Abstract
Purpose
This retrospective original research was designed to illustrate the general outcome after radiofrequency (RF) neurotomy of lumbar medial branch (MB) and posterior ramus of the sacroiliac joint of 160 patients with chronic low back pain (LBP) 1, 6, and 12 months after treatment.
Methods
Visual Analog Scale (VAS) 0–10 pain scores, quality of life, body mass index (BMI), medication usage, and frequency of physical exercise/sports participation (none, 1–3×/week, more) were collected before the procedure, at 1 month post procedure (n=160), and again at 6 (n=73) and 12 months (n=89) post procedure.
Results
A VAS decrease of 4 points on a 10-point scale (from 8 to 4) in the overall group was seen after 6 months and of 4.5 after 12 months. Lower medication usage was reported, with opioids decreased by 40% and nonsteroidal anti-inflammatory drugs (NSAIDs) by 60%. Decreased pain lasted for 12 months. Significantly better outcomes were reported by patients with BMIs <30. No gender-specific differences occurred in the reported decrease in VAS. Analysis of the “no-sports” group versus the more active (1–3 times weekly sports) group showed a better pain decrease after 1 year in the active group.
Conclusion
The data suggest RF treatment for chronic LBP that can lead to long-term improvement. Patients with a BMI >30 are less likely to report decreased pain. The better long-term pain relief in the sports participating group is a motivation for the authors to keep the patients in motion.
Keywords: radiofrequency, low back pain, BMI, sacroiliac joint, gender, sports, cooled RF neurotomy
Introduction
The prevalence of facet joint (FJ)-mediated low back pain (LBP) is between 31% and 45%,1,2 and the prevalence of sacroiliac joint (SIJ) as a source of chronic axial LBP is reported to be between 18% and 30%.3
One of the treatment options of FJ-mediated LBP is the use of radiofrequency (RF) neurotomy and cooled RF (Sinergy, Halyard Health, Alpharetta, GA, USA) for the treatment of SIJ-mediated LBP.
The results reported in studies of FJ-mediated LBP RF treatment are inconsistent. Negative results have been reported in studies that had inappropriate patient selection or used surgically unsuitable techniques.4–6 Studies that were well designed and conducted on appropriately selected groups of patients have shown positive outcomes that cannot be explained by the placebo effect. Inappropriate conclusions have been drawn by systematic reviews of invalid studies, leading to the acceptance of poor evidence against the efficacy of lumbar medial branch (MB) neurotomy. This has led to clear misrepresentations of the data that exist to support this therapeutic approach to LBP.7,8
The long-term efficacy of cooled RF (SInergy) treatment of SIJ-mediated LBP has been reported previously in a retrospective case series of 126 patients.9 The evidence for cooled RF neurotomy is also substantial10 and has been illustrated in placebo-controlled studies.11,12
Nevertheless, there are limited data addressing predictive factors, such as body mass index (BMI), comorbidities, and gender. The usage of double MB blocks as diagnostic and predictive elements is accepted and well documented.13–15 One study showed that depression appears to be a limiting factor in the success of the therapy. The success rate in this study was low in all groups, with the use of a 20-G cannula, and although the authors described using the Spine Intervention Society (SIS) technique, the success rate after 6 months (32%) and 12 months (22%) does not correspond to the results seen in other studies using the SIS technique.16
Objective
This retrospective study was designed to investigate general outcomes after RF neurotomy of lumbar MB or lateral branch (LB) neurotomy of SIJ in patients with chronic LBP at 1, 6, and 12 months after treatment. Outcomes were stratified by BMI, gender, and age. The effects of these treatments on opioid and nonsteroidal anti-inflammatory drug (NSAID) usage were determined. These data were analyzed to determine the predictive nature of BMI, gender, and sports activity on the success rate of RF treatment for FJ- and SIJ-mediated LBP.
Methods
The records of 160 patients with chronic LBP who underwent treatment with RF MB neurotomy (Figure 1; parallel needle technique) and/or cooled RF lateral branch neurotomy (LBN) (Figure 2) in case of SIJ-mediated LBP were identified. These study subjects were selected for treatment based on physical examination (PE) and positive response (>50% pain relief) to a lumbar MB block (Figure 3) and/or dorsal ramus (DR) L5 block or intra-articular SIJ block (Figure 4). Lumbar MB L3 and L4 and the L5 DR were lesioned by the SIS parallel needle technique (n=43). Cooled RF LBN involved lesioning the L5 DR and the lateral branches of the S1–S3 dorsal rami for the treatment of SIJ pain (n=109). Visual Analog Scale (VAS) pain scores, quality of life, BMI, medication usage, and satisfaction with pain management were collected before the procedure, at 1 month post procedure (n=160), and again at 6 (n=73) and 12 months (n=89) post procedure.
Figure 1.
L4 medial branch neurotomy.
Figure 2.

Sacroiliac joint cooled radiofrequency neurotomy.
Figure 3.

L4 medial branch block.
Figure 4.
Intra-articular fluoroscopy-guided sacroiliac joint block.
Study design
This research project enrolled a total of 160 study subjects included the following 3 groups:
Group 1 (n=43): MB lumbar FJ L4/5 and L5/S1, MB L3, L4, and DR (dorsal ramus) L5 (SIS technique, parallel needle placement, 18G curved needle, 90 seconds at 80°C).
Group 2 (n=109): cooled RF treatment of the SIJ, SIJ LB of the posterior rami S1–S3, and rami dorsalis of L5 (Halyard Health SInergy System). All procedures were done after a positive response of >50% pain relief to a single MB block (1 mL 2% lidocaine and 0.3 mL iopamidol) or intra-articular fluoroscopy-guided SIJ block (1.5 mL 2% lidocaine and 0.3–0.5 mL iopamidol) after clinical signs during the PE of having a FJ/SIJ pain syndrome.
Group 3 (n=8): other regions treated as appropriate for their disease process.
Subgroups were divided according to 1-, 6-, and 12-month follow-up data. Subjects were instructed to complete a diary form documenting medication usage and pain (sent back anonymously in a prepaid envelope) at 6 and 12 months post-RF treatment of the SIJ and/or lumbar FJs. Approval was received from the Ethics Committee of the government of Upper Austria (Ethikkomission des Landes Oberosterreich, Nr. K-29–13, 2013-05-27). Written informed consent was obtained for the use of each subject’s data.
To be treated with RF neurotomy, the study subjects needed to present with the following characteristics: 1) chronic LBP for ≥6 months; 2) a VAS pain score of ≥6; 3) pain localized in the FJ/SIJ region; 4) signs and symptoms of FJ/SIJ-mediated LBP upon PE (e.g., Patrick’s test, distraction, compression test, pain below L5, and lateral and dorsal thigh pain); 5) failure to achieve adequate improvement with conservative noninvasive treatments previously; and 6) >50% pain relief from a single fluoroscopically confirmed intra-articular SIJ injection (1.5 mL 2% lidocaine plus 0.3–0.5 mL iopamidol 200 mg/mL) and 1 mL 2% lidocaine and 0.3 mL iopamidol 200 mg/mL as a MB block (L3–L4) and DR L5 block.
Patients were excluded from the study if they received pain relief for longer than what could be achieved with lidocaine (1–2 hours). Furthermore, study subjects were asked before treatment about their maximal and minimal daily pain and the relationship between activity and pain increases or decreases. After the test block, in order to examine the relationship between pain provocation (pain with movement) and the resulting pain reports, the subjects were required to fill out a diary noting their pain level on the VAS every 30 minutes for ~6 hours. The test block was accepted as positive if there was at least a 50% decrease in pain reported for the duration of the lidocaine effect and then having a subsequent VAS pain increase after the medication effect dissipated.
Study subjects were treated at Medizinisches Zentrum SchmerzLOS Linz, Austria, Medizinisches Zentrum SchmerzLOS, Baden/Vienna, Austria, and Private Hospital Döbling, Vienna, Austria. Minimal sedation was used, allowing the patient to communicate for the duration of the procedure.
All subjects were provided with a diary with forms for self-reporting of data collected at 1, 6, and 12 months post treatment. These forms inquired about quality of life (much better, better, same, or worse), pain score on the VAS 0–10, and pain in the same or other pain region as before the treatment. Weight and height, comorbidities (chronic heart or kidney failure), physical activity with sports, (none, up to 3 times a week, or daily exercises with or without professional support), and medication usage before and after treatment (with NSAIDs and opioids at the same, less, or greater doses) were also collected. The study was designed to determine any influence of BMI, age, gender, and co-existing diseases on the outcomes and pain relief after the RF treatment of the FJ or SIJ.
Statistical analysis
All analyses were performed using SPSS version 22 (IBM, Armonk, NY, USA). Descriptive statistics were used to summarize the number of cases, mean, standard deviation (SD), minimum, maximum, and all quartiles (ie, 25th and 75th percentile). Table 1 summarizes confidence intervals for the mean differences of VAS with standard deviation, standard error (SE), upper and lower boundaries of the interval, as well as the two-sided p value for one-sample t-tests. All statistical differences were considered significant at p<0.05. To test the normality of the data, the Kolmogorov–Smirnov (KS) test and the Shapiro–Wilk (SW) test were used. As both tests showed significant results, and therefore the assumption of normal distribution did not hold for our variables, a test on differences in location was made by the nonparametric Wilcoxon test. In many cases (if requirements of central limit theorem were fulfilled), we also conducted an additional paired t-test.
Table 1.
CIs for the mean differences of VAS
| VAS difference | Mean (SE) | 95% CI | p-Value |
|---|---|---|---|
| Pre – 1 month | 3.77 (0.20) | 3.37–4.18 | 0.000 |
| Pre – final | 3.74 (0.21) | 3.31–4.16 | 0.000 |
| 1 month – final | −0.11 (0.22) | −0.54–0.33 | 0.633 |
Abbreviations: CI, confidence interval; SE, standard error; VAS, Visual Analog Scale.
Results
Table 2 summarizes VAS for the whole sample pretreatment, 1 month post treatment, and 6 or 12 months post treatment (= final), as well as the number of cases, mean and standard deviation (SD), and the two-sided p values for tests of normality (both KS and SW tests, respectively).
Table 2.
VAS results from questionnaire sent to treated patients
| VAS
| |||
|---|---|---|---|
| Pre | 1 month | Final | |
| Cases | 160 | 157 | 159 |
| Estimators | |||
| Mean | 8.019 | 4.229 | 4.280 |
| SD | 1.41 | 2.15 | 2.47 |
| p-values (2-sided) | |||
| KS test | <0.0001 | <0.0001 | <0.0001 |
| SW test | <0.0001 | <0.0001 | <0.0001 |
Abbreviations: KS, Kolmogorov–Smirnov; SD, standard deviation; SW, Shapiro–Wilk test; VAS, Visual Analog Scale.
All treated patients were sent a questionnaire (with self-addressed return envelope) after 6 and 12 months. A total of 164 patients sent back the form; of those patients, 4 returned the form with missing data at important variables (in VAS pre and/or location), hence were removed. The remaining 160 cases composed the sample. There were no severe or moderate complications during or after the procedures. Mild complications spontaneously resolved without any sequelae.
VAS reduction total group
The results indicate a reduction of the VAS pain score in all groups 1, 6, and 12 months after treatment and a small increase between 6 and 12 months (4.209 up to 4.517). Figure 5 depicts the VAS decrease after 1 month and the long-term results after 6 and 12 months.
Figure 5.
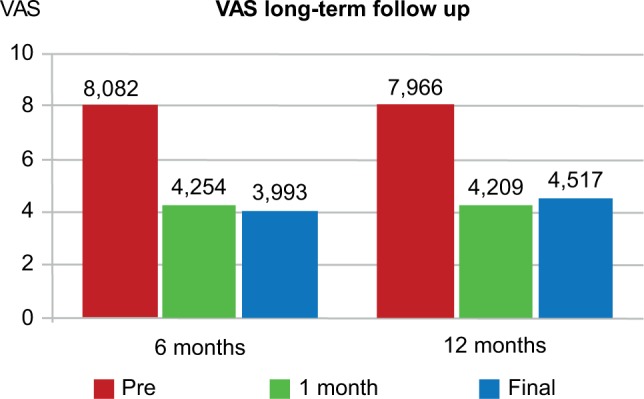
Visual Analog Scale (VAS): pre, 1 month, and final.
Medication usage (NSAIDs and opioids)
All groups of subjects required less medication for pain management in the follow-up period. For all subjects (135 valid cases), 88 of 135 (65.2%) needed less medication and just 1 of 135 (0.7%) needed more. NSAID reduction was possible for 46 of 75 cases (61%). Of the opioid users, only 14 of 37 (38%) were able to reduce or stop the medication after treatment (Figure 6).
Figure 6.
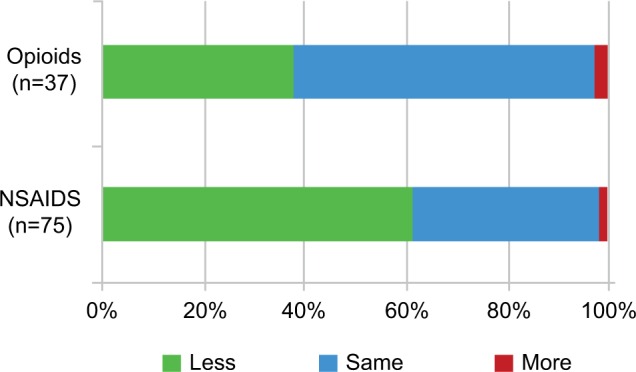
Reduction of opioids and/or nonsteroidal anti-inflammatory drugs after treatment.
Abbreviation: NSAIDS, nonsteroidal anti-inflammatory drugs.
Results sorted by area (lumbar facets and SI joint)
The results were nearly equal between subjects treated on the lumbar MBs (18G, 1-cm active tip, parallel technique) and SIJ (cooled RF treatment, Halyard Health) for VAS (Table 3) and for medication usage (NSAID and opioid; Table 4).
Table 3.
Results of MB neurotomy facetjoints and cooled RF treatment of SIJ after 6 and 12 months
| Group | VAS | n | Mean | SD | Percentiles
|
||
|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | |||||
| Lumbar | |||||||
| 6 months | Pre | 16 | 7.6 | 1.5 | 6.3 | 8.0 | 8.9 |
| 1 month | 15 | 4.5 | 1.7 | 3.0 | 4.5 | 5.0 | |
| Final | 15 | 3.3 | 2.5 | 1.0 | 3.0 | 5.0 | |
| 12 months | Pre | 27 | 7.9 | 1.2 | 7.0 | 8.0 | 9.0 |
| 1 month | 27 | 4.4 | 2.2 | 3.0 | 4.5 | 6.0 | |
| Final | 27 | 4.8 | 2.3 | 2.5 | 5.0 | 7.0 | |
| SIJ | |||||||
| 6 months | Pre | 53 | 8.2 | 1.4 | 7.0 | 8.0 | 9.3 |
| 1 month | 52 | 4.0 | 2.2 | 2.3 | 3.3 | 5.8 | |
| Final | 53 | 4.2 | 2.4 | 2.0 | 4.0 | 6.0 | |
| 12 months | Pre | 56 | 8.0 | 1.5 | 7.0 | 8.0 | 9.4 |
| 1 month | 55 | 4.1 | 2.2 | 2.5 | 3.0 | 6.0 | |
| Final | 56 | 4.4 | 2.7 | 2.0 | 4.5 | 6.0 | |
Abbreviations: MB, medial branch; SD, standard deviation; RF, radiofrequency; SIJ, sacroiliac joint; VAS, Visual Analog Scale.
Table 4.
Medication usage (NSAID and opioid)
| Area | Usage | No. of cases | Percent |
|---|---|---|---|
| Lumbar | Less | 23 | 63.9 |
| Equal | 12 | 33.3 | |
| More | 1 | 2.8 | |
| Sum | 36 | 100.0 | |
| Missing | 7 | ||
| SIJ | Less | 59 | 64.1 |
| Equal | 33 | 35.9 | |
| More | 0 | 0.0 | |
| Sum | 92 | 100.0 | |
| Missing | 17 |
Note: All groups of subjects required less medication for pain management in the follow-up period.
Abbreviations: NSAID, nonsteroidal anti-inflammatory drug; SIJ, sacroiliac joint.
BMI dependence
When the subjects were separated into two groups (BMI ≤30 or >30) as shown in Figure 7, a difference was noted in VAS and in quality of life (“do you feel better, the same, or worse since the treatment”) pre- and post treatment.
Figure 7.
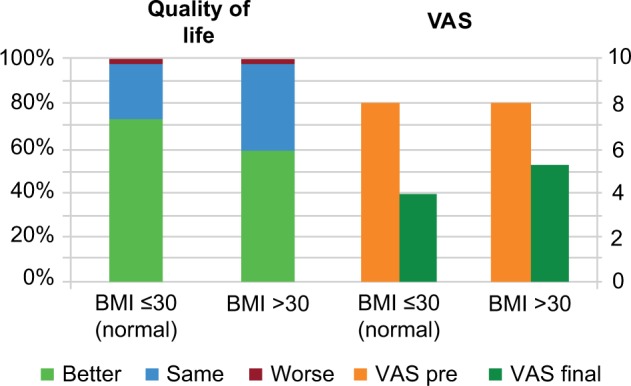
The improvement of quality of life and the VAS before and treatment in both groups.
Abbreviation: BMI, body mass index; VAS, Visual Analog Scale.
The mean VAS decrease in the normal weight group was from 8.022 to 3.978 and in the obesity group from 8.060 to 5.159 after 6 or 12 months (Table 5).
Table 5.
BMI ≤30 versus BMI >30 pain decrease after 6 and 12 months
| Group | VAS | n | Mean (SD) | Percentiles
|
||
|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||
| BMI ≤30 | ||||||
| 6 months | Pre | 48 | 8.2 (1.5) | 7.0 | 8.3 | 9.9 |
| 1 month | 47 | 4.4 (2.3) | 3.0 | 4.5 | 7.0 | |
| Final | 48 | 3.5 (2.0) | 2.0 | 3.0 | 4.9 | |
| 12 months | Pre | 68 | 7.9 (1.5) | 7.0 | 8.0 | 9.0 |
| 1 month | 68 | 4.2 (2.1) | 2.6 | 4.0 | 6.0 | |
| Final | 68 | 4.3 (2.5) | 2.0 | 4.3 | 6.9 | |
| BMI >30 | ||||||
| 6 months | Pre | 23 | 7.9 (12) | 7.0 | 8.0 | 9.0 |
| 1 month | 23 | 4.0 (1.9) | 3.0 | 3.0 | 5.0 | |
| Final | 22 | 5.1 (2.7) | 2.8 | 5.5 | 8.0 | |
| 12 months | Pre | 19 | 8.2 (1.2) | 7.0 | 8.0 | 9.0 |
| 1 month | 18 | 4.2 (2.3) | 3.0 | 3.0 | 5.3 | |
| Final | 19 | 5.2 (2.6) | 3.0 | 5.0 | 8.0 | |
Abbreviations: BMI, body mass index; SD, standard deviation; VAS, Visual Analog Scale.
Confidence interval
The 95% confidence interval of the difference of the VAS pretreatment versus 1 month post treatment was 3.37–4.18. The VAS for pretreatment versus 6 or 12 months post treatment was 3.31–4.16. This shows a 95% probability that the average pain decrease is between 3.31 and 4.16 points on the VAS scale after treatment (Table 1).
The influence of gender of the patient
In an analysis of VAS decrease by gender of the subject, our results were approximately the same for the male (n=51) and female (n=109) groups (Table 6).
Table 6.
VAS and gender dependence
| Group | VAS | n | Mean (SD) | Percentiles
|
||
|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||
| Male | ||||||
| 6 months | Pre | 19 | 7.9 (1.5) | 6.0 | 8.0 | 9.0 |
| 1 month | 19 | 3.8 (2.0) | 2.0 | 3.5 | 6.0 | |
| Final | 19 | 4.2 (2.3) | 2.0 | 4.0 | 6.0 | |
| 12 months | Pre | 32 | 8.0 (1.4) | 7.0 | 8.0 | 9.3 |
| 1 month | 32 | 3.9 (2.2) | 2.1 | 3.0 | 5.9 | |
| Final | 32 | 4.9 (2.7) | 2.1 | 5.0 | 7.0 | |
| Female | ||||||
| 6 months | Pre | 54 | 8.1 (1.4) | 7.0 | 8.0 | 9.0 |
| 1 month | 52 | 4.4 (2.2) | 3.0 | 4.0, | 6.5 | |
| Final | 53 | 3.9 (2.4) | 2.0 | 3.5 | 5.8 | |
| 12 months | Pre | 55 | 7.9 (1.5) | 7.0 | 8.0 | 9.0 |
| 1 month | 54 | 4.4 (2.1) | 3.0 | 4.5 | 6.0 | |
| Final | 55 | 4.3 (2.5) | 2.0 | 5.0 | 6.0 | |
Abbreviations: SD, standard deviation; VAS, Visual Analog Scale.
In an analysis of satisfaction (“quality of life” becoming better, equal, or worse), despite the fact that the VAS reduction in males and females was similar, the results revealed higher satisfaction with the outcome in the female group (Figure 8).
Figure 8.
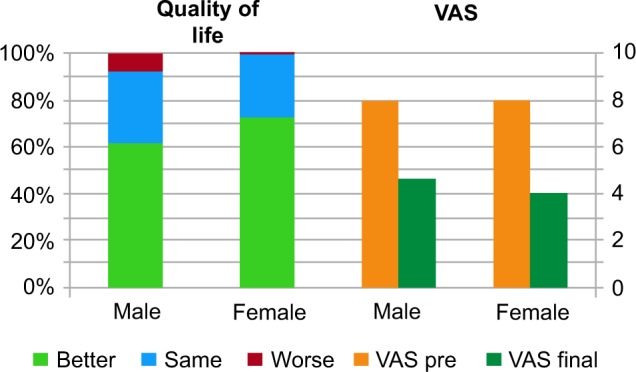
Nearly equal decrease in the VAS score, which is not concordant with the feeling of quality of life in male versus female.
Abbreviation: VAS, Visual Analog Scale.
In an analysis of the “no sports” group versus the active group (doing sports activities 1–3 times a week), the data showed a larger decrease (Table 7) in pain after 1 year in the active group (Figure 9) and changes in quality of life (Figure 10).
Table 7.
Difference in VAS between physically active (sports group) and sedentary (no sports) group
| Group | VAS | n | Mean (SD) | Percentiles
|
||
|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||
| No sports | ||||||
| 6 months | Pre | 21 | 8.1 (1.3) | 7.0 | 8.0 | 9.0 |
| 1 month | 21 | 4.5 (2.1) | 3.0 | 4.5 | 5.0 | |
| Final | 20 | 4.5 (2.6) | 3.0 | 4.3 | 6.4 | |
| 12 months | Pre | 20 | 8.4 (1.1) | 7.5 | 8.5 | 9.0 |
| 1 month | 19 | 4.8 (2.5) | 3.0 | 5.0 | 7.0 | |
| Final | 20 | 5.5 (2.7) | 3.0 | 6.0 | 8.0 | |
| At least once/week | ||||||
| 6 months | Pre | 45 | 8.1 (1.5) | 7.3 | 8.0 | 9.0 |
| 1 month | 44 | 3.8 (2.1) | 2.3 | 3.0 | 5.0 | |
| Final | 45 | 3.9 (2.2) | 2.0 | 3.5 | 6.0 | |
| 12 months | Pre | 60 | 7.9 (1.5) | 7.0 | 8.0 | 9.0 |
| 1 month | 60 | 4.0 (2.1) | 2.5 | 3.0 | 5.4 | |
| Final | 60 | 4.2 (2.4) | 2.0 | 4.3 | 6.0 | |
Abbreviations: SD, standard deviation; VAS, Visual Analog Scale.
Figure 9.
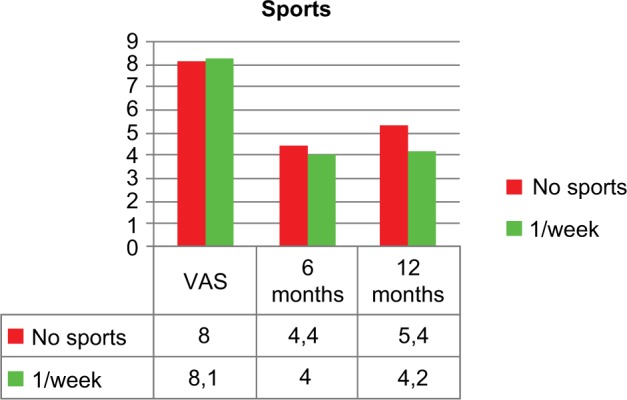
Better long-term pain decrease in the sports group, VAS pre-, 1 month, and 6–12 months.
Abbreviation: VAS, Visual Analog Scale.
Figure 10.
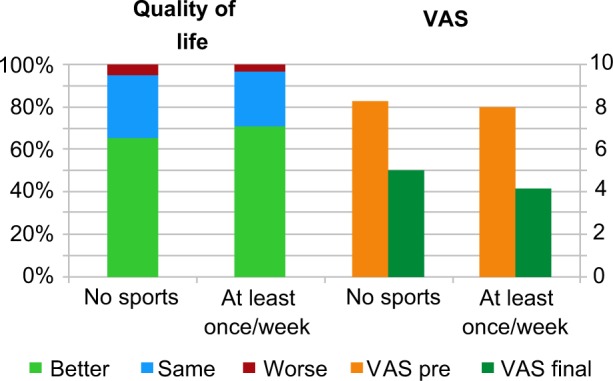
Improvement of quality of life in no sports and sports group after treatment (left) and final VAS course after 12 months (right).
Abbreviation: VAS, Visual Analog Scale.
Table 7 shows the VAS reduction for the two groups (no sports activity versus physical activity at least once a week). The VAS increased to 5.5 after 12 months in the sedentary group, whereas pain levels were almost equal after 6 and 12 months (VAS: 3.9 after 6 months to 4.2 after 1 year) in those who did sports activity at least once a week.
Similar to these results, as it is shown in Figure 10, the satisfaction and the VAS reduction after 12 months of those who do sports at least once a week were higher than that of the no sports activity group.
Conclusions and discussion
The durability of pain relief reported in this study is consistent with other studies of RF neurotomy for SIJ-mediated LBP and lumbar FJ-mediated LBP.15,17–19
The limitations of this study are those that apply to all retrospective investigations: there was no control group to account for confounders, such as the placebo effect. However, the differences that were seen were larger than what we would expect for the placebo effect. There were also issues with difficulties that occurred with a small percentage of subjects in filling out the questionnaire and returning it to the investigative staff, and missing data for some of these subjects.
A single intra-articular (SIJ) or MB (lumbar FJ) diagnostic block was used in selecting subjects to undergo RF or cooled RF LBN. Despite the recommendation of the SIS to perform double blocks, the authors prefer the use of a single block in their practices.
The main reason for this is that most of the patients, having obtained impressive pain relief after the first block, did not understand that this was a transient effect and that a second block would be necessary for severe degenerative changes. The authors have noted that doing a second block after a positive first block can engender insecure feelings and lead to reduced compliance. There is a substantial risk of false-positive responses to local anesthetic blocks, and the likely inclusion of subjects with false-positive responses in this study is a limitation that may contribute to the relatively lower success rates compared with studies in which controlled blocks were used.
The decreases in chronic pain and medication usage in this study suggest that the use of RF treatment should be first-line treatment for LBP, with a 95% probability of significant pain reduction (3–4 points on the VAS 0–10 scale) that may last for 12 months.
The data suggest a lower decrease of pain, and improvement of quality of life may be achieved in patients with BMI >30. However, the changes are still statistically and clinically significant. These results may be explained by technical difficulties in performing the procedure in larger patients or a higher C-reactive protein value and underlying inflammation in some obese patients. This bears further investigation. However, the presence of obesity should not be construed as a contraindication to interventions, such as neurotomies of the lumbar MB, L5 DR, or LB of SIJ. Obesity may prove to be a significant predictive factor.
The discrepancy in the response of the female and male subjects in this study was interesting, in that the Austrian women seem to be more satisfied than the men with the same decrease of VAS. However, further gender-specific studies should be done to confirm this observation about the outcome of these treatments. An interesting point could be that endocrine or menopausal status and perhaps former pregnancies may have played a role in our study as many more women (108) than men (51) reported chronic LBP.
The better long-term pain relief reported by the group doing sports activities 1–3 times a week for at least 30 minutes suggests that LBP patients may get benefit from engaging in regular exercise. Further studies will be needed to determine whether special sports programs could be designed to further improve these outcomes.
The results of the lumbar MB neurotomies with the parallel needle technique seem to be as good as the results of LB neurotomies of the SIJ with the cooled RF probe (Halyard Health SInergy System). Overall, the authors have determined that treatment with RF methods for chronic LBP is a safe and effective method for long-term pain reduction. It is recommended that insurance coverage should be provided for this treatment.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine (Phila Pa 1976) 2000;25(10):1270–1277. doi: 10.1097/00007632-200005150-00012. [DOI] [PubMed] [Google Scholar]
- 2.MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2013;14(5):639–645. doi: 10.1111/pme.12000. [DOI] [PubMed] [Google Scholar]
- 3.Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976) 1996;21(16):1889–1892. doi: 10.1097/00007632-199608150-00012. [DOI] [PubMed] [Google Scholar]
- 4.Gallagher J, Petriccione de Vadi PL, Wedley JR. RF facet joint denervation in treatment of LBP: Prospective controlled double blind study. Pain Clinic. 1994;7:193–198. [Google Scholar]
- 5.Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine (Phila Pa 1976) 2001;26(13):1411–1416. doi: 10.1097/00007632-200107010-00003. [DOI] [PubMed] [Google Scholar]
- 6.Van Wijk RM, Geurts JW, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain. A randomized, double-blind sham lesion-controlled trial. Clin J Pain. 2004;21(4):335–344. doi: 10.1097/01.ajp.0000120792.69705.c9. [DOI] [PubMed] [Google Scholar]
- 7.Bogduk N, Dreyfuss P, Govind J. A narrative review of lumbar medial branch neurotomy for the treatment of back pain. Pain Med. 2009;10(6):1035–1045. doi: 10.1111/j.1526-4637.2009.00692.x. [DOI] [PubMed] [Google Scholar]
- 8.Van Zundert J, Vanelderen P, Kessels A, van Kleef M. Radiofrequency treatment of facet-related pain: evidence and controversies. Curr Pain Headache Rep. 2012;16(1):19–25. doi: 10.1007/s11916-011-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stelzer W, Aiglesberger M, Stelzer D, Stelzer V. Use of cooled radiofrequency lateral branch neurotomy for the treatment of sacroiliac joint-mediated low back pain: a large case series. Pain Med. 2013;14(1):29–35. doi: 10.1111/pme.12014. [DOI] [PubMed] [Google Scholar]
- 10.Manchikanti L, Abdi S, Atluri S, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013;16(Suppl 2):S49–283. [PubMed] [Google Scholar]
- 11.Patel N, Gross A, Brown L, Gekht G. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain. Pain Medicine. 2012;13(3):383–398. doi: 10.1111/j.1526-4637.2012.01328.x. [DOI] [PubMed] [Google Scholar]
- 12.Cohen SP, Hurley RW, Buckenmaier CC, 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109(2):279–288. doi: 10.1097/ALN.0b013e31817f4c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen SP, Huang JHY, Brummett C. Review Facet joint pain–advances in patient selection and treatment. Nat Rev Rheumatol. 2013;9(2):101–116. doi: 10.1038/nrrheum.2012.198. [DOI] [PubMed] [Google Scholar]
- 14.Cohen SP, Strassels SA, Kurihara C, Crooks MT, Erdek MA, Forsythe A, Marcuson M. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg AnesPain Med. 2009;3(34):206–214. doi: 10.1097/AAP.0b013e3181958f4b. [DOI] [PubMed] [Google Scholar]
- 15.Cohen SP, Hurley RW, Christo PJ, Winkley J, Mohiuddin MM, Stojanovic MP. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007;231(1):45–52. doi: 10.1097/01.ajp.0000210941.04182.ea. [DOI] [PubMed] [Google Scholar]
- 16.Streitberger K, Müller T, Eichenberger U, Trelle S, Curatolo M. Factors determining the success of radiofrequency denervation in lumbar facet joint pain: a prospective study. Eur Spine J. 2011;20(12):2160–2165. doi: 10.1007/s00586-011-1891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel N, Gross A, Brown L, Gekht G. A randomized, placebo controlled study to assess the efficacy of lateral branch denervation for chronic sacroiliac joint pain. Pain Med. 2012;13(3):383–98. doi: 10.1111/j.1526-4637.2012.01328.x. [DOI] [PubMed] [Google Scholar]
- 18.Hagg O, Fritzell P, Nordwall A, Swedish Lumbar Spine Study Group The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 19.Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine (Phila Pa 1976) 2004;29(21):2471–2473. doi: 10.1097/01.brs.0000143170.47345.44. [DOI] [PubMed] [Google Scholar]