A 30-year-old heterosexual man presented with a painless erosion lesion on the coronal sulcus for 3 weeks. It was oval, indurated, slightly elevated kissing erosion with clean, smooth bases (Fig. 1). The lesion in the prepuce, being too hard to bend, would flip over all at once when the prepuce was drawn back (dory flop phenomenon). He was otherwise asymptomatic, and the inguinal lymph nodes on both sides were not enlarged. The patient’s history revealed unprotected sexual intercourse with a female partner 5 weeks before the onset of the lesion. Direct immunofluorescence from the lesion confirmed the presence of treponema pallidum (Fig. 2). A rapid plasma reagin (RPR) test was positive, with a titer of 1:4. In addition, a T. pallidum particle agglutination assay was reactive, and a fluorescent treponemal antibody absorption test was reactive for both IgG and IgM antibodies. Serologic analysis for human immunodeficiency virus was negative. Primary syphilis was diagnosed and the patient received benzathine penicillin G and the lesion resolved within 5 weeks (Fig. 3).
Fig. 1.

Indurated, slightly elevated kissing erosion with clean, smooth bases on the coronal sulcus.
Fig. 2.
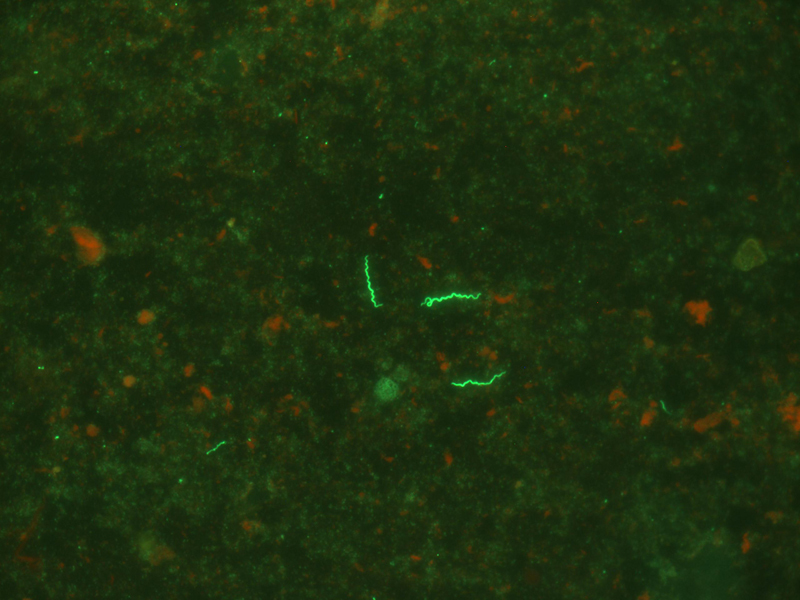
Direct immunofluoresent staining showing T. pallidum.
Fig. 3.

The lesion markedly improved after treatment.
The kissing chancre refers to an ulcer occurring in a fold of the skin or mucous membrane which forms symmetrical lesions on each side. Locations for such ulcers can be on the lips, labia minora and coronal sulcus. The mechanism of kissing chancre is not clear, however, it is assumed that the ulcer is formed when one side of the skin or mucous membrane becomes infected and then autoinfects the other sided from prolonged close contact. Here, we report a kissing chancre on coronal sulcus.
The differential diagnosis of kissing chancre should include genital herpes, chancroid, lymphogranuloma venereum, drug eruption, superficial fungal infection, traumatic injury and lichen planus. Herpetic ulcer should be multiple, painful and superficial, blisters occur at early stage, but atypical lesions may be difficult to distinguish from chancre. Genital herpes is far more common than syphilis, which has become the most common cause of North America “atypical chancre”, however, unlike syphilitic ulcers, Culture of scrapings from the base of the lesion should be positive in herpes. Chancroid ulcers are painful and multiple, exudative without indurated. Lymphogranuloma venereum can have small papular lesions associated with local lymphadenopathy.
A dark-field examination is recommended by many studies for the diagnosis of primary syphilis by visualizing T. pallidum in lesional exudate. It is an inexpensive and rapid diagnostic method but requires a specialized microscope and expertise. Direct immunofluorescent staining for T. pallidum using fluid or tissue is strongly suggested due to high sensitivity. However, serologic testing remains the mainstay for diagnosis of syphilis.
As expected benzathine penicillin therapy induced a rapid regression of the genital lesions. We believe when a positive serologic syphilis test is associated with ulcerative lesion, additional laboratory tests are not necessary. Therefore, syphilis should be considered whenever symmetric genitalia lesions are found. Sexual history is also important.
Conflicts of interest
We declare that we have no conflicts of interest.
Contributors
JL had full access to all of the data and has final responsibility for the integrity of the data and the accuracy of the data analysis. JL was the initial clinician and XKL and ZSW did the literature search. JL devised most of the protocol for management and follow-up of the patient. XKL and ZSW prepared the preliminary draft of the report, which was then revised by JL.


