Abstract
Background
Few studies have addressed retention of minorities, particularly African Americans, in longitudinal research. Our aim was to determine whether there was differential retention between African Americans and Whites in the ARIC cohort and identify cardiovascular disease (CVD) risk factors and indicators of socioeconomic status (SES) associated with these retention differences.
Methods
15,688 participants, 27% African American and 73% White, were included from baseline, 1987-1989, and classified as having died, lost or withdrew from study contact, or remained active in study calls through 2013. Life tables were created illustrating retention patterns stratified by race, from baseline through visit 5, 2011-2013. Prevalence tables stratified by race, participation status, and center were created to examine CVD risk factors and SES at baseline and visit 5.
Results
54% of African Americans compared with 62% of Whites were still in follow-up by 2013. This difference was due to an 8% higher cumulative incidence of death among African Americans. Those who remained in follow-up had the lowest baseline CVD risk factors and better SES, followed by those who were lost/withdrew, then those who died. Whites had lower levels of most CVD risk factors and higher SES than African Americans overall at baseline and visit 5; though, the magnitude of visit 5 differences was less.
Conclusions
In the ARIC cohort, retention differed among African Americans and Whites, but related more to mortality differences than dropping-out. Additional research is needed to better characterize the factors contributing to minority participants’ recruitment and retention in longitudinal research.
Keywords: Attrition, Race, Prospective Cohort, CVD Risk Factors, SES
Introduction
In recent decades, efforts have been made to include diverse populations in clinical research. These efforts are important in order to fully understand the disease processes and causes of persistent health disparities among historically underrepresented groups, particularly African Americans.1 Many of the existing studies examining how to encourage minorities to participate in research only address recruitment strategies and not retention. A meta-analysis of 95 reports analyzing recruitment and retention of racial/ethnic minorities in clinical research found only 13% involved longitudinal or multi-wave studies.2 Of these longitudinal and multi-wave reports, the majority were clinical trials or prevention trials with relatively short follow-up periods.2 Health disparities cannot be understood or adequately addressed without understanding how to recruit and retain minorities in medical research.
The Atherosclerosis Risk in Communities (ARIC) Study, a predominantly biracial longitudinal cohort of men and women, provides an opportunity to examine retention of African American study participants over a 27-year follow-up period and identify some factors associated with retention in comparison with Whites.
Methods
Between 1987 and 1989, 15,792 participants were enrolled into the ARIC prospective cohort using probability sampling of individuals, aged 45 to 64 years, from Forsyth County, NC, Jackson, MS, the northwestern suburbs of Minneapolis, MN, and Washington County, MD.3 African Americans only were recruited in Jackson, whereas the Minneapolis and Washington County samples were overwhelmingly White. The Forsyth County sample included both Whites and African Americans. A previous report showed that initial recruitment and baseline participation in the ARIC cohort was 46% for African Americans and 67% for Whites, and factors associated with lower participation included lower education, smoking, lower income, and reporting poor overall health.4 The differences in cardiovascular risk factors between respondents and non-respondents were greater among Whites than among African Americans.4 Among those who did participate at ARIC baseline, African Americans had higher prevalence of many cardiovascular risk factors than did Whites.5
Following cohort participants’ informed consent, ARIC assessed cardiovascular disease (CVD) and CVD risk factors at up to five clinic visits (1987-89, 1990-92, 1993-95, 1996-98, 2011-13) with occasional additional visits for ancillary examinations in subsets of the cohort. These visits typically lasted 3-6 hours and included interviews, physical examinations, and imaging studies. Of note, there were two additional opportunities for brain imaging in African Americans. In an ongoing fashion, ARIC also conducted annual or semi-annual telephone follow-up contacts, lasting about 15 minutes, to enhance retention and to identify incident and fatal events. Although all study procedures were standardized, interviewer techniques were tailored to the needs of individual communities. The two ARIC centers with African American participants used a variety of strategies to encourage continued cohort attendance, including participation appreciation events, community engagement efforts, and race-matched recruiters, interviewers, and clinical exam staff (Table 1).
Table 1. Strategies used for ARIC retention, 1987-2013.
| General Promotion |
| Highlighted National Institutes of Health and University sponsorship and created an ARIC identity with a study logo |
| Promoted the altruistic and personal benefits of participation in important health research. |
| Issued periodic press releases about ARIC or its findings |
| Created a study website and referred to information therein |
| Conducted occasional town meetings with the cohort (some centers) |
| Mailed a study newsletter periodically and sent annual birthday cards |
| Techniques to Maintain Contact |
| Obtained and updated participants’ contact information at examinations |
| 15-minute phone calls to maintain contact annually to semi-annually |
| If required, made multiple attempts to contact participants when telephoning |
| Traced participants via commercial sources when need be |
| Left open the opportunity to return to the study if participation became temporarily difficult |
| Involved proxy telephone respondents when cohort members needed help |
| Specific Examination Strategies |
| Made every attempt to minimize participant time and burden by keeping exams short lasting 3-6 hours |
| Ensured staff diversity and professionalism |
| Offered transportation to examinations as the cohort aged |
| Offered financial incentives to participate in later years |
| Provided a snack and study tokens (eg, refrigerator magnets, water bottles) |
| Returned clinically relevant examination results to participants and their health providers |
| Thanked participants often, offered respect and appreciation, and reminded participants of their importance to the research. |
For the analyses presented in this article, we excluded non-White and non-African American participants, leaving 15,688 individuals whose censoring status was tracked from baseline, 1987-89, through visit 5, 2011-13. Our first aim was to illustrate the retention rates of ARIC participants from baseline through visit 5 stratified by race. Race-specific life-tables were created, showing, over time, the proportions of participants who died, were lost/withdrew from continued contact, or remained in follow-up (ie, continued study phone calls) through 2013. The date of death was obtained and reflected in decedents’ censor dates. Censor dates for those who were lost/withdrew and for the group who remained in follow-up, were determined from the last date of known status. To ensure that those who were lost/withdrew had not died, National Death Index (NDI) searches were periodically conducted to identify deaths among cohort participants. Among those who lost/withdrew, very few were lost; the majority voluntarily withdrew from further ARIC contact. Participation rates at each of the five examination visits were plotted as the number who took part in the visit divided by the number estimated to be alive at the time.
Our second aim was to describe retention in relation to baseline characteristics. We described prevalences or means and standard deviations of socioeconomic and cardiovascular disease risk factors, including education, income, reported health, leisure and sport activity, smoking status, alcohol consumption, obesity, diabetes, hypertension, and plasma cholesterol, measured by ARIC’s standardized methods, stratified by race, by center among African Americans, and by the three retention groups. We assessed baseline prevalences stratifying African Americans by center to highlight the heterogeneity within the race group. Characteristics of participants from these two centers notably differed and stratification offered a more nuanced view of retention differences within the African American cohort as well as between African Americans and Whites. Characteristics of White participants did not appreciably differ between centers.
Our third aim was to determine how attrition between 1987 and 2013 affected the previously reported risk factor differences observed at baseline between African Americans and Whites. We analyzed the same CVD risk factors assessed at baseline at visit 5, stratified by race, and by center among African Americans, between those who attended the visit. Stratification by center among African Americans was carried out for reasons listed above.
Results
At baseline visit 1 during 1987-89, African American participants represented 27% of the total cohort of 15,688 with 24% from Jackson, MS and 3% from Forsyth County, NC, whereas White participants represented 73%. 55% of the cohort was female, 45% male, and the mean baseline age was 54.2 years old with a range of 45 to 64 years old. By visit 5 during 2011-13, there were 6,415 total participants, 23% African American, with 22% from Jackson, MS and 1% from Forsyth County, NC, and 77% White participants. Women made up 59% of the cohort, 41% male, and the mean age was 75.8 years of age (range 66 to 90). Of those examined at ARIC visit 5, 91% of participants underwent a full clinic examination, 3% had abbreviated clinic examinations, and 6% were examined in their homes or care facilities.
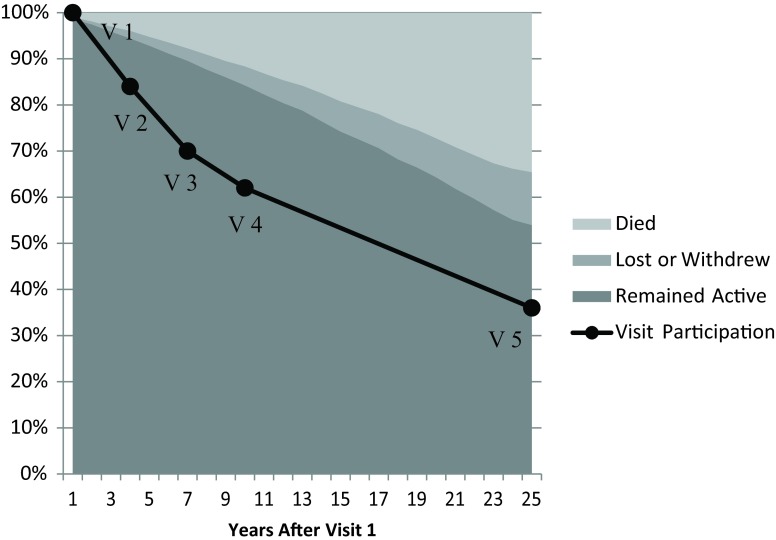
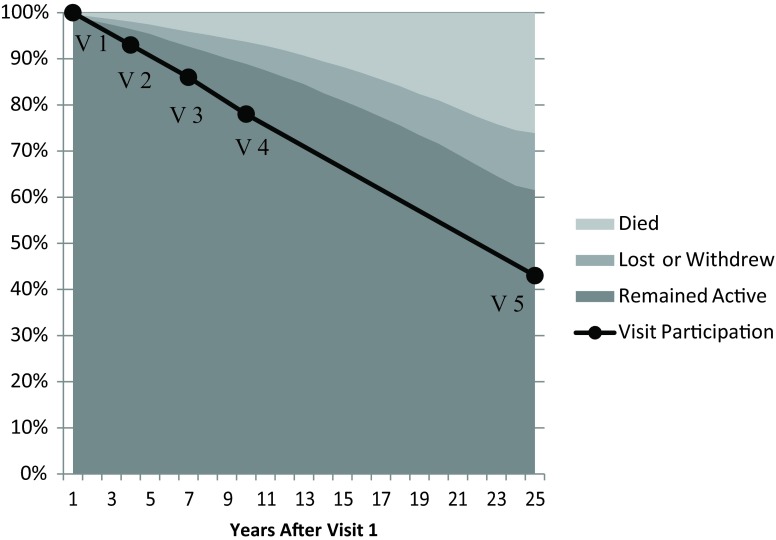
Race-specific Retention over ARIC Follow-up Period
As shown in Figure 1, among African American participants, 54% remained in follow-up by visit 5, 35% had died by or during visit 5, and 11% were lost/withdrew from the study. Among White participants (Figure 2), 62% remained in follow-up through visit 5, 26% had died by or during visit 5, and 12% were lost/withdrew from the study. Thus, overall, African Americans were less likely to still be in follow-up in the study by visit 5, mainly because they were more likely to have died over the follow-up period. African American and White participants were lost/withdrew from the study at similar proportions through the most recent exam.
Figure 1. Participation of African Americans through visit 5.
Figure 2. Participation of Whites through visit 5.
Notably, participation in each of the five examination visits among those who remained in follow-up tended to be lower in African Americans than Whites (Figure 1). At visit 5, 89% of African Americans still in follow-up in ARIC completed a full or abbreviated ARIC examination, compared to 93% of Whites.
Association of Baseline CVD Risk Factors with Retention Categories
Among 4,210 African Americans at baseline (Table 2), those who died by visit 5 were, on average, the oldest, followed by those who were lost/withdrew, and those who remained in follow-up. This was true for both Jackson and Forsyth African Americans and was mirrored in the White cohort. Women made up a greater proportion of participants remaining in follow-up and a smaller proportion of those who died. Education and income were lowest among Jackson participants, followed by Forsyth County participants, and considerably lower overall than Whites. Reported health among both cohorts of African Americans was worse, on average, than the reported health of Whites. Poor health was most prevalent among those who died or were lost/withdrew.
Table 2. Prevalence of CVD risk factors at baseline visit 1, 1987 through 1989, stratified by race, center, and status at visit 5, 2011 through 2013, ARIC.
| African Americans, n=4,210 | White, n=11,478 | ||||||||
| Jackson, MS, n=3,727 | Forsyth County, NC, n=483 | ||||||||
| Remained active | Lost or withdrew | Died | Remained active | Lost or withdrew | Died | Remained active | Lost or withdrew | Died | |
| n=2,070 | n=352 | n=1,305 | n=188 | n=132 | n=163 | n=7,030 | n =1,433 | n=3,015 | |
| Age, years | 51.8 ± 5.3 | 54.9 ± 5.7 | 55.5 ± 5.8 | 52.2 ± 5.6 | 54.4 ± 6.0 | 57.6 ± 5.0 | 52.9 ± 5.4 | 55.8 ± 5.7 | 57.2 ± 5.3 |
| Women, % | 68.5 | 61.1 | 53.0 | 70.2 | 54.6 | 49.1 | 57.7 | 47.1 | 43.8 |
| Educationa <high school, % | 35.8 | 51.9 | 53.1 | 19.7 | 32.6 | 41.4 | 13.0 | 23.6 | 24.3 |
| Incomea,<$16,000, % | 51.6 | 69.3 | 70.5 | 30.3 | 50.8 | 56.4 | 12.4 | 22.9 | 22.5 |
| Reported health | |||||||||
| Excellent, % | 26.0 | 17.8 | 18.8 | 27.1 | 27.3 | 11.7 | 50.2 | 33.9 | 34.1 |
| Good, % | 50.1 | 39.1 | 42.3 | 58.0 | 41.4 | 59.1 | 42.9 | 48.1 | 47.7 |
| Fair, % | 20.5 | 33.2 | 27.8 | 13.3 | 25.0 | 21.4 | 6.0 | 13.1 | 14.5 |
| Poor, % | 3.5 | 9.9 | 11.0 | 1.6 | 6.3 | 7.8 | 0.9 | 4.9 | 3.7 |
| Low leisure and sport activity, % | 60.0 | 64.3 | 64.4 | 43.6 | 43.2 | 51.2 | 29.0 | 36.6 | 35.8 |
| Smoking, current, % | 20.8 | 33.8 | 39.1 | 32.5 | 47.7 | 46.0 | 18.7 | 31.0 | 36.0 |
| Alcohol consumption, current, % | 28.6 | 26.9 | 32.4 | 50.0 | 47.7 | 38.9 | 66.5 | 61.1 | 61.8 |
| Weightb, obese, % | 41.1 | 47.4 | 42.3 | 37.6 | 35.1 | 28.8 | 20.2 | 27.3 | 27.4 |
| Diabetesc, % | 9.3 | 36.6 | 27.1 | 6.9 | 21.4 | 22.5 | 4.0 | 14.1 | 11.4 |
| Hypertensiond, % | 48.0 | 67.8 | 67.9 | 42.3 | 47.0 | 62.4 | 21.4 | 38.7 | 35.7 |
| Taking medication, % | 37.9 | 57.7 | 49.3 | 35.6 | 41.2 | 55.8 | 20.7 | 34.4 | 34.0 |
| Total cholesterol, mg/dL | 215.0 ± 44.8 | 224.1 ± 46.5 | 214.0 ± 46.7 | 208.7 ± 41.5 | 214.8 ± 46.6 | 211.9 ± 42.8 | 212.9 ± 39.4 | 221.7 ± 43.2 | 216.8 ± 42.4 |
| Hyperlipidemiae, % | 25.5 | 35.2 | 26.8 | 21.8 | 28.8 | 25.2 | 24.3 | 31.5 | 28.6 |
| Taking medication, % | 1.1 | 2.3 | 1.5 | 2.1 | 3.8 | 0.6 | 2.9 | 4.3 | 4.2 |
a. Based on self-report during visit 1.
b. Based on BMI < 18.5 kg/m2 for underweight, 18.5 – 24.9 kg/m2 for normal weight, 25 – 29.9 kg/m2 for overweight, and > 30 kg/m2 for obese at visit 1.
c. Diabetes defined as non-fasting blood glucose > 200 mg/dL, fasting blood glucose > 126 mg/dL, self-report of diabetes, or reporting takin medication for diabetes or high blood sugar at visit 1.
d. Diastolic blood pressure > 90 mm Hg, systolic blood pressure > 140 mm Hg, or use of hypertensive medication at visit 1.
e. Total cholesterol > 240 mg/dL t vist
The level of leisure activity was lowest among Jackson participants, followed by Forsyth participants, then White participants. Those who died tended to have the largest proportion with low leisure and sport activity. Among both African Americans and Whites, those who died had a higher prevalence of current smoking at baseline. Participants who remained in follow-up in ARIC tended to have less baseline obesity (not Forsyth African Americans), less prevalent diabetes, and less prevalent hypertension. These measures were more favorable for Whites than African Americans with the Jackson cohort having the highest prevalence of obesity, diabetes, and hypertension. Hyperlipidemia was slightly higher among those who were lost/withdrew than the other two retention categories, across all race and center groups.
Race Differences in CVD Risk Factors among Visit 5 Participants
Although African Americans had more attrition due to death during ARIC follow-up, the disparity in risk factors between African Americans and Whites, and between Jackson and Forsyth African Americans, seen at baseline were still apparent at visit 5 (Table 3). Among visit 5 participants, more Whites reported excellent or good health than did African Americans, while, among African Americans, more Jackson participants reported excellent health but more Forsyth participants reported good health than did those from Jackson. African Americans compared with Whites at visit 5 were more likely to have low levels of physical activity, be current smokers, but were less likely to be current drinkers. African Americans had more prevalent obesity, diabetes, and hypertension. Notably, while African Americans had higher average total cholesterol concentrations, those in the Jackson cohort had less prevalent hyperlipidemia than those in the Forsyth cohort and Whites, both of whom had prevalences of hyperlipidemia of 11%.
Table 3. Prevalence of cardiovascular disease risk factors at visit 5, 2011 through 2013, stratified by race and center, ARIC.
| African American, n=1,499 | White, n=4,916 | ||
| Jackson, MS, n=1,401 | Forsyth County, NC, n=98 | ||
| Age, years | 75.1 ± 5.2 | 75.0 ± 5.4 | 76.0 ± 5.3 |
| Women, % | 68.0 | 64.3 | 56.2 |
| Reported health | |||
| Excellent, % | 13.7 | 8.3 | 26.7 |
| Good, % | 51.0 | 75.0 | 56.7 |
| Fair, % | 31.4 | 8.3 | 14.3 |
| Poor, % | 3.9 | 8.3 | 2.3 |
| Leisure & sport activity | |||
| Low leisure & sport, % | 43.0 | 36.5 | 35.3 |
| Smoking | |||
| Current smoker, % | 6.9 | 6.5 | 5.4 |
| Alcohol consumption | |||
| Current drinker, % | 18.8 | 21.0 | 57.8 |
| Weighta | |||
| Obese, % | 46.9 | 40.7 | 31.6 |
| Diabetesb, % | 41.2 | 38.0 | 25.6 |
| Hypertensionc, % | 88.2 | 87.6 | 70.8 |
| Taking medication, % | 88.1 | 86.6 | 72.1 |
| Total cholesterol, mg/dL | 184.2 ± 40.2 | 182.9 ± 43.0 | 180.7 ± 7 |
| Hyperlipidemiad, % | 8.2 | 11.2 | 11.1 |
| Taking medication, % | 53.6 | 52.6 | 56.7 |
a .Based on BMI < 18.5 kg/m2 for underweight, 18.5 – 24.9 kg/m2 for normal weight, 25 – 29.9 kg/m2 for overweight, and > 30 kg/m2 for obese at visit 5.
b. Diabetes defined as non-fasting blood glucose > 200 mg/dL, fasting blood glucose > 126 mg/dL, self-report of diabetes, or reporting taking medication for diabetes or high blood sugar at visit 5.
c. Diastolic blood pressure > 90 mm Hg, systolic blood pressure > 140 mm Hg, or use of hypertensive medication at visit 5.
d. Total cholesterol > 240 mg/dL at visit 5.
Discussion
Retention in the ARIC cohort over the 27 years of follow-up has been good. Yet, there were differences in the proportions of White and African American ARIC participants who took part in each of the five examination visits. A main contributor to differences in retention was the 8% higher cumulative risk of death among African Americans compared with Whites despite African Americans and Whites being classified as lost/withdrew at about the same proportions. Racial differences in mortality are closely related to socioeconomic status as well as risk factors associated with CVD and total mortality.6 African Americans from Jackson and Forsyth County who died by visit 5 had the highest risk factors for CVD compared with African Americans who were lost/withdrew and those who remained in follow-up. African Americans also had higher levels of CVD risk factors at baseline than White participants overall, and this pattern persisted to ARIC visit 5.
Poorer participation in exams and poorer longitudinal retention of African American participants in cohort studies may be related to poorer health, lower socioeconomic status, as well as other social and behavioral factors that should be considered when designing and implementing longitudinal research. These differences, particularly related to mortality, require changes to study design as well as analysis to fully account for potential bias. While there are effective statistical methods to deal with censoring, such as competing risks analysis and g-methods, these statistical corrections cannot remove all of the bias that may occur without addressing study design. However, there is very little research on how to effectively reduce these disparities in study recruitment and design, and once reduced, how to prevent attrition among historically underrepresented groups over long follow-up periods.7 Further, there is no evidence race alone is a determining factor in compliance and attrition rates.8 Other elements such as socioeconomic status, cultural background, age, study design, and the study investigators may all play a role in initial participation and retention across races.8 Being able to identify factors important in predicting retention among ARIC participants who remained active and those who were censored helps pinpoint how racial/ethnic subgroups differ and how these differences may affect study results.
ARIC has used a variety of strategies to boost study retention (Table 1) including annual or semi-annual telephone contact, annual birthday cards, opportunities to return to the study if participation was temporarily difficult, culturally aware and professional research staff, and returning clinically relevant examination results to participants and their healthcare providers. Despite these efforts to enhance retention, understanding the most cost-effective strategies to retain diverse study participants deserves more adequate study. A meta-analysis of 24 clinical trials that included African American participants, with follow-up times ranging from 3 months to 5 years (median of 34 months), had an average drop-out rate of 23.3%.7 Reasons for drop-out included personal obligations, loss to follow-up, non-compliance with study requirements, and monetary or other incentives for participation that participants considered too low.7 Retention strategies reported were similar to those used in ARIC and focused on building rapport with participants and maintaining frequent, thoughtful communication while trying to keep the burden of participation low.7 While the clinical trials examined were much shorter than ARIC, many of the issues surrounding retention were the same.
There are some limitations to the ARIC data. The categories for ‘remained in follow-up,’ ‘lost/withdrew,’ and ‘died’ did not take into account the completeness of participation. ARIC followed participants by telephone even if they did not attend or refused to complete an exam. Within the group that remained nominally in follow-up, there may have been important differences between those who attended every clinic exam and those who refused one or more exams. We showed that African Americans who still participated in telephone interviews were less likely to participate in clinic visits than Whites. This suggests that despite differential loss due to death between African Americans and Whites, considerations surrounding retention are still relevant in understanding the higher number of African Americans than Whites still in follow-up who are not fully participating. We also did not differentiate between those who were lost to follow-up and those who voluntarily withdrew from the study as those numbers were relatively small, but these two groups may, in fact, have important differences. Finally, we could not study other ethnic groups due to their small numbers. It is unclear whether the differences in retention seen in African Americans would apply to other race-ethnic groups.
Conclusion
Examination of factors associated with retention among the African American and White ARIC participants over the course of an extended follow-up revealed that disparities evident during the baseline study visit persisted and may have contributed to differential retention rates. Unbiased assessment of the association of risk factors with outcomes in diverse longitudinal cohorts requires employment of targeted population-sensitive retention strategies and detailed assessment of factors that may contribute to differential attrition.
References
- 1.Heiat A, Gross CP, Krumholz HM. Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med. 2002;162(15):1682-1688. 10.1001/archinte.162.15.1682 [DOI] [PubMed] [Google Scholar]
- 2.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27(1):1-28. 10.1146/annurev.publhealth.27.021405.102113 [DOI] [PubMed] [Google Scholar]
- 3.The ARIC investigators . The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687-702. 10.1093/oxfordjournals.aje.a115184 [DOI] [PubMed] [Google Scholar]
- 4.Jackson R, Chambless LE, Yang K, et al. ; The Atherosclerosis Risk in Communities (ARIC) Study Investigators . Differences between respondents and nonrespondents in a multicenter community-based study vary by gender ethnicity. J Clin Epidemiol. 1996;49(12):1441-1446. 10.1016/0895-4356(95)00047-X [DOI] [PubMed] [Google Scholar]
- 5.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD; ARIC Study Investigators . Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690-1696. 10.1016/j.jacc.2010.11.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States, 1970-1990: gender, racial, and educational differences. Soc Sci Med. 2001;52(11):1629-1641. 10.1016/S0277-9536(00)00273-2 [DOI] [PubMed] [Google Scholar]
- 7.Otado J, Kwagyan J, Edwards D, Ukaegbu A, Rockcliffe F, Osafo N. Culturally competent strategies for recruitment and retention of African American populations into clinical trials. Clin Transl Sci. 2015;8(5):460-466. 10.1111/cts.12285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005;111(10):1332-1336. 10.1161/01.CIR.0000158134.24860.91 [DOI] [PubMed] [Google Scholar]