinolone acetate.
Fig. 2.
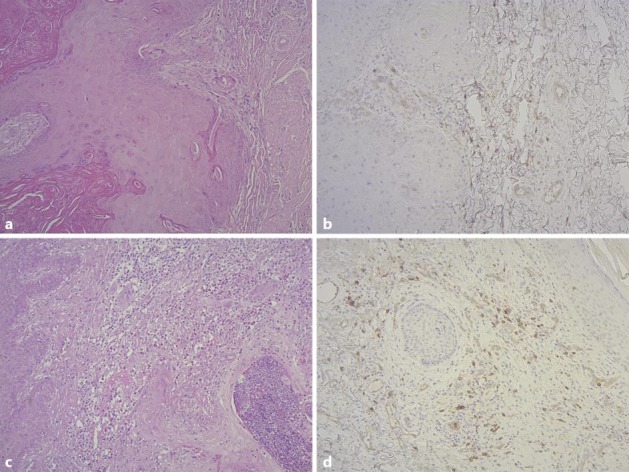
Histological pictures of keratoacanthoma. Haematoxylin and eosin stain (a) as well as CD123 staining (b) of a mature keratoacanthoma. Haematoxylin and eosin stain (c) as well as CD123 staining (d) of a keratoacanthoma in regression.
The patient refused further surgical intervention at this time and was treated instead with conventional radiotherapy on the left hand (energy 50 kV in 12 fractions with a total dose of 48 Gy). Within 1 month after the end of radiotherapy, the tumour recurred around the radiotherapy field (fig 1b) and two new tumours appeared on the extensor surface of the right arm. Histological examination of recurring and new lesions (fig 2) showed a picture identical to the previous biopsies and the tumours were interpreted as KA. Based on this recent history of recurrent KA, multiple self-healing squamous epithelioma (MSSE) Ferguson-Smith was suspected [1]. Mutation analysis of genomic DNA from blood revealed a p.Arg80X nonsense mutation (c.238C>T) in exon II of the transforming growth factor beta receptor 1 gene (TGFBR1), as described in other MSSE patients [2] confirming the diagnosis despite negative family history and late appearance of the first KA in the 7th decade.
The patient then agreed to minimal surgical intervention combined with intralesional injections of triamcinolone acetate, which induced rapid healing of the three lesions (fig 1c). Neither lesion recurred over a 4-year follow-up.
Comparison between mature (fig 2a, b) and spontaneously regressed (fig 2c, d) KA using haematoxylin and eosin and staining with CD123 plasmacytoid dendritic cell surface marker revealed a strongly increased inflammatory infiltrate with numerous plasmacytoid dendritic cells in the regressing KA versus the mature one.
Discussion
Morphologically close to cutaneous SCC, KA is a benign tumour, rapidly growing over 4–5 weeks before spontaneous regression over weeks or months, leaving a scar [1]. KAs are usually solitary lesions, but multiple forms exist like the MSSE, or Ferguson-Smith disease, an autosomal-dominant genodermatosis. The origin and behaviour of KA is controversial: KA is sometimes classified as a variant of SCC, sharing local destructive and metastatic capacity [3]. Others consider KA as a distinct entity due to its particular histology and spontaneous regression [4, 5, 6]. Recent evidence suggests that the gatekeeper mutations underlying the two may be different. The causal TGFBR1 mutations in multiple KA of MSSE/Ferguson-Smith disease [2] contrast with the Notch 1/2 gatekeeper mutations in SCC [7]. Further studies are needed to determine whether this is a consistent fundamental distinction between SCC and all KA.
In general, TGF-beta signalling is considered to function as a tumor suppressor in early tumorigenesis and a promoter in late stages. Therefore, the reversal of this paradigm in MSSE, with initial growth and subsequent regression, is not surprising. Similarly, injection of corticosteroids in MSSE may have paradoxical effects with action on the proliferation phase rather than the inflammatory regression phase of the KA. The presence of abundant plasmacytoid dendritic cells in KA compared to cutaneous SCC has been reported [8], but the comparison between regressed and mature KA has not been described yet. Triggering of multiple KA after imiquimod treatment [9] and radiotherapy [10] has been reported.
Our case confirms that radiotherapy exacerbates MSSE and should be avoided. This and the late occurrence of the KA in sun-exposed skin indicate that supplementary driving factors are necessary for MSSE-type KA tumorigenesis besides the primary genomic TGFBR1 mutations. Also, this particular type of KA responds well to excision and corticosteroid prevention of recurrence. Intralesional triamcinolone acetate injection is a safe and easy to use method as reported in older articles [11], especially in patients with contraindications to extensive and repeated surgery, also effective for multiple lesions. Our case underlines the difference between SCC and KA, responding differently to therapies like imiquimod or radiotherapy.
Statement of Ethics
This study was approved by the Commission for Ethics of Human Research of the Canton of Vaud. The patient's written informed consent was obtained.
Disclosure Statement
The authors have no conflicts of interest.
Acknowledgement
This study was supported in part by SNSF grant 31003A-140767 to D.H. and in part by the Biomedical Research Council of Singapore (E.B.L., I.S.). We are indebted to Daniel Bachmann and Isabelle Surbeck for technical support.
References
- 1.Smith JF. A case of multiple primary squamous-celled carcinomata of the skin in a young man, with spontaneous healing. Br J Dermatol. 1934;46:267–272. [Google Scholar]
- 2.Goudie DR, D'Alessandro M, Merriman B, Lee H, Szeverényi I, Avery S, et al. Multiple self-healing squamous epithelioma is caused by a disease-specific spectrum of mutations in TGFBR1. Nat Genet. 2011;43:365–369. doi: 10.1038/ng.780. [DOI] [PubMed] [Google Scholar]
- 3.Hodak E, Jones RE, Ackerman AB. Solitary keratoacanthoma is a squamous-cell carcinoma: three examples with metastases. Am J Dermatopathol. 1993;15:332–342. doi: 10.1097/00000372-199308000-00007. discussion 343–352. [DOI] [PubMed] [Google Scholar]
- 4.Li J, Wang K, Gao F, Jensen TD, Li ST, DeAngelis PM, et al. Array comparative genomic hybridization of keratoacanthomas and squamous cell carcinomas: different patterns of genetic aberrations suggest two distinct entities. J Invest Dermatol. 2012;132:2060–2066. doi: 10.1038/jid.2012.104. [DOI] [PubMed] [Google Scholar]
- 5.Mandrell JC, Santa Cruz D. Keratoacanthoma: hyperplasia, benign neoplasm, or a type of squamous cell carcinoma? Semin Diagn Pathol. 2009;26:150–163. doi: 10.1053/j.semdp.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Weedon DD, Malo J, Brooks D, Williamson R. Squamous cell carcinoma arising in keratoacanthoma: a neglected phenomenon in the elderly. Am J Dermatopathol. 2010;32:423–426. doi: 10.1097/DAD.0b013e3181c4340a. [DOI] [PubMed] [Google Scholar]
- 7.South AP, Purdie KJ, Watt SA, Haldenby S, den Breems NY, Dimon M, et al. NOTCH1 mutations occur early during cutaneous squamous cell carcinogenesis. J Invest Dermatol. 2014;134:2630–2638. doi: 10.1038/jid.2014.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abbas O, Hussein L, Kurban M, Kibbi A-G. Plasmacytoid dendritic cell involvement in the host response against keratoacanthoma. J Am Acad Dermatol. 2014;70:1142–1145. doi: 10.1016/j.jaad.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Pini AM, Koch S, Schärer L, French LE, Läuchli S, Hofbauer GFL. Eruptive keratoacanthoma following topical imiquimod for in situ squamous cell carcinoma of the skin in a renal transplant recipient. J Am Acad Dermatol. 2008;59:S116–S117. doi: 10.1016/j.jaad.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Robertson SJ, Bashir SJ, Pichert G, Robson A, Whittaker S. Severe exacerbation of multiple self-healing squamous epithelioma (Ferguson-Smith disease) with radiotherapy, which was successfully treated with acitretin. Clin Exp Dermatol. 2010;35:e100–e102. doi: 10.1111/j.1365-2230.2009.03668.x. [DOI] [PubMed] [Google Scholar]
- 11.Sanders S, Busam KJ, Halpern AC, Nehal KS. Intralesional corticosteroid treatment of multiple eruptive keratoacanthomas: case report and review of a controversial therapy. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2002;28:954–958. doi: 10.1046/j.1524-4725.2002.02069.x. [DOI] [PubMed] [Google Scholar]


