Abstract
Seasonal influenza is a significant cause of morbidity and mortality of children in Korea. However, few data are available on parental perception and action toward childhood influenza. This study aimed to characterize parental perception and patterns of action in response to influenza and influenza-like illnesses (ILIs), including vaccination and healthcare use. This prospective study involved a random survey of parents whose children were aged 6–59 months. The survey was conducted in October 2014. The study included 638 parents of 824 children younger than 6 years. Most parental information of influenza came from mass media (28.2%) and social media (15.5%). The factor that most often motivated parents to vaccinate their children against influenza was promotion of the government or mass media (36.6%). Negative predictors of immunization included safety concerns about influenza vaccination (28.1%) and mistrust in the vaccine's effectiveness (23.3%). Therefore, correct information about influenza and vaccination from mass media will be one of the cornerstones for implementing a successful childhood immunization program and reducing morbidity and mortality in Korea. Furthermore, to enroll younger children in vaccination programs, and to minimize coverage gaps, public concerns about vaccine safety should be resolved. The demographic data in the present study will be used to provide a deeper insight into a parental perception and will help health care providers increase influenza immunization rate.
Keywords: Survey and Questionnaires, Influenza, Human, Influenza Vaccines, Children
INTRODUCTION
Seasonal influenza is a significant cause of morbidity and mortality in Korea each year, and the incidence is highest in children (1). Moreover, children are a major reservoir for influenza, frequently spreading the disease to other family members and community contacts (2,3,4). Fortunately, influenza is one of the major communicable disease for which vaccines are available, and vaccinating children can reduce the rate and severity of influenza in both children and their families (5,6). The flu vaccine was recommended for everyone from six months of age, but was available free of charge only for people aged 65 years and over under the National Immunization Program (NIP). As of October 2016, the flu vaccines in infants under 12-months-old are also included in NIP.
Several studies have investigated perceptions among adults regarding influenza vaccination. However, few data are available concerning parental perceptions and actions against influenza in their children. Our paper is unique in that this is the first study to ask parental perception regarding influenza and influenza vaccination in Korea.
To understand parental behavior regarding treatment for influenza-like illnesses (ILIs), and to elucidate how parents could be educated more effectively, this study investigated the perspectives and expected patterns of healthcare use by parents of children with influenza. Choosing interventions that are well-matched to public's intention and then implementing those interventions are vital steps toward improving outcomes of public health educations and therapeutics for influenza in children.
MATERIALS AND METHODS
Participants
This is a community-based, cross-sectional study that involves random sample of parents with children aged 6–59 months. We conducted face-to-face interviews in several big marketplaces in Ansan and Jeonju cities. Since there are only one tertiary-level hospitals in each city, the percentage of patients utilizing emergency services can be estimated by reviewing hospital visit data in each single center. The survey-eligible population consisted of parents or caregivers of children aged between 6 and 59 months of age as of October 2014. We randomly interviewed 638 parents.
Questionnaire design
After obtaining consent, a trained interviewer conducted the survey. The interview questionnaire consisted of questions grouped into 3 sections: 1) demographics; 2) influenza-related questions (experience of influenza, parental perception on how influenza can be prevented, whether the parent immunizes their child against influenza, the factors that influenced their decision to accept or refuse the vaccine, and whether the media, government policy statements, or the opinions of their relatives had affected their attitude toward vaccination); and 3) patterns of healthcare usage for ILIs during influenza season. The survey content was based primarily on the Health Belief Model (HBM), which theorizes that parents' vaccination decisions are based on the following beliefs: perceived susceptibility of their child to influenza, perceived severity of influenza, perceived risks of vaccination, perceived benefits of vaccination, and perceived barriers to vaccination (7). The questionnaire included 23 questions. Parents could cite multiple answers for some questions. Table 1 shows section of the questionnaire on the influenza based on the HBM.
Table 1. Questionnaires on influenza based on the Health Belief Model (HBM).
| Drivers | Perceived susceptibility | • One of my family members or relatives has experienced the influenza |
| • My child is at high risk of getting influenza | ||
| Perceived severity | • Influenza can cause serious health problems for my child | |
| • Influenza is highly contagious | ||
| • Influenza complications can be very dangerous | ||
| Perceived benefits | • Influenza vaccination is the most effective way to prevent the disease | |
| • The influenza vaccine can reduce the symptoms and complications of the disease | ||
| • The influenza vaccine is effective at preventing the disease | ||
| Barriers | Perceived barriers | • The influenza vaccine is not safe for children |
| • I have negative feelings about the influenza vaccine | ||
| • The influenza vaccine is not effective | ||
| • There are many side effects of the influenza vaccine | ||
| • The influenza vaccine weakens the immune system | ||
| • Getting the influenza vaccine is not convenient | ||
| • The influenza vaccine is costly |
Data analysis
The data were categorized and analyzed using Statistical Package for the Social Sciences for Windows ver. 18.0 (SPSS Inc., Chicago, IL, USA). Categorical variables are presented as percentages. To test for significance, the χ2 test was performed. A P value < 0.05 was considered statistically significant, while a P value < 0.01 was considered highly significant.
Ethics statement
This study was approved by the Institutional Review Board of Korea University Ansan Hospital (No. AS14066). Informed consent was submitted by all subjects when they were enrolled.
RESULTS
Demographic (general) characteristics
A total of 638 persons with 824 children completed the interview; 41.5% of the children were younger than 36 months, and 58.5% were aged between 37 and 59 months. Of all the children, 51.9% lived in Ansan, and 48.1% lived in Jeonju; 54.8% of the families had 2 children, 39.0% had 1 child, and 6.2% had 3 children. Most children (87.9%) did not live with their grandparents; 50.8% of the respondents were working mothers. In 28.1% of the families, family income was under 2,500 USD; it was between 2,500 and 4,200 USD in 42.3% of the families, and over 4,200 USD in 24.9% of the families (USD/KRW = 1,166 as of November, 2016); 4.7% of the respondents declined to disclose their family income. Educational background was high, as 74.8% of the responders had a college degree or higher, and 21.6% had a high school education or lower; 3.6% of respondents declined to disclose their educational background. The mean number of household members was 4.13. Most (95%) of the children were healthy, while 5% had underlying diseases (epilepsy, asthma, allergic rhinitis, atopic dermatitis, ventricular septal defect, pulmonary stenosis, supraventricular tachycardia, vesicoureteral reflux, hydronephrosis, and Hirschsprung's disease). Table 2 presents the demographic characteristics of the survey respondents.
Table 2. Demographic characteristics of the survey respondents and type of visiting hospital during the daytime.
| Variables | No. (%) | Proportion of samples, % (n = 824) |
||
|---|---|---|---|---|
| ≤ 36 mon | 37–59 mon | |||
| Total | 824 (100.0) | 41.5 | 58.5 | |
| Residence | Ansan | 428 (51.9) | 41.6 | 58.4 |
| Jeonju | 396 (48.1) | 41.4 | 58.6 | |
| No. of the child | 1 | 321 (39.0) | 28.7 | 71.3 |
| 2 | 452 (54.9) | 48.5 | 51.5 | |
| 3 | 51 (6.2) | 60.8 | 39.2 | |
| Family structure | Nuclear family | 724 (87.7) | 41.9 | 58.1 |
| Extended family | 100 (12.1) | 39.0 | 61.0 | |
| Maternal working status | Housewife | 419 (50.8) | 45.8 | 54.2 |
| Working | 405 (49.2) | 37.0 | 63.0 | |
| Monthly household Income, USD | < 2,500 | 241 (29.2) | 42.7 | 57.3 |
| 2,500–4,200 | 334 (40.5) | 38.9 | 61.1 | |
| > 4,200 | 211 (25.6) | 43.1 | 56.9 | |
| No response | 38 (4.6) | 47.4 | 52.6 | |
| Parent or guardian's highest education | ≤ High school | 169 (20.5) | 37.3 | 62.7 |
| ≥ College | 625 (75.8) | 42.4 | 57.6 | |
| No response | 30 (3.6) | 46.7 | 53.4 | |
Experience of influenza in the family
About 15.2% of the responders stated that at least 1 of their family members had contracted influenza; in 37.5% of cases, the first child had been infected, whereas 15.5% of cases involved the father, 13.2% the mother, 13.4% the grandparents, and 8.5% the second child. Region, number of children, number of family members, age of children, socio-economic state, maternal working status, and parental educational background were not associated with contracting influenza.
Parental perception on severity and infectivity of the disease
Many parents (64.9%) believed that influenza could cause serious problems in their children. Over half (57.4%) of the parents thought that complicated influenza would be very dangerous for their child. The perceived complication rate was higher in parents of older children than that of younger children (P = 0.038). With regards to the infectivity of influenza, 62.7% of parents thought that influenza viruses can be transmitted easily from person to person among family members.
Parental perception on preventive method
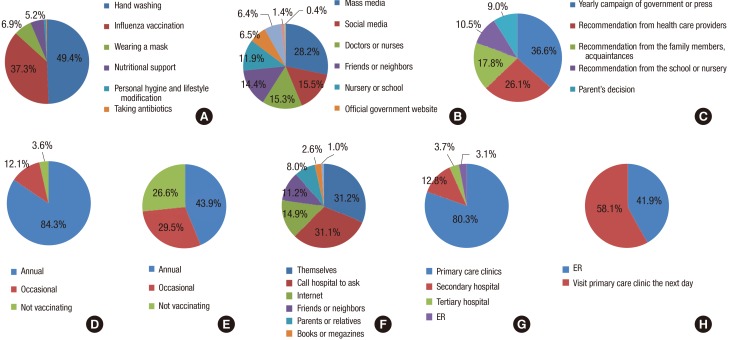
Fig. 1A summarizes parental attitudes on the most effective way to prevent influenza. About half of the respondents (49.4%) thought that hand washing was the most effective preventive method, and 37.3% of the respondents thought that influenza vaccination was the most effective.
Fig. 1.
Survey results.
(A) Most effective ways to prevent influenza. (B) Sources of information on influenza and vaccination. (C) Motivating factors for influenza vaccination. (D) Influenza vaccination status in children. (E) Influenza vaccination status in parents. (F) Decision making in hospital visits. (G) Type of visiting hospital during the daytime. (H) Type of visiting hospital during the nighttime.
ER = emergency room.
Parental perception on the influenza vaccination
Most (84.3%) of the respondents had a positive perception of the influenza vaccination, and some (2.6%) had a negative perception. Regarding the effectiveness of the vaccination, 28.8% of respondents believed that it could prevent influenza, and 40.9% of respondents thought that vaccination would alleviate symptoms or prevent complications of the disease. Parents who lived with their child's grandparents, and those with more children, tended to think that the influenza vaccine was effective (P = 0.042 and P = 0.042, respectively).
Parental educational background was not related to vaccination rate, but parents with a higher educational level tended to think the vaccination was troublesome. Specifically, a higher proportion of respondents with higher education answered that vaccinating children with the influenza vaccine was troublesome and uncomfortable (26% of respondents with advanced degree, 16.8% of college graduates, 8.2% of high school graduates; P = 0.010).
Many (64.8%) parents considered the influenza vaccines to be expensive. Housewife-mothers than working mothers (P = 0.001), and parents in low-income families than in high-income families were more likely to think the vaccine is expensive (P = 0.001).
When asked about the side effects of the vaccine, 3.9% answered that influenza vaccines have many side effects. A small percentage (4.2%) of the parents thought the vaccine would weaken the immune status of the child. When asked about the safety of influenza vaccination in children, only 29.5% answered that the vaccine is safe.
Sources of information on influenza and vaccination
Our data showed that 28.2% of the respondents obtained information on influenza and influenza vaccination from the mass media (TV/radio/newspaper/magazines), followed by social media (portal sites/online communities; 15.5%), doctors/nurses (15.3%), friends/neighbors (14.4%), nurseries/schools (11.9%), the official government website (6.5%), and families/relatives (6.4%). Other sources were leaflets and text messages (1.4%); 0.4% of the respondents had never heard any information. These results imply that parents rely more on direct or indirect personal experiences (48.2%) than on government policy or expert opinion. The result is summarized in Fig. 1B.
Motivating factor for vaccination
Fig. 1C summarizes parental responses to questions about social factors that affect the acceptance of the influenza vaccine. About a third (36.6%) of the respondents were motivated to vaccinate their children by a yearly government or press campaign, followed by recommendations from a healthcare provider (26.1%) or a family member (17.8%).
Influenza vaccination status
Most parents (96.4%) had immunized their child against influenza in the previous year; 84.3% reported annual vaccination, whereas 3.6% of the parents did not vaccinate their children (Fig. 1D). None of the other factors such as educational background, family income, etc. affected vaccination status.
Regarding parents themselves, 73.4% reported that they had got a flu shot in the previous year, and 43.9% reported that they got the shot annually (Fig. 1E). When asked about their plan for the upcoming influenza season, 92.6% of the parents answered that they would vaccinate their children.
Parent-reported reasons for refusing vaccination
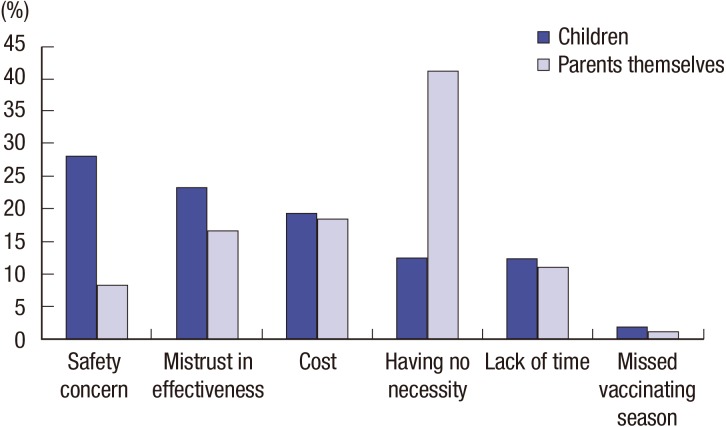
Parents were asked their reasons for refusing the influenza vaccination for their children and for themselves. The results can be seen in Fig. 2. The most frequent answer for the children was “safety concerns” (28.1% of a total of 638 respondents), while that for the adults themselves was the “needlessness of the vaccination” (41.2% of a total of 638 respondents).
Fig. 2.
Reasons for refusal of the influenza vaccination in parents and children.
Decision making in hospital visits during ILIs
When parents had a child with febrile illness, 31.2% responded that they had made the decision to visit the hospital as parents themselves, 31.1% had called the hospital to ask whether to go, 14.9% had used internet searching, 11.2% had asked their friends or neighbors, 8.0% had asked grandparents or other family members, 2.6% had gotten information on infant care from books or magazines, and 1.0% had asked teachers in kindergartens or daycare centers. Parents with low income or low education tended to call the hospital rather than make the decision by themselves. These results are summarized in Fig. 1F.
Fever duration before parents took their febrile child to hospital
During influenza season, most of the respondents (92.1%) took their child to a hospital within 1–2 days of fever onset, and 7.2% waited 3–4 days with a febrile child. No variables—age, number of children, parental income, or education—were related to duration of fever at hospital visit.
Ambulatory medical care utilization in daytime/nighttime fever
Concerning emergency room (ER) visits, when a child had a fever during the daytime, most (80.3%) of the parents visited primary care clinics, and 3.1% visited ER (Fig. 1G). None of the following factors had a significant influence on parental choice of visiting hospital: region, ordinal number or age of the child, family structure, maternal working status, monthly household income, or parent or guardian's highest education. Table 3 shows the result. Fig. 1G shows the type of visiting hospital during the daytime.
Table 3. Type of visiting hospital during the daytime.
| Variables | Pediatric clinic | Public health center | ER | Others | |
|---|---|---|---|---|---|
| Total, % | 80.3 | 0.1 | 3.1 | 16.5 | |
| Residence | Ansan | 82.7 | 0.0 | 3.0 | 14.3 |
| Jeonju | 77.7 | 0.2 | 3.2 | 18.9 | |
| Age of the children, mon | ≤ 36 | 81.8 | 0.0 | 1.8 | 16.4 |
| 37–59 | 79.9 | 0.1 | 3.5 | 16.5 | |
| No. of the children | 1 | 80.5 | 0.0 | 4.2 | 15.3 |
| 2 | 80.4 | 0.2 | 1.8 | 17.6 | |
| 3 | 78.6 | 0.0 | 7.1 | 14.3 | |
| Family structure | Nuclear family | 80.1 | 0.0 | 16.7 | 3.2 |
| Extended family | 81.5 | 0.9 | 14.8 | 2.8 | |
| Maternal working status | Housewife | 80.0 | 0.0 | 17.0 | 3.0 |
| Working | 80.6 | 0.2 | 16.0 | 3.2 | |
| Monthly household Income, USD | < 2,500 | 77.9 | 0.0 | 18.7 | 3.4 |
| 2,500–4,200 | 79.8 | 0.3 | 15.8 | 4.1 | |
| > 4,200 | 83.3 | 0.0 | 15.3 | 1.4 | |
| No response | 83.7 | 0.0 | 14.0 | 2.3 | |
| Parent or guardian's highest education | ≤ High school | 80.3 | 0.0 | 17.6 | 2.1 |
| ≥ College | 80.2 | 0.1 | 16.6 | 3.1 | |
| No response | 82.4 | 0.0 | 8.8 | 8.8 | |
ER = emergency room.
When child had a fever at night, 41.9% of the parents chose to visit ER, and the rest chose to visit the hospital the next day (Fig. 1H). The parents were more likely to visit ER at night when they had fewer children (P = 0.012), an extended family type (P = 0.000), and a lower educational level (P = 0.039). Children's age, maternal working status, and family income were not associated with ER visit at night.
Ambulatory medical care utilization at vaccination
When vaccinating their children, most parents visited private medical facilities (87.6%), and some visited a public health center (9.0%). Parents with a high educational background were more likely to choose a private medical facility for vaccination (P = 0.002). Neither children's age nor household income was associated with the type of hospital chosen for vaccination.
Insurance coverage and hospital visits
Parents were asked whether their private insurance coverage status had influenced their decision on visiting a hospital or choosing the type of hospital. Most parents (74%) answered that it had no influence on their decision.
Data showing regional differences
Ansan and Jeonju have only one tertiary-level hospitals in each city. Ansan is a city of population 694,727, including 74,678 (1.1%) foreigners, with 22,670 (3.3%) up to 36-month-old children and 12,596 (1.8%) 37 to 59-month-old children (8). The number of people receiving basic living security is 21,603 (3.1%) (9). Jeonju is a city of population 659,033, including 5,848 (0.9%) foreigners. There are 23,499 (3.6%) up to 36-month-old children, and 13,328 (2.0%) 37 to 59-month-old children (10). The number of people receiving basic living security is 27,896 (4.2%) (11).
With regards to the perception of influenza, parents in Ansan perceived the severity of influenza in children more highly (P = 0.004), as more parents agreed that influenza could cause serious problems to their children (70.3% in Ansan vs. 59.1% in Jeonju). Furthermore, more parents in Ansan received vaccination annually (48.5% vs. 39.0%; P = 0.032).
When a child had a fever at night, parents in Jeonju (60.6%) were more likely to visit hospital the next day than parents in Ansan (55.8%; P = 0.011). When vaccinating their children, parents in Jeonju were more likely to visit a public health center (14.4%) than parents in Ansan (4.2%; P = 0.000).
DISCUSSION
This survey reveals many important public health issues for childhood influenza immunizations.
Of all family members, influenza was most frequently seen in the first child in this study, perhaps because nurseries or schools tend to perform more group activities with children in this age group. Indeed, because of new governmental policy whereby parents receive financial support to send their children to a nursery, more young children than before would be exposed to such group activities—even infants. This may increase their risk of contracting influenza. Hence, to protect children and reduce the infection in the entire community, it is important to vaccinate this age group. With involvement of infants under 12-months-old in NIP as of October 2016, health education should also target older children to optimize immunization coverage and to provide more extensive herd immunity to the population.
With regards to the question about the most effective way to prevent influenza, half of the respondents (49.4%) thought that hand washing was the most effective. In one study about parental perception of H1N1 influenza (12), parents who believed that infection could be prevented with precautionary measures other than vaccination were 15 times less likely to vaccinate their children, demonstrating the importance of explaining to the public why vaccines are more effective in providing specific protection against certain infectious diseases.
Parents living in an extended family structure were more likely to believe that the influenza vaccine was effective. This may be because families with a large number of members have a high chance of infection, or because such families have a greater chance of obtaining vaccine information from grandparents who receive the influenza vaccine under government support annually.
In this study, children's vaccination rate was shown to be independent of parental educational background, although parents with higher education levels thought that vaccination was troublesome. Conversely, other studies have shown that children of parents with a higher educational background were more likely to be vaccinated (12,13,14). The same studies suggested that this was due to more effective risk-benefit communication between healthcare staff and better educated parents, particularly as regards the balance between personal risk and the safety and effectiveness of the preventive maneuver. Parents with a higher education may also be more prone to accept scientific knowledge rather than non-expert opinions.
Korea is one of the most networked countries in the world ranking third worldwide in 2014 in terms of highest internet penetration rates (15), and ranking first worldwide in 2016 in terms of average internet speed (16). The influence of high accessibility to internet and crowded residential environment in the country might have enabled equalities between individuals with regard to access and use of information, reducing gap between the more and the less educated parents. Other explanation for this discrepancy can be that as parental level of education and access to information increase, parents are more willing to question the vaccines and medications that are offered to their children and want to participate more in the decision making process (17).
Our data showed that parents usually obtain information about influenza and the influenza vaccine from mass media (28.2%) and social media (15.5%). In fact, the most motivating factor was exposure to mass media (TV/radio/newspapers/magazines; 36.6%). In a study of parental attitudes on influenza, reported media exposure was significantly associated with changes in parental influenza-related attitudes: parents were more likely to perceive an influenza outbreak as more severe if they had heard about it in the media. Furthermore, if parents had heard about influenza-related mortality, they were likely to perceive risk of vaccination as being lower. Finally, when parents had heard about vaccine shortages, they were likely to perceive influenza as more severe, and this served to increase the view that vaccination is a social norm (13).
As the most frequent source of information and most motivating factor regarding vaccination was “mass media,” it is important that the media continue to address public health-related issues with thorough discussions based on correct information. This will increase the level of knowledge, awareness, and attention on the topic. In many other studies, the perceived side effects could be because of publicity of exceedingly rare but exaggerated reports of associated side effects such as Guillain-Barre syndrome, which is not proven to have direct associations with vaccination (18,19,20,21). And being influenced by the relatives' opinions or from the politicians or from the media all decreased vaccine acceptance (12,22). It is important to recognize that parents mostly get information regarding vaccines, from mass media, social media, and family members and friends, which can adversely affect vaccination rate owing to incorrect information. Physician's role would be to provide correct knowledge and information besides treating disease of their patient. Physicians could increase the pediatric influenza vaccination rate by improving their recommendation strategies. In this regard, to ensure better communication and treatment, physicians should be aware of parental perception and understanding of the disease. Healthcare providers have a crucial role to play in increasing pediatric vaccination rates, and communicating with parents is beneficial (23). Indeed, one study regarding seasonal influenza vaccines revealed that parents value their physicians' recommendations (24)—when doctors encourage parents to vaccinate their healthy children, the overall proportion of vaccinated children increases significantly. Therefore, during influenza season, vaccination should be encouraged by doctors when children visit the clinic. If the number of missed opportunities in this regard were improved, the pediatric influenza vaccination rate would increase significantly. Our research found that most parents visited primary care clinics; when primary care clinics were not available, they visited ER. Thus, it is especially important that healthcare providers in primary clinics and ERs recommend the influenza vaccination.
Studies have shown that concern about vaccine safety is the most important risk factor for low vaccine acceptance (25,26). Interestingly, when there are high levels of immunization coverage, disease is reduced and public attention shifts to concerns about vaccine safety rather than fear of the diseases. When concerns about vaccine safety become widespread, a loss in public confidence in vaccines can result in a resurgence of the disease (23). Our study also showed that parental fears were associated with low uptake of the seasonal influenza vaccine. Specifically, parents of unimmunized children cited safety concerns about vaccination, mistrust in the effectiveness of vaccination, cost, and the needlessness of vaccination as reasons for their refusal to vaccinate. Among these, “safety concerns” were the primary reason (28.1%), whereas the most common reasons that parents refused the flu shot for themselves were “needlessness of the vaccination” (41.2%)—“safety concerns” were the fifth reason (8.4%).
Fiebach and Viscoli (27) found that, among children under 7 years old in North India, the most common reasons for refusing the vaccine were fear of a reaction to the shot, a previous bad experience, and perception that the patient did not require the vaccine because they rarely became ill. The present study corroborates these results.
As parents think that influenza vaccination is not safe enough in younger children, education from primary care providers about the risks and benefits of immunization and vaccine safety may help address these concerns. To improve the health of children, we need to identify and eliminate systemic barriers that prevent influenza vaccine recommendations from being implemented. Keeping the public well informed will help, as will communicating better with parents regarding the risks and benefits of vaccination.
In summary, data are limited regarding how the parents of young children view influenza and the influenza vaccination. Several previous studies have examined parental attitudes to influenza (24,28), but these studies focused on specific part (physician recommendation) among many factors that affect vaccination rate, or examined data on older children with and without chronic medical conditions. Therefore, they may not be entirely applicable to parents of healthy young children. Our survey mostly involved the parents of healthy young children. To our knowledge, this is the first study about parental perception on influenza and the flu shot in Korean parents. Moreover, since the questionnaires were conducted in a marketplace in both cities, it may be that people without high accessibility to hospitals, or who do not favor medical treatment and services, were included in our study.
Successful prevention of influenza disease will depend in part on educating parents about the influenza vaccine. This process will be aided by an understanding of how parental attitudes about influenza are formed and can change. The findings of the present study indicate specific strategies for public health practitioners to improve vaccination rates. The results will be used in general practice, as they provide patient-centered information.
This study has several potential limitations. Firstly, because the data were collected on the basis of parental recall, and the self-reported influenza vaccination status was validated, the rate of influenza vaccination may have been overestimated or underestimated. Furthermore, the study population was well educated, and reported a relatively high household income, which limits the generalizability of the study to more disadvantaged populations and other clinical settings.
Childhood influenza vaccination in Korea has not been covered under NIP. As a change has been made recently in infants aged under 12-months-old, the effect of cost on actual vaccination rate should be re-evaluated. Also, since the most common reasons for refusing flu shot in children were safety concern and mistrust in effectiveness, further study investigating immunogenicity and reactogenicity of various influenza vaccines administered in children (trivalent inactivated vaccines, quadrivalent vaccines, and live attenuated vaccine) are needed.
Footnotes
Funding: This project was supported by the Transgovernmental Enterprise for Pandemic Influenza in Korea (Grant No. HI10C2146).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Kim DH, Eun B, Kim YK. Data curation: Jo DS, Kim YK. Formal analysis: Song YH. Investigation: Hwang J, Lim CH, Kim DH, Eun B, Kim YK.
References
- 1.Ki HO, Kim IH, Cho EH, Kang MG, Chu H, Lee JY. Korean influenza sentinel surveillance report, 2014–2015 [Internt] [accessed on 25 August 2016]. Available at http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037MNU1380&q_type=&year=2015&cid=66230&pageNum=%20.
- 2.Longini IM, Jr, Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982;115:736–751. doi: 10.1093/oxfordjournals.aje.a113356. [DOI] [PubMed] [Google Scholar]
- 3.Monto AS, Koopman JS, Longini IM., Jr Tecumseh study of illness. XIII. Influenza infection and disease, 1976-1981. Am J Epidemiol. 1985;121:811–822. doi: 10.1093/oxfordjournals.aje.a114052. [DOI] [PubMed] [Google Scholar]
- 4.Fox JP, Cooney MK, Hall CE, Foy HM. Influenzavirus infections in Seattle families, 1975–1979. II. Pattern of infection in invaded households and relation of age and prior antibody to occurrence of infection and related illness. Am J Epidemiol. 1982;116:228–242. doi: 10.1093/oxfordjournals.aje.a113408. [DOI] [PubMed] [Google Scholar]
- 5.Monto AS, Davenport FM, Napier JA, Francis T., Jr Effect of vaccination of a school-age population upon the course of an A2-Hong Kong influenza epidemic. Bull World Health Organ. 1969;41:537–542. [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics; Committee on Infectious Diseases. Influenza. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, American Academy of Pediatrics; Committee on Infectious Diseases, editors. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015. pp. 482–492. [Google Scholar]
- 7.Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, CA: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- 8.Ansan City Hall (KR) Population statistics by age group in Ansan [Internet] [accessed on 18 October 2016]. Available at https://stat.iansan.net/new/Population.jsp?menuId=20002001.
- 9.Ansan City Hall (KR) Statistical information on social welfare services in Ansan [Internet] [accessed on 18 October 2016]. Available at https://stat.iansan.net/new/Welfare.jsp?menuId=20002004.
- 10.Statistics Korea. Population statistics by age group in Jeonju [Internet] [accessed on 18 October 2016]. Available at http://stat.kosis.kr/statHtml_host/statHtml.do?orgId=711&tblId=DT_M0105Y&dbUser=NSI_IN_711.
- 11.Statistics Korea. Statistical information on social welfare services in Jeonju [Internet] [accessed on 18 October 2016]. Available at http://stat.kosis.kr/statHtml_host/statHtml.do?orgId=711&tblId=DT_YB1223_1&dbUser=NSI_IN_711.
- 12.Akis S, Velipasaoglu S, Camurdan AD, Beyazova U, Sahn F. Factors associated with parental acceptance and refusal of pandemic influenza A/H1N1 vaccine in Turkey. Eur J Pediatr. 2011;170:1165–1172. doi: 10.1007/s00431-011-1425-6. [DOI] [PubMed] [Google Scholar]
- 13.Daley MF, Crane LA, Chandramouli V, Beaty BL, Barrow J, Allred N, Berman S, Kempe A. Influenza among healthy young children: changes in parental attitudes and predictors of immunization during the 2003 to 2004 influenza season. Pediatrics. 2006;117:e268–77. doi: 10.1542/peds.2005-1752. [DOI] [PubMed] [Google Scholar]
- 14.Elliott C, Farmer K. Immunization status of children under 7 years in the Vikas Nagar area, North India. Child Care Health Dev. 2006;32:415–421. doi: 10.1111/j.1365-2214.2006.00623.x. [DOI] [PubMed] [Google Scholar]
- 15.Statista (US) Global internet penetration rates in 2014, by country [Internet] [accessed on 18 October 2016]. Available at https://www.statista.com/statistics/470934/global-internet-penetration-rates-by-country/
- 16.Statista (US) Average internet speed by country as of 1st quarter 2016 (in Mbps) [Internet] [accessed on 18 October 2016]. Available at https://www.statista.com/statistics/204952/average-internet-connection-speed-by-country/
- 17.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 18.Baxter R, Bakshi N, Fireman B, Lewis E, Ray P, Vellozzi C, Klein NP. Lack of association of Guillain-Barré syndrome with vaccinations. Clin Infect Dis. 2013;57:197–204. doi: 10.1093/cid/cit222. [DOI] [PubMed] [Google Scholar]
- 19.Vellozzi C, Iqbal S, Broder K. Guillain-Barre syndrome, influenza, and influenza vaccination: the epidemiologic evidence. Clin Infect Dis. 2014;58:1149–1155. doi: 10.1093/cid/ciu005. [DOI] [PubMed] [Google Scholar]
- 20.Vellozzi C, Iqbal S, Stewart B, Tokars J, DeStefano F. Cumulative risk of Guillain-Barré syndrome among vaccinated and unvaccinated populations during the 2009 H1N1 influenza pandemic. Am J Public Health. 2014;104:696–701. doi: 10.2105/AJPH.2013.301651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verity C, Stellitano L, Winstone AM, Stowe J, Andrews N, Miller E. Pandemic A/H1N1 2009 influenza vaccination, preceding infections and clinical findings in UK children with Guillain-Barré syndrome. Arch Dis Child. 2014;99:532–538. doi: 10.1136/archdischild-2013-304475. [DOI] [PubMed] [Google Scholar]
- 22.Rachiotis G, Mouchtouri VA, Kremastinou J, Gourgoulianis K, Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among healthcare workers in Greece. Euro Surveill. 2010;15:19486. [PubMed] [Google Scholar]
- 23.Salmon DA, Pan WK, Omer SB, Navar AM, Orenstein W, Marcuse EK, Taylor J, deHart MP, Stokley S, Carter T, et al. Vaccine knowledge and practices of primary care providers of exempt vs. vaccinated children. Hum Vaccin. 2008;4:286–291. doi: 10.4161/hv.4.4.5752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hemingway CO, Poehling KA. Change in recommendation affects influenza vaccinations among children 6 to 59 months of age. Pediatrics. 2004;114:948–952. doi: 10.1542/peds.2003-0509-F. [DOI] [PubMed] [Google Scholar]
- 25.Eastwood K, Durrheim DN, Jones A, Butler M. Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Australian public. Med J Aust. 2010;192:33–36. doi: 10.5694/j.1326-5377.2010.tb03399.x. [DOI] [PubMed] [Google Scholar]
- 26.Leo HL, Clark SJ, Butchart AT, Singer DC, Clark NM, Davis MM. 2009 seasonal and H1N1 influenza vaccination compliance in asthmatic children and adults. J Allergy Clin Immunol. 2010;126:166–168. doi: 10.1016/j.jaci.2010.03.040. [DOI] [PubMed] [Google Scholar]
- 27.Fiebach NH, Viscoli CM. Patient acceptance of influenza vaccination. Am J Med. 1991;91:393–400. doi: 10.1016/0002-9343(91)90157-s. [DOI] [PubMed] [Google Scholar]
- 28.Poehling KA, Speroff T, Dittus RS, Griffin MR, Hickson GB, Edwards KM. Predictors of influenza virus vaccination status in hospitalized children. Pediatrics. 2001;108:E99. doi: 10.1542/peds.108.6.e99. [DOI] [PubMed] [Google Scholar]