Abstract
Context:
Chronic pelvic pain (CPP) is a common condition of women of the reproductive age group. It has a negative impact on a woman's personal health and quality of life (QOL). Practicing yoga has shown numerous benefits in various chronic painful conditions.
Aim:
To study the effects of yogic intervention on pain scores and quality of life in females of reproductive age group with CPP, on conventional therapy.
Settings and Design:
It is a follow-up, randomized case-control study done in a tertiary care hospital.
Subjects and Methods:
Sixty female patients of CPP in the age group of 18–45 years were randomly divided into Group I (n = 30) and Group II (n = 30). Group I received only conventional therapy in the form of NSAIDS and Group II received yoga therapy in the form of asanas, pranayama, and relaxation along with the conventional therapy for 8 weeks. They were assessed twice (pre- and post-treatment) for pain scores through visual analog scale (VAS) score and QOL by the World Health Organization quality of life-BREF (WHOQOL-BREF) questionnaire.
Statistical Analysis Used:
Repeated measure ANOVA followed by Tukey's test. P < 0.05 was considered significant.
Results:
After 8 weeks of yogic intervention, Group II patients showed a significant decrease in intensity of pain seen by a decrease in VAS score (P < 0.001) and improvement in the quality of life with a significant increase (P < 0.001) in physical, psychological, social, and environmental domain scores of WHOQOL-BREF.
Conclusions:
The practice of yoga causes a reduction in the pain intensity and improves the quality of life in patients with chronic pelvic pain.
Key words: Chronic pelvic pain, pain scores, quality of life, World Health Organization quality of life-BREF, yoga
INTRODUCTION
Chronic pelvic pain (CPP) is defined as an “intermittent or constant pain in the lower abdomen or pelvis of a woman, of at least 6 months duration, not occurring exclusively with menstruation or intercourse and not associated with pregnancy.[1] It is a common condition of the reproductive age of group women, yet its pathophysiology remains poorly understood.[2] In South-East Asian countries, the prevalence of CPP varies from 5.2% in India, 8.89% in Pakistan to 43.2% in Thailand.[3] CPP has a negative impact on a woman's personal health and quality of life (QOL).[4,5]
Though the exact etiology is unknown but CPP may occur due to the involvement and the complex interactions between of gynecological, gastrointestinal, urinary, musculoskeletal, endocrine, and neurologic systems. It may also be influenced by psychological and sociocultural factors.[6] Common conditions that cause CPP are endometriosis, chronic pelvic inflammatory disease, adenomyosis, fibroids, adhesions, celiac disease, colitis, inflammatory bowel disease, fibromyalgia, degenerative disk disease, and chronic urinary tract infection.[7]
The common presentations of CPP are noncyclic lower abdominal pain seen in about 80% of women, congestive dysmenorrhea in 26%, and pelvic tenderness in 20% of cases.[8] Symptoms of depression, anxiety, low QOL, low productivity, decreased energy, sexual dysfunction, and relationship problems are also present in these patients of CPP.[9,10]
The treatment of CPP entails two aspects, one is the treatment of chronic pain, and the other is the treatment of the underlying cause. In most cases, an effective treatment can be achieved by using both approaches. The treatment can be medical or surgical but for those women in whom a definitive diagnosis cannot be reached (61% of women with CPP reported that the etiology was unknown), it requires a multidisciplinary approach, i.e., addressing dietary, social, environmental, and psychological factors in addition to standard medical therapy.[10,11]
Yoga is an effective, time-tested method for improving overall health and managing psychosomatic and chronic degenerative disorders.[12] Practicing yoga regularly has shown improvement in QOL and pain reduction in chronic low back pain.[13,14] Prevalence of musculoskeletal pain (neck pain and lower back pain) was found to be lower in dentists with regular yoga practice as compared to dentists practicing other physical activities or with no physical activity.[15] Yoga therapy has shown a reduction in severity and duration of pain in women with primary dysmenorrhea.[16] Literature survey however has shown a paucity of studies on the beneficial effects of yoga on pain and QOL in females with CPP.
We hypothesized that the use of yogic intervention used along with conventional therapy in CPP patients will help in improving visual analog scale (VAS) score and QOL as compared to conventional therapy alone. The primary objective of our study was to measure VAS score and World Health Organization QOL-BREF (WHOQOL-BREF) scores in CPP patients on conventional therapy and in CPP patients on both conventional + yoga therapy.
SUBJECTS AND METHODS
Sampling
It was a follow-up, randomized case-control study. Eighty CPP patients were recruited from gynecology outpatient department. All subjects underwent complete physical and clinical assessment prior to the participation. Subjects with CPP were randomly divided into two groups Group I and Group II. Simple randomization was done using a computer-generated random number table, and allocation was done by sealed envelope technique. However, nine subjects in Group I could not come for follow-up and ten subjects in Group II showed poor compliance to the yoga regimen. Hence, we selected thirty subjects in each group to participate in our study. Prior to the participation, all the subjects were explained the purpose of study in detail and a written informed consent was taken. This research proposal was approved by the Institutional Research Protocol and Ethics Committee.
Inclusion criteria
Gender: Females
Age: 18–45 years.
Exclusion criteria
Females with obvious gynecological and nongynecological causes of CPP
Gynecological, abdominal, or pelvic malignancy
Desire to conceive
Pregnant females/pregnancy in the past 12 months
Moderate to severe hypertension
Severe low backache
Any other medical disease complicating CPP.
Assessments
Pain assessment was done using VAS and QOL assessment was done through WHOQOL-BREF questionnaire. Both groups (I and II) underwent assessment for the outcome measures at the beginning as well as after 8 weeks of respective therapy. Figure 1 depicts plan of the study.
Figure 1.
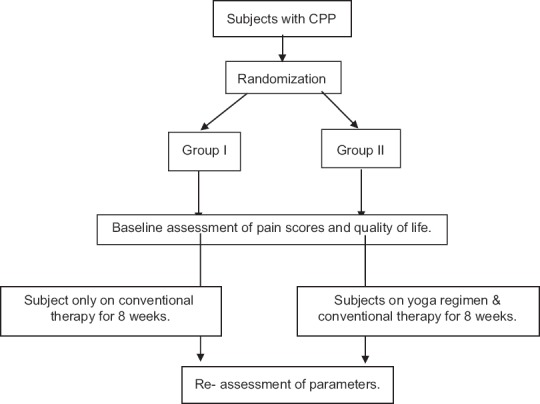
Plan of the study
Visual analog score for pain
VAS is the most extensively used pain measurement tool. It is a unidimensional measurement tool that can be applied to measure pain intensity and pain relief.[17] The scale comprises a 10 cm straight line with verbal anchors that define boundaries. The score is obtained by measuring the distance in millimeters from left to right. It is quick and relatively easy to use. Results are to be considered as follows: Mild/no pain, 0–30; moderate pain, 31–69; and severe pain, 70–100.[18] Studies have shown VAS to be sensitive measure of variation in patient's pain in response to treatment and are reproducible over time for that individual patient.[19]
World Health Organization quality of life-BREF questionnaire
The WHOQOL-BREF is the short 26-item form of the larger WHOQOL-100 assessment that yields four QOL domains: Physical health, psychological, social QOL, and environmental QOL. In addition, it also includes two questions for “overall quality of life” and “general health” facets. The domain scores are scaled in a positive direction (i.e., higher scores denote higher QOL). Responses are scored via five-point response scales with various anchor statements (e.g., from 1 [Very dissatisfied] or/[Very poor] to 5 [Very satisfied] or [Very good]). The WHOQOL-BREF can be scored in three ways; through raw scores and two transformation methods; the first that creates domain scores within the range of 4–20 and the second that creates domain scores within the range of 0–100. The internal consistency of WHOQOL-BREF ranged from 0.66 to 0.84 (Chronbach's alpha coefficient).[20] The WHOQOL-BREFs psychometric properties have been analyzed using cross-sectional data from 11,830 adults from 23 countries and are a valid assessment across cultures and socioeconomic status.[21] The Hindi version of the WHOQOL-BREF has been developed which can be used for intervention studies and drug trials. This instrument holds satisfactory psychometric properties and can be used in an Indian setting.[22]
Intervention
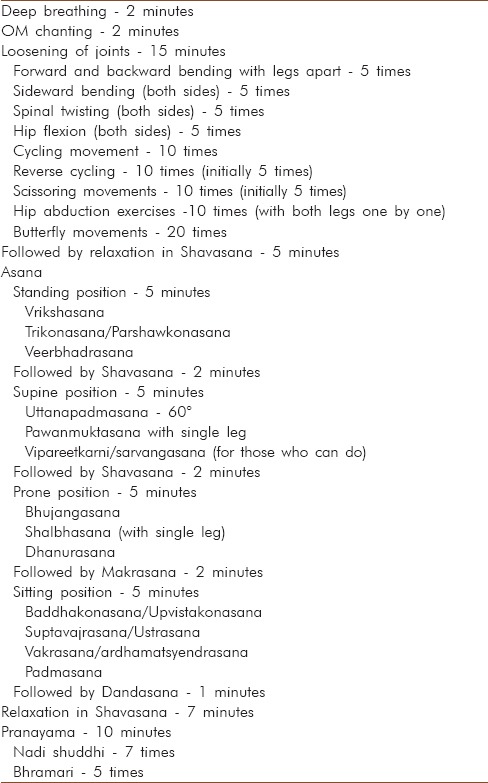
Group I received only conventional therapy in the form of analgesics mainly NSAIDS (nonsteroidal anti-inflammatory drugs) as and when required for pain (CPP). Group II subjects underwent regular supervised yogic regimen which included deep breathing, OM chanting, asana, pranayama and relaxation, etc., [Table 1] for 5 times a week for 8 weeks under the expert guidance of highly trained yoga specialists and trainers (having 5–10 years’ experience in teaching yoga possessing MD/PhD in yoga) running the yoga center in Physiology Department under Central Council for Research in Yoga and Naturopathy. All the subjects practicing yoga were beginners. They were thoroughly supervised by the instructors to carry yoga correctly. Attendance of the subjects was maintained regularly by the instructors. Yoga was performed in a quite environment in a batch of 10–15 subjects of CPP. The yoga sessions were carried out from 10 to 11 am. They also received conventional therapy in the form of NSAIDS (as and when required) for CPP.
Table 1.
The yoga regimen followed by Group II subjects
Statistical analysis
Data were analyzed by IBM SPSS Statistics 20 software (by IBM Corporation, USA). Two factors repeated measure ANOVA followed by Tukey's test at 5% level of significance. One factor is group (Group I and Group II) another factor is time (pre, post) for comparison of mean pain score and QOL scores before intervention and after intervention between the groups and within the group that is pre- and post-comparison for each group.
RESULTS
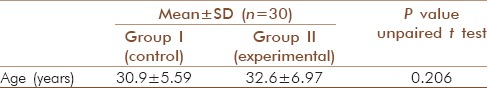
The mean age of the subjects in Group I and Group II was 30.9 ± 5.59 years and 32.6 ± 6.97 years, respectively, and they were age-matched [Table 2].
Table 2.
Comparison of age of the subjects in Group I and Group II
Visual analog scale score
At the onset of study, there was no significant difference of VAS scores between Group I (65.60 ± 5.89) and Group II (66.90 ± 8.40) subjects. After 8 weeks of intervention, Group II subjects showed a significant reduction (P < 0.001) in VAS scores (34.07 ± 10.12) as compared to Group I (67.03 ± 6.557) subjects indicating better pain reduction in Group II subjects. There was no significant difference between the pre- and post-treatment VAS scores in Group I subjects. A significant reduction was seen in posttreatment VAS scores (P < 0.001) as compared to pretreatment VAS scores in Group II subjects [Table 3]. Figure 2 depicts a comparison of VAS score before and after 8 weeks of intervention in Group I and Group II.
Table 3.
Comparison of VAS scores before (pre) and after 8 weeks of intervention (post) in Group I and Group II
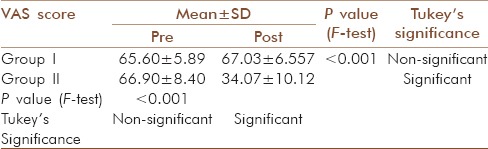
Figure 2.
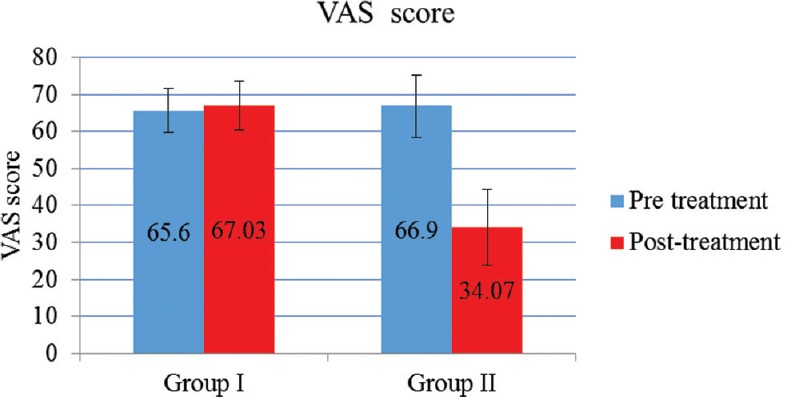
Comparison of VAS score before and after 8 weeks of intervention in Group I and Group II
Quality of life
There was a significant difference between the pretreatment and posttreatment values of WHOQOL-BREF transformed scores (P < 0.001) in various (physical, psychological, social, and environmental) domains in Group II subjects. WHOQOL-BREF scores increased significantly in Group II after yogic intervention as compared to the Group I subjects [Tables 4–7]. Figures 3–6 depicts the comparison of the WHOQOL-BREF transformed scores in the physical, psychological, social, and environmental domain, respectively, before and after 8 weeks of intervention in Group I and Group II subjects.
Table 4.
Comparison of the WHOQOL-Bref transformed scores in the Physical domain before (PRE) and after 8 weeks of intervention (POST) in Group I and Group II
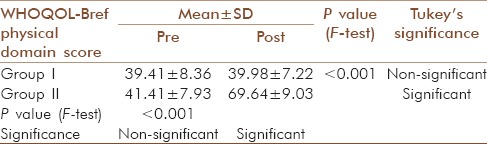
Table 7.
Comparison of the WHOQOL-Bref transformed scores in the Environmental domain before (pre) and after 8 weeks of intervention (post) in Group I and Group II
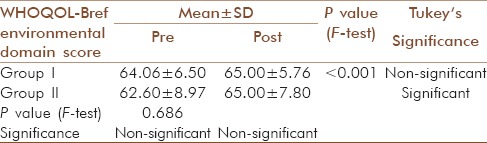
Figure 3.
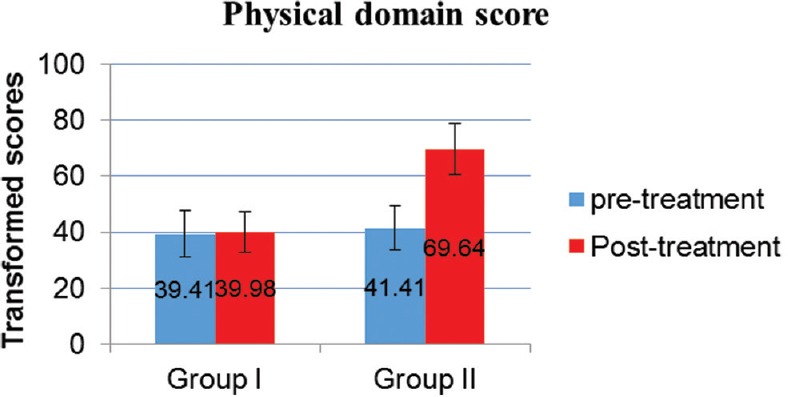
Comparison of the WHOQOL-Bref transformed scores in the physical domain before and after 8 weeks of intervention in Group I and Group II
Figure 6.
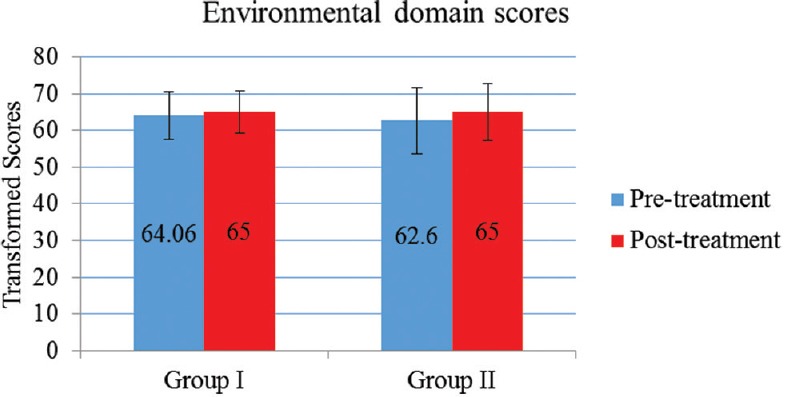
Comparison of the WHOQOL-Bref transformed scores in the Environmental domain before and after 8 weeks of intervention in Group I and Group II
Table 5.
Comparison of the WHOQOL-Bref transformed scores in the psychological domain before (pre) and after 8 weeks of intervention (post) in Group I and Group II
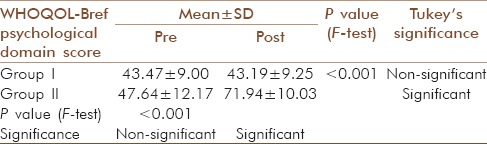
Table 6.
Comparison of the WHOQOL-Bref transformed scores in the Psychological domain before (pre) and after 8 weeks of intervention (post) in Group I and Group II
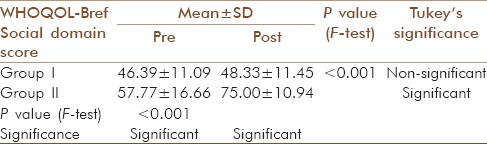
Figure 4.
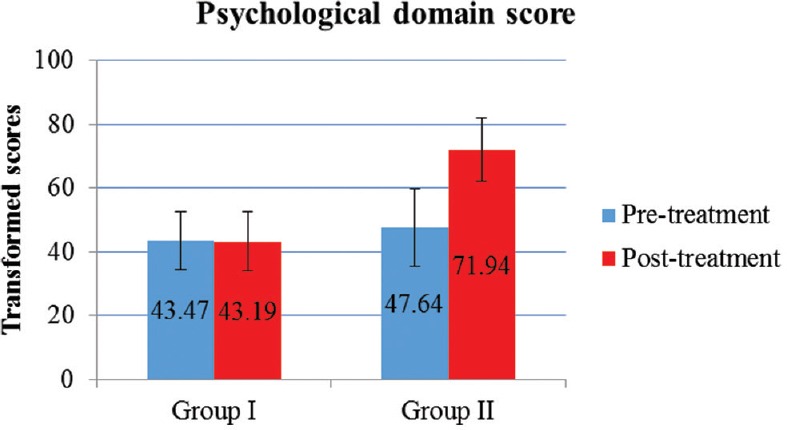
Comparison of the WHOQOL-Bref transformed scores in the psychological domain before and after 8 weeks of intervention in Group I and Group II
Figure 5.
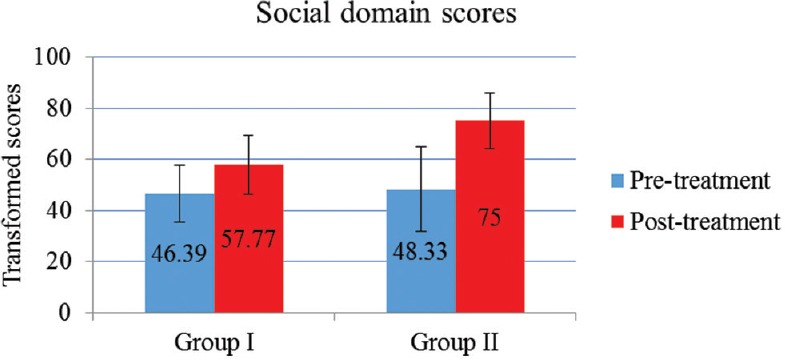
Comparison of the WHOQOL-Bref transformed scores in the Social domain before and after 8 weeks of intervention in Group I and Group II
DISCUSSION
Yoga and pain score
In the present study, 8 weeks of yogic intervention resulted in statistically significant decrease in the VAS scores, in CPP patients. However, no significant changes in VAS scores were seen in CPP patients receiving only conventional therapy (Group I). The difference in VAS scores between CPP patients on conventional therapy (Group I) and CPP patients on conventional + yoga therapy (Group II) postintervention were also significant. Decrease in VAS score is suggestive of decrease in pain intensity after 8 weeks of yoga therapy. Pain relief in gynecological conditions after yoga therapy has been reported in many studies. On extensive literature survey, we could not come across any of the study highlighting the role of yogic intervention on CPP patients. Hence, we do not have a similar study to compare our results. However, yoga nidra therapy of 6 months significantly reduced the pain symptoms in women with dysmenorrhea.[23] Moreover, practicing yoga poses (asana) significantly reduced severity and duration of dymenorrhea.[16] Other studies showing the effect of yoga on other painful conditions are also available. Yoga therapy for 5 times, 4 weeks a week, significantly improved VAS score in patients with myofascial pain syndrome.[24] Practicing yoga asana for 4 weeks led to significant reduction of VAS scores in chronic low back pain patients.[25] Moreover, yoga training reduced the intensity and frequency of headaches in patients suffering from migraine.[26] After 12 weeks of yoga intervention, which included various asana, women with chronic low back pain showed a significant reduction in VAS scores of pain, significant increase in back flexibility, and significant increase in brain-derived neurotropic factor (BDNF). This increase in BDNF could be attributed to pain reduction in patients with chronic pain.[27] Yoga therapy enhances the tone of muscles and helps in releasing of muscle tension. Relaxation exercises performed during yoga leads to reduction of stress-related muscle tension and also modify neurobiological pain perception which could be a mechanism for pain reduction.[28] Increase in BDNF and improvements in the pelvic muscle tone after yoga therapy might be responsible for pain relief in CPP patients.
Yoga and quality of life in chronic pelvic pain patients
There was a significant improvement in QOL after 8 weeks of yoga therapy. Improvement was seen in all domains, i.e., physical, psychological, social, and environmental domain. However, no significant change in QOL scores was seen in CPP patients receiving only conventional therapy (Group I). The difference in QOL scores between CPP patients on conventional therapy (Group I) and CPP patients on conventional + yoga intervention (Group II) posttreatment was also significant in physical, psychological, and social domain. Studies have shown that practicing yoga causes a significant improvement of QOL not only in painful conditions but also in various other medical illnesses. It was seen that yogic intervention (comprising of asana, pranayama, meditation, and lectures on yoga philosophy) in patients with chronic low back pain led to improvement in the QOL in all the four domains of WHOQOL-BREF.[13] Yoga training was helpful in improving QOL in all domains of women with perimenopausal symptoms.[29,30] Reduction in the pain intensity and frequency might have led to the improvement of QOL in physical domain and increase in brain GABA levels may be a cause for psychological and social QOL improvement.[31]
Hence, improvement in pelvic and abdominal muscle tone and increase in the levels of BDNF along with brain GABA levels (as shown by previous studies) by yoga therapy may perhaps be attributed for the significant reduction in VAS score and improvement in QOL in CPP patients on yoga therapy.
CONCLUSION
From this study, it can be concluded that after 8 weeks of yoga therapy, Group II CPP subjects had lesser intensity of pain as shown by significantly reduced VAS scores and improved QOL with a significant increase in physical, psychological, and social domain scores of WHOQOL-BREF. Hence, yoga regimen used in our study can be a used as add-on treatment for the pain relief and for improving QOL in patients of CPP. Better pain management with yoga can help reduce dependence on NSAIDS and its associated side effects.
Limitations of our study
This study was conducted in limited time period and the assessment of the parameters was done twice before and after study. If the study had been of a longer duration, multiple assessments would have been possible at regular intervals and then the trends of changes and long-term effects on yoga on CPP patients could have been determined. Further, we could not assess the levels of biochemical markers, i.e., brain-derived neurotropic factor (BDNF) and GABA because of resource crunch. Levels of these markers would have helped us to validate our findings more scientifically. Further work needs to be done in this field with a larger sample size and a longer follow-up to increase the efficacy and therapeutic value of the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
My sincere thanks to Dr. Jyoti Chauhan, Mr. Ashish Mishra, Dr. Krishan Kumar Goswami, and Mr. Tika Ram at Yoga and Naturopathy OPD and Lifestyle Intervention Center, UCMS and GTB Hospital, Delhi under Central Council for Research in Yoga and Naturopathy, Ministry of AYUSH for teaching and supervising the subjects doing yoga. My special thanks to all those patients participating in our study.
REFERENCES
- 1.Zondervan KT, Yudkin PL, Vessey MP, Dawes MG, Barlow DH, Kennedy SH. Prevalence and incidence of chronic pelvic pain in primary care: Evidence from a national general practice database. Br J Obstet Gynaecol. 1999;106:1149–55. doi: 10.1111/j.1471-0528.1999.tb08140.x. [DOI] [PubMed] [Google Scholar]
- 2.Bordman R, Jackson B. Below the belt: Approach to chronic pelvic pain. Can Fam Physician. 2006;52:1556–62. [PMC free article] [PubMed] [Google Scholar]
- 3.Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS. WHO systematic review of prevalence of chronic pelvic pain: A neglected reproductive health morbidity. BMC Public Health. 2006;6:177. doi: 10.1186/1471-2458-6-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grace V, Zondervan K. Chronic pelvic pain in women in New Zealand: Comparative well-being, comorbidity, and impact on work and other activities. Health Care Women Int. 2006;27:585–99. doi: 10.1080/07399330600803725. [DOI] [PubMed] [Google Scholar]
- 5.Yuan CC. Laparoscopic uterosacral nerve ablation and chronic pelvic pain. J Chin Med Assoc. 2006;69:101–3. doi: 10.1016/S1726-4901(09)70185-6. [DOI] [PubMed] [Google Scholar]
- 6.Howard FM. Chronic pelvic pain in women. Am J Manag Care. 2001;7:1001–11. [PubMed] [Google Scholar]
- 7.Zhu X, Hamilton KD, McNicol ED. Acupuncture for pain in endometriosis. Cochrane Database Syst Rev. 2011;9:CD007864. doi: 10.1002/14651858.CD007864.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iftikhar R. Outcome of laparoscopy in chronic pelvic pain. J Surg Pak. 2008;13:155–8. [Google Scholar]
- 9.Haggerty CL, Schulz R, Ness RB. PID Evaluation and Clinical Health Study Investigators. Lower quality of life among women with chronic pelvic pain after pelvic inflammatory disease. Obstet Gynecol. 2003;102(5 Pt 1):934–9. doi: 10.1016/s0029-7844(03)00695-1. [DOI] [PubMed] [Google Scholar]
- 10.Mathias SD, Kuppermann M, Liberman RF, Lipschutz RC, Steege JF. Chronic pelvic pain: Prevalence, health-related quality of life, and economic correlates. Obstet Gynecol. 1996;87:321–7. doi: 10.1016/0029-7844(95)00458-0. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz DD. Chronic pelvic pain in women. Am Fam Physician. 2008;77:1535–42. [PubMed] [Google Scholar]
- 12.Trakroo M, Bhavanani AB, Pal GK, Udupa K, Krishnamurthy N. A comparative study of the effects of asan, pranayama and asan-pranayama training on neurological and neuromuscular functions of Pondicherry police trainees. Int J Yoga. 2013;6:96–103. doi: 10.4103/0973-6131.113398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tekur P, Chametcha S, Hongasandra RN, Raghuram N. Effect of yoga on quality of life of CLBP patients: A randomized control study. Int J Yoga. 2010;3:10–7. doi: 10.4103/0973-6131.66773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: A meta-analysis. J Pain. 2012;13:1–9. doi: 10.1016/j.jpain.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Koneru S, Tanikonda R. Role of yoga and physical activity in work-related musculoskeletal disorders among dentists. J Int Soc Prev Community Dent. 2015;5:199–204. doi: 10.4103/2231-0762.159957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rakhshaee Z. Effect of three yoga poses (Cobra, cat and fish poses) in women with primary dysmenorrhea: A randomized clinical trial. J Pediatr Adolesc Gynecol. 2011;24:192–6. doi: 10.1016/j.jpag.2011.01.059. [DOI] [PubMed] [Google Scholar]
- 17.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psychol Med. 1988;18:1007–19. doi: 10.1017/s0033291700009934. [DOI] [PubMed] [Google Scholar]
- 18.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain. 1997;72:95–7. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 19.Sriwatanakul K, Kelvie W, Lasagna L, Calimlim JF, Weis OF, Mehta G. Studies with different types of visual analog scales for measurement of pain. Clin Pharmacol Ther. 1983;34:234–9. doi: 10.1038/clpt.1983.159. [DOI] [PubMed] [Google Scholar]
- 20.The WHOQOL Group. WHOQOL-BREF: Introduction, administration, scoring and generic version of the assessment. Field trial version. Geneva: WHO; 1996. [Google Scholar]
- 21.Skevington SM, Lotfy M, O’Connell KA WHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 22.Saxena S, Chandiramani K, Bhargava R. WHOQOL-Hindi: A questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160–5. [PubMed] [Google Scholar]
- 23.Rani K, Tiwari SC, Singh U, Agrawal GG, Srivastava N. Six-month trial of Yoga Nidra in menstrual disorder patients: Effects on somatoform symptoms. Ind Psychiatry J. 2011;20:97–102. doi: 10.4103/0972-6748.102489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharan D, Manjula M, Urmi D, Ajeesh P. Effect of yoga on the Myofascial Pain Syndrome of neck. Int J Yoga. 2014;7:54–9. doi: 10.4103/0973-6131.123486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nambi GS, Inbasekaran D, Khuman R, Devi S, Shanmugananth E, Jagannathan K. Changes in pain intensity and health related quality of life with Iyengar yoga in nonspecific chronic low back pain: A randomized controlled study. Int J Yoga. 2014;7:48–53. doi: 10.4103/0973-6131.123481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kisan R, Sujan M, Adoor M, Rao R, Nalini A, Kutty BM, et al. Effect of yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014;7:126–32. doi: 10.4103/0973-6131.133891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee M, Moon W, Kim J. Effect of yoga on pain, brain-derived neurotrophic factor, and serotonin in premenopausal women with chronic low back pain. Evid Based Complement Alternat Med. 2014;2014:203173. doi: 10.1155/2014/203173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crow EM, Jeannot E, Trewhela A. Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: A systematic review. Int J Yoga. 2015;8:3–14. doi: 10.4103/0973-6131.146046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nayak G, Kamath A, Kumar PN, Rao A. Effect of yoga therapy on physical and psychological quality of life of perimenopausal women in selected coastal areas of Karnataka, India. J Midlife Health. 2014;5:180–5. doi: 10.4103/0976-7800.145161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jayabharathi B, Judie A. Complementary health approach to quality of life in menopausal women: A community-based interventional study. Clin Interv Aging. 2014;9:1913–21. doi: 10.2147/CIA.S70064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: A randomized controlled MRS study. J Altern Complement Med. 2010;16:1145–52. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]


