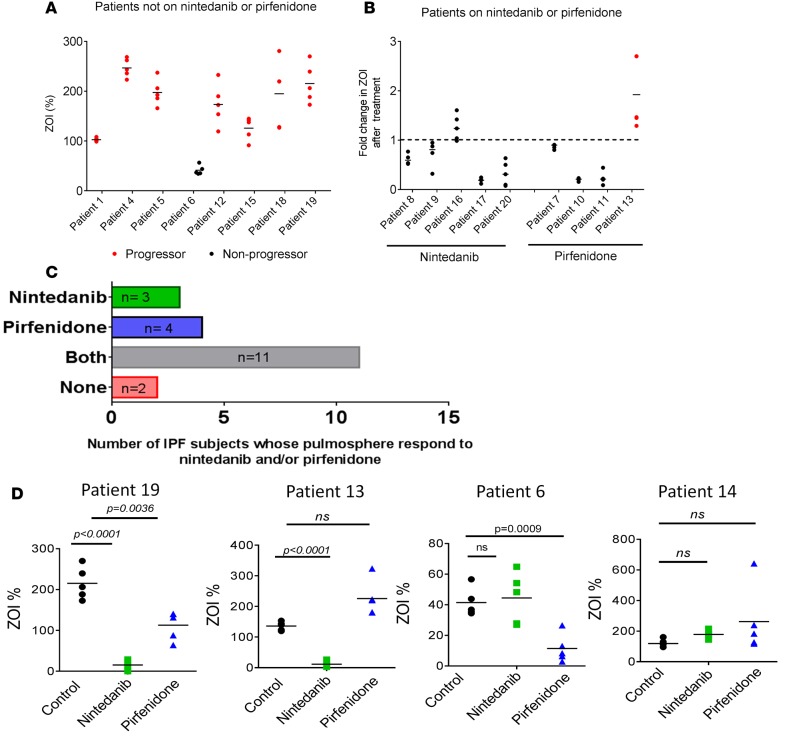
Figure 6. Correlation between pulmosphere invasiveness and disease progression in patients with IPF.
(A) Relationship between clinical outcomes in individual patients and invasiveness of patient pulmosphere. These 8 patients with IPF were not on any medication directed to IPF. Progressors were defined as those patients with a drop in forced vital capacity (FVC) >10% or a drop in DLCO >15% in 12 months or death. (B) Relationship between patient disease progression and pulmosphere invasiveness in response to nintedanib and pirfenidone. Five patients were on nintedanib, and four patients were on pirfenidone (red represents progressors and black represents nonprogressors. Median values of ZOI >1 represent pulmospheres nonresponsive to the treatment, and median values of ZOI <1 represent pulmospheres responsive to drug treatment. (C) Number of patients whose pulmospheres were responsive to nintedanib only (green), pirfenidone only (blue), either nintedanib or pirfenidone (gray), or neither (red). (D) Individual patient responses to nintedanib and pirfenidone. Patient 19 responded to both nintedanib and pirfenidone, with greater inhibition of invasiveness of pulmospheres with nintedanib than pirfenidone. Patient 13 responded only to nintedanib. Patient 6 responded only to pirfenidone. Patient 14 did not respond to nintedanib or pirfenidone. All P values, compared with untreated pulmospheres, 2-tailed paired t test. Data were obtained from 5 pulmosphere for each group (untreated, nintedanib treated, and pirfenidone treated) per patient. “Response” is defined as a decrease in the ZOI% of each patient’s pulmosphere after treatment with nintedanib or pirfenidone as compared with untreated control.