Abstract
Metastasis to the small bowel from a previously resected colorectal cancer is rare and may erroneously be diagnosed as a primary small bowel carcinoma. It usually occurs several years after the primary resection. We present the case of a 67-year-old man who had undergone left hemicolectomy for colon cancer 3 years earlier and returned with subacute small bowel obstruction. This was initially thought, based on preoperative radiological findings and normal colonoscopic examination, to be due a primary jejunal cancer. Even at surgery, the lesion convincingly appeared as an obstructing primary small bowel carcinoma. However, the histology of the resected small bowel revealed metastatic colon cancer. This rare and an unusual metastatic occurrence some years after the primary resection is described and reviewed.
Keywords: Colorectal cancer, Small bowel, Metastases, Complications
While small bowel cancer is rare, it may occur in patients who were previously diagnosed and surgically treated for colorectal carcinoma (CRC).1 This late metastasis may occur at distant and unusual sites, and be diagnosed erroneously as a primary small bowel carcinoma.
We present a case of subacute small bowel obstruction in an older male patient who had undergone left hemicolectomy for colon cancer 3 years earlier.
Case report
A 67-year-old man presented with 3-month history of colicky left-sided abdominal pain, which was associated with nausea, abdominal distension and constipation. He tolerated only a liquid diet only and had lost some weight. He underwent coronary artery bypass graft 10 years previously, as well as an emergency Hartman procedure for obstructing left colon cancer (T3,N0,Tx) 3 years earlier. This was followed by its reversal 3 months later. He received neither adjuvant chemotherapy nor receiving antiplatelet therapy. Prior to his referral, he underwent colonoscopy, which was reported as normal. Generally, he appeared in reasonable health, and abdominal examination revealed a midline scar with an incisional hernia, and a transverse scar in the left iliac fossa at the site of the stoma closure. There was deep tenderness in the left hypochondrium, but no palpable masses or organomegaly. Rectal examination was normal.
Routine blood investigation revealed microcytic, hypochromic anaemia (haemoglobin 10 g%), and a low albumen level (24 g/L). Carcinoembryonic antigen levels were normal. Computed tomography (CT) revealed a locally advanced jejunal lesion with proximal jejunal dilatation and enlarged mesenteric lymph nodes (Figure 1). The tumour was infiltrating the abdominal wall and the perinephric fat, and was closely adherent to the inferior pole of the spleen.
Figure 1.
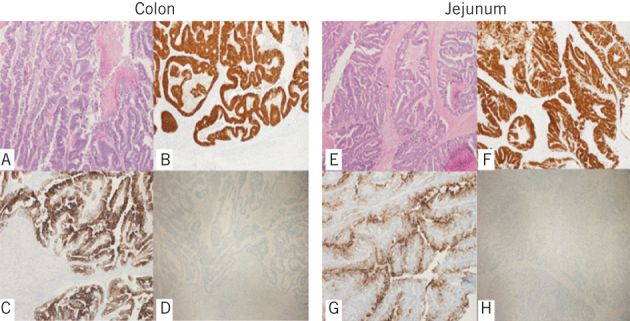
CT scan of the abdomen showing a locally advanced jejunal lesion with proximal jejunal dilatation and enlarged mesenteric lymph nodes and mesenteric stranding. The tumour was infiltrating the abdominal wall and the perinephric fat, and was closely adherent to the inferior pole of the spleen.
Total parenteral nutrition was started and, following cardiac evaluation, the patient underwent exploratory laparotomy. This showed dense adhesions and a dilated proximal jejunum, alongside collapse of the distal jejunum and ileum. The tumour was mobilized and widely resected with an end-to-end small bowel stapled anastomosis (Figure 2).
Figure 2.
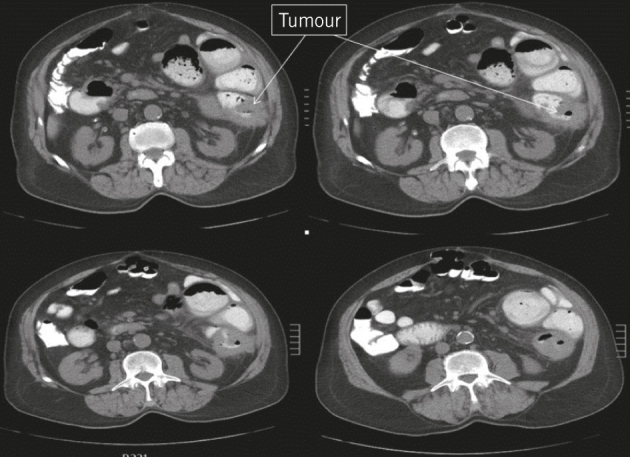
The resected jejunal lesion. Histopathology revealed this to be a metastatic lesion from a previously resected left colon cancer 3 years earlier.
On the forth postoperative day, the patient complained of abdominal distension, and his blood pressure and haemoglobin levels dropped suddenly. He was taken for re-exploration, during which blood clots in the paracolic gutter and pelvis were evacuated and haemostasis was secured. His postoperative recovery was thereafter smooth, except for elevated cardiac enzymes and very high troponin 2 levels, indicating myocardial infarction. On the fouth day after the second exploration, he developed a low-output enterocutaneous fistula, which closed spontaneously after 4 weeks of conservative treatment. He was discharged home in reasonable general health.
Histology revealed moderately differentiated metastatic colonic adenocarcinoma, with 15 lymph nodes negative for malignancy. Revision of the colonic lesion histology (Figures 3A–D) and that of the resected small bowel lesion (Figures 3E–H) showed malignant epithelial neoplasm, with complex glandular architecture and intraluminal necrosis (Figures 3A and E), which is typical of colonic adenocarcinoma. Both lesions shared the same immunohistochemical reactivity pattern of colonic adenocarcinoma, with diffuse and strong positive staining for anti-CDX2 (Figures 3B and F), positive staining for anti-CK20 (Figures 3C and G), and negative staining for anti-CK7 (Figures 3D and H).
Figure 3.
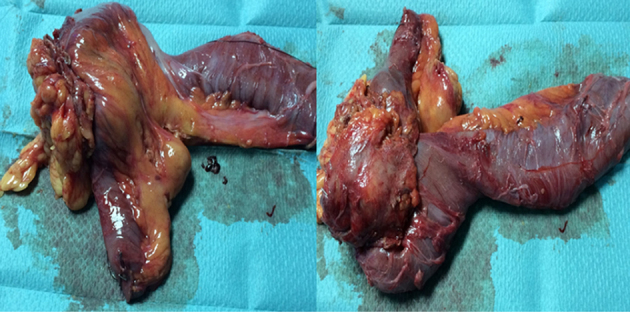
Histological examination of the colonic lesion (left panel) and small intestine lesion (right panel) showing a malignant epithelial neoplasm with complex glandular architecture and intraluminal necrosis; findings typical of colonic adenocarcinoma (A and E). Both lesions share the same immunohistochemical reactivity pattern of colonic adenocarcinoma: diffuse and strong positive staining for anti-CDX2 (B and F); positive staining for anti-CK20 (C and G); and negative staining for anti-CK7 (D and H). (Hematoxylin-eosin, magnification x40 (A and E); immune-stains for CDX2 (B and F), CK20 (C and G) and CK7 (D and H), magnification x40).
The decision of the multidisciplinary tumour board was to start chemotherapy; this was refused by the patient, however. He remained well, with no recurrence at 18-month follow-up.
Discussion
Although distant CRC metastasis to unusual sites many years after the primary resection is relatively rare, it has been reported.1 Sites included the small bowel, ureter, brain, kidney and thyroid.2 and it is thought that this wide distribution may be due to haematogenous spread. The incidence of metastases to the small bowel in autopsy cases is 2.8–8.2%.3 The presenting symptoms are vague abdominal cramps, but obstructive symptoms such as colicky pain, distension, vomiting and constipation may predominate. Other presentations include weight loss, ileus and obscure gastrointestinal bleeding with chronic anaemia.4 The diagnosis is often made on a small bowel series or CT. However, neither can differentiate a primary form a metastatic small bowel cancer. Obscure gastrointestinal bleeding can be localised by capsule enetroscopy and diagnosed in some cases by balloon-assisted enetroscopy.5 In this case, capsule enetroscopy was not considered due to the obstructive nature of the lesion and the inevitable need for surgical resection, regardless of the diagnosis.
Although radical surgical resection of such late colorectal metastasis is reportedly associated with a good quality of life, postoperative complication rates are considered to be high, at approaching 80%, and survival is short (ranging from 2–15 months),2 although survival of up to 11 years has been reported.4 This case lends support to this unfavourable picture, as our patient experienced a number of serious postoperative complications, including intraabdominal bleeding, cardiac infarction and enetrocutaneous fistula.
There are a number of similar cases in the literature of metastatic CRC to the small bowel presenting years after the primary cancer resection. Kojima et al reported the case of 68-year-old female with recurrent ileus and anemia 2 years after left colectomy for CRC.4 Resection of the ileal tumour revealed adenocarcinoma of colonic origin, after which the patient survived for more than 11 years.4 Thoma et al reported three cases of metastatic CRC to the small bowel, all of which presented with obscure gastrointestinal bleeding 1.3–7 years after the primary CRC resection. The diagnosis was made by capsule enteroscopy and double balloon enteroscopy.5 A Japanese survey identified six cases of metastatic small bowel tumours derived from CRC, consisting of four males and three females aged 60–80 years.4 In two cases, the tumours were synchronous, while the small bowel metastases appeared between 1.6–9 years (mean 3.6 years) in the remaining four. The most common site for metastases was the ileum, and all patients were alive at 6–30 months, with no recurrence or metastases.4
Our case highlights the late occurrence, potentially several years after the resection of the primary CRC, of colorectal metastases to unusual sites such as the small bowel. This metastasis may also masquerade as a primary small bowel cancer.
Acknowledgment
The authors have no competing nor conflict of interests, nor financial disclosures, to declare.
References
- 1.Huerta S, Li HC. Small bowel obstruction due to metastatic colon cancer. Anticancer Drugs 2009; : S15–18. [DOI] [PubMed] [Google Scholar]
- 2.Tomita R, Fujisaki S, Sakurai K et al. . [Malignant small bowel ileus caused by local recurrence after colorectal cancer surgery]. Gan To Kagaku Ryoho 2013; : 1942–1943. [PubMed] [Google Scholar]
- 3.Routh A, Hickman BT. Metastatic tumors of the small intestine: case report and review of literature. J Miss State Med Assoc 1984; : 235–236. [PubMed] [Google Scholar]
- 4.Kojima Y, Matsumoto F, Mikami Y et al. . Metastatic Small Bowel Tumor from Descending Colon Cancer with Extensive Hematogenous or Lymphogenous Spread: Survey of the Japanese Literature. Case Rep Gastroenterol 2010; : 340–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thoma MN, Saiyed SM, Charles RJ. Metastatic colorectal cancer to the small bowel-an uncommon cause of obscure GI bleeding: a three-case experience with review of the literature. J Gastrointest Cancer 2011; : 119–122. [DOI] [PubMed] [Google Scholar]


