Abstract
Background: In a cadaveric model, we evaluated thumb metacarpal subsidence, indicated by a decreased metacarpal-to-scaphoid distance, after 2 surgical procedures used to treat thumb carpometacarpal (CMC) osteoarthritis (OA): partial trapeziectomy with capsular interposition (PTCI), which involves removal of 2 mm of both the distal trapezium and base of the metacarpal; and total trapeziectomy with capsular interposition (TTCI). Methods: Nine matched pairs of cadaveric hands were randomly assigned to undergo either PTCI or TTCI. Preoperatively, physiologic forces were applied across the thumb CMC joint by loading 6 tendons, simulating lateral pinch. Anteroposterior radiographs were obtained, and the metacarpal-to-scaphoid distance on each image was estimated independently by 3 separate readers using customized software. A hand surgeon then performed the PTCI and TTCI procedures, and the measurements under loading were repeated. The results were assessed for interrater reliability. Mean values for metacarpal-to-scaphoid distance before and after the surgical procedures were compared. Results: Preoperatively, the metacarpal-to-scaphoid distance in the PTCI and TTCI groups was not significantly different. Postoperatively, metacarpal subsidence was significantly less in the PTCI group (17% compared with 34% for TTCI; P = .05). Conclusions: Metacarpal subsidence occurred after both PTCI and TTCI, but significantly less subsidence was observed after PTCI; thus, thumb length was better preserved. Previous research has shown an inverse correlation between maintenance of thumb length and overall Disabilities of the Arm, Shoulder, and Hand (DASH) score. A procedure for treating thumb CMC OA that preserves thumb length and minimizes disruption of stabilizing joint tissue may provide enhanced maintenance of thumb stability and improved patient outcomes.
Keywords: arthroplasty, carpometacarpal, joint, osteoarthritis, thumb, trapezium
Introduction
Osteoarthritis (OA) affects the joints of the hand of more than 2.9 million US adults who are older than 60 years of age.7,19 OA of the thumb carpometacarpal (CMC) joint most commonly occurs in postmenopausal women, affecting more than one-third of those older than 65 years.1,27 Symptoms of thumb CMC OA include pain at the base of the thumb, swelling and stiffness of the joint, and decreased grip and pinch strength. The symptoms can be sufficiently severe that patients cannot perform vocational activities or activities of daily living and their quality of life may decline markedly.
Surgical treatments for thumb CMC OA include first metacarpal osteotomy, trapezial osteotomy, arthrodesis, trapeziectomy, ligament reconstruction and tendon interposition (LRTI), hematoma distraction arthroplasty, bone or soft tissue interposition arthroplasty, and joint-replacement arthroplasty.4,5,8-11,13,15,21,22,24-26 All these techniques have been found to mitigate symptoms and improve function, but an “ideal” procedure that not only alleviates pain but also preserves the length, stability, strength, and normal function of the thumb, while avoiding the morbidity associated with tendon harvest, has not yet been established.
Partial trapeziectomy with capsular interposition (PTCI) was recently described as a novel treatment for thumb CMC OA.18 Development of this procedure stemmed from studies by Barron and Eaton2 and Mo and Gelberman.17 In the former, the authors introduced trapezial arthrotomy with minimal bony resection and tendon interposition; in the latter, this technique was modified to add minimal bony resection of the base of the metacarpal. Both studies encouraged salvage of the trapezium for decreasing the risk of shortening and subluxation of the thumb, which results from total trapeziectomy procedures. The PTCI procedure involves removal of the irregular arthritic surface of the metacarpal base, resection of only the distal aspect of the trapezium, and use of the joint capsule to provide local tissue interposition. By minimizing hard and soft tissue disruption, this technique is theorized to maintain thumb stability as indicated by maintenance of ligamentous tethers and thumb length. We report a biomechanical, cadaveric study of this technique in which it was compared with total trapeziectomy with capsular interposition (TTCI). Specifically, we compared thumb metacarpal subsidence after each operation. We hypothesized that, compared with TTCI, PTCI results in less disruption of bone and soft tissue and therefore will experience less metacarpal subsidence under load.
Materials and Methods
Nine matched pairs of fresh-frozen cadaveric hands (5 men and 4 women; mean age = 38.5 years [range = 20-54 years]) were used for this study. Each pair was randomly assigned to the TTCI or PTCI group by using random-number-generation software. All thumb CMC joints were examined fluoroscopically before the study to ensure that they were free of degenerative changes.
An aluminum jig was fabricated to stabilize the hand with the thumb in the lateral pinch position. With the use of a braided-suture locking stitch, the flexor pollicis longus (FPL), adductor pollicis (ADD), opponens pollicis (OPP)/flexor pollicis brevis (FPB), abductor pollicis longus (APL), and abductor pollicis brevis (APB) tendons were dissected, tagged, and fixed with acrylic thread for physiologic loading. We loaded these 6 tendons in line with the direction of pull of the muscle fibers.6 The FPL and APL were each loaded with 2.5 kg, the ADD/OPP/FPB with 3 kg, and the APB with 1.5 kg (Figure 1). To provide a reference for relative metacarpal motion and metacarpal-to-scaphoid distance, 2 K-wires were embedded in the bone of the first metacarpal base (immediately distal of the resection site) and the distal scaphoid. The K-wires were placed so that they were free of soft tissue tethers.
Figure 1.
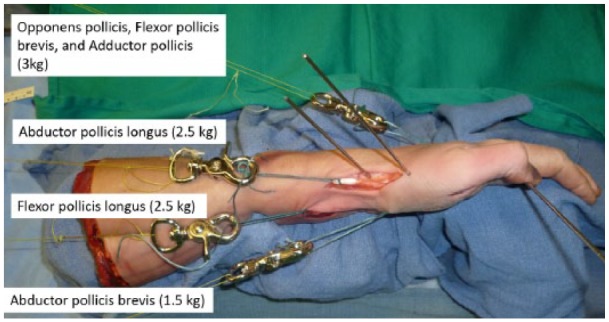
Cadaveric hand specimen placed in custom-built fixture to restrain it during anatomical loading of tendons to simulate lateral pinch.
Note. Weighted suture was attached to the flexor pollicis longus, adductor pollicis, opponens pollicis/flexor pollicis brevis, abductor pollicis longus, and abductor pollicis brevis tendons.
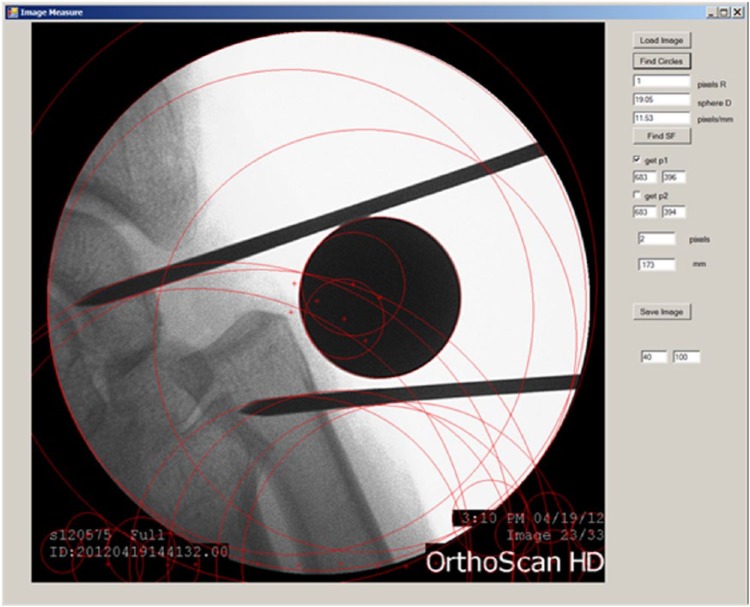
Three different readers then estimated the metacarpal-to-scaphoid distance in all wrists by examining 3 anteroposterior radiographs for each specimen. To prevent any differences in magnification between images from affecting the accuracy of measurements, a 19.1-mm-diameter metal sphere was used as a calibration marker. Custom-designed software using the Hough transform model23 was developed to calibrate the linear distance between the ends of the K-wires and the known diameter of the sphere (Figure 2). This software computes the ratio of the measured diameter of the sphere to the number of pixels along the diameter of the sphere in the radiograph. This information is then used to calculate the distance between K-wires, which is equal to the metacarpal-to-scaphoid distance under applied load.
Figure 2.
Custom software showing implementation of the Hough transform model for the identification of the spherical marker in the field of view.
Note. The software computes the ratio of the known diameter of the sphere to the number of pixels along the diameter of the sphere in the radiograph. It then uses this information to calculate the distance between K-wire tips to estimate metacarpal-to-scaphoid distance. The red circles indicate areas identified by the software as regions forming an arc. The sphere is isolated from these circles.
The randomly assigned surgical procedure (PTCI or TTCI) was then performed by a fellowship-trained hand surgeon. The TTCI technique was based on the operation described by Gervis in 194912 but was modified to include capsular interposition tissue. The principal steps in the PTCI procedure are exposure of the thumb CMC joint by elevating the periosteum and APL tendon from the base of the first metacarpal, resection of 2 mm of bone from both the base of the first metacarpal and the distal aspect of the trapezium, use of redundant local capsular tissue for interposition, and repair of the joint by reefing the periosteal flap and APL tendon on the dorsal surface of the first metacarpal.18 After the surgical procedures, tendons were loaded and unloaded with thumb distraction to encourage settling of bones and soft tissue. Following the fifth load/unload cycle, measurements and estimations of metacarpal-to-scaphoid distance were performed according to the same protocol as that used preoperatively.
Statistical Analysis
Before the study, we conducted a power analysis that assumed, on the basis of a previous radiographic analysis of thumb CMC OA progression,16 that 2 mm would represent a clinically important difference in metacarpal-to-scaphoid distance. We calculated that a sample size of 9 matched pairs was adequate to detect a 2-mm difference between the 2 surgical groups with α = 0.05 and β = 0.20.
All measurements were done independently by 3 readers who were blinded to the measurements obtained by the other 2 readers. The data were assessed for systematic bias across readers and specimens by using 3-way analysis of variance (ANOVA) and assuming that P ≤ .05 represented a significant difference. If no bias was observed, we planned to average the values for metacarpal-to-scaphoid distance across readers and specimens and use Student t tests to compare values for specimens in the TTCI group with those in the PTCI group. If bias was observed, we planned to calculate the mean value for each reader and then compare the 3 means by using 3-way ANOVA.
Results
We observed no main effect or interaction among readers (P = .98) or specimens (P = .90) and no significant differences among the values for metacarpal-to-scaphoid distance estimated by each reader (P > .88). Because the measurements were consistent, we averaged all values across readers and specimens.
Preoperatively, there was no significant difference in the metacarpal-to-scaphoid distance under applied load between the TTCI and PTCI groups (23.13 mm [SD = 3.40] vs. 25.61 mm [SD = 3.31]; P = .23). Postoperatively, the distance under applied load was smaller in the TTCI group compared with the PTCI group (15.38 mm [SD = 2.48] vs. 21.30 [SD = 2.72]; Figure 3). Overall, the postoperative reduction in metacarpal-to-scaphoid distance was significantly larger in the TTCI group (7.75 mm [SD = 3.09] vs. 4.28 mm [SD = 3.25]; 34% vs. 17%; P < .001), indicating that metacarpal subsidence was greater. Figure 4 shows representative images of post-TTCI and post-PTCI specimens. In the post-TTCI specimen (Figure 4), the thumb metacarpal subsided to a point near the scaphoid as a result of excision of the trapezium. In the post-PTCI specimen (Figure 4), the remainder of the trapezium was interposed between the metacarpal and scaphoid, so thumb metacarpal subsidence was minimal.
Figure 3.
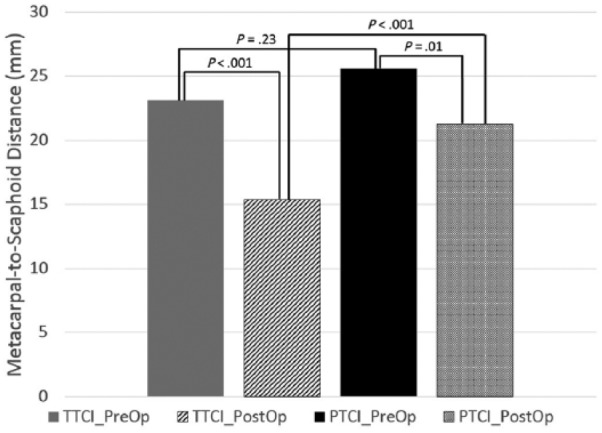
Mean metacarpal-to-scaphoid distance for TTCI and PTCI specimens under applied load.
Note. There was no significant difference between the 2 groups preoperatively. However, there was a significant difference between the 2 groups in metacarpal-to-scaphoid distance postoperatively, with the TTCI group showing greater metacarpal subsidence. TTCI, total trapeziectomy with capsular interposition; PTCI, partial trapeziectomy with capsular interposition.
Figure 4.
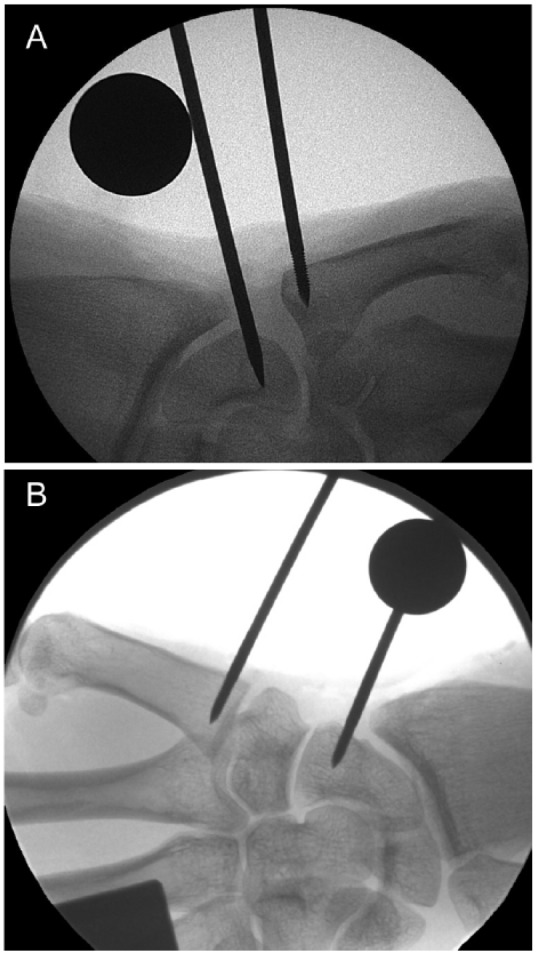
Representative images obtained after TTCI and PTCI in a cadaveric model simulating lateral pinch.
Note. (A) In the post-TTCI specimen, the thumb metacarpal has subsided to a point near the scaphoid as a result of excision of the trapezium. (B) With PTCI, only the diseased articular surfaces of the metacarpal and trapezium are removed, leaving the remainder of the trapezium interposed between the metacarpal and scaphoid; therefore, thumb metacarpal subsidence is minimal. TTCI, total trapeziectomy with capsular interposition; PTCI, partial trapeziectomy with capsular interposition.
Discussion
In a cadaveric model, PTCI resulted in significantly less metacarpal subsidence under simulated lateral pinch than did TTCI. Maintenance of thumb length has been reported to inversely correlate with overall Disabilities of the Arm, Shoulder, and Hand (DASH) scores and specific DASH questions involving high-strength activities.25 It is possible that PTCI may result in improved patient outcomes as measured by DASH because of postoperative thumb length maintenance, but a clinical study of PTCI with 2-year minimum follow-up would be required to support this argument. To date, no studies investigating surgical treatment for thumb CMC OA have found a direct correlation between thumb shortening and reduced grip strength or pinch strength. However, a self-perceived improvement in symptoms when performing high strength pinch or grip activities as measured by the DASH may be indicative of an improvement of the upper extremity as an overall functional unit.14
Our results with respect to subsidence of the thumb metacarpal after total excision of the trapezium are similar to those in the cadaver study by Yao et al,28 who measured the distance from the metacarpal base to the distal surface of the trapezium before and after total trapeziectomy and suspension of the metacarpal with either a K-wire or suture-button device. The mean loss in space height was 12.8 mm in the K-wire group (n = 10) and 13.2 mm in the suture-button group (n = 10). We found a loss of 7.75 mm after TTCI including capsular interposition. It is important to note that Yao et al did not use interposition material. Our findings are also comparable with those of a cadaveric study comparing the trapezial space height of 3 common treatments for thumb CMC OA: trapezial excision alone, trapezial excision and suture suspensionplasty (TESS), and trapezial excision followed by LRTI.20 This group reported a statistically significant loss in height for all procedures, with the TESS procedure resulting in the least loss in trapezial space height (3 mm). We found a difference of 4.28 mm after the PTCI procedure.
The limitations of our study include the possibility that variations in the quality of the cadaveric tissue influenced our results. However, we think that our use of a matched-pairs study design reduced effects commonly attributed to variations in tissue quality, joint incongruity, and morphologic characteristics. In addition, randomization controlled for inherent differences in strength and stability between the hands in any given pair. Another possible limitation was that cadaveric specimens do not undergo the biologic healing that could change thumb CMC joint dynamics and subsidence results. Clinical studies have shown that initial postoperative measures of subsidence are less than those taken at a minimum 2-year follow-up.4,25 It is possible that long-term follow-up of PTCI in patients may show increased subsidence. Therefore, our results would most closely compare with immediate postoperative clinical findings of thumb subsidence. A clinical study on PTCI may also help reveal the long-term effects of bony impingement on the redundant tissue between the rough surfaces of the metacarpal and trapezium. Furthermore, we used cadaveric specimens from younger persons (mean age at death = 38.5 years) to limit the possibility that age-related conditions affected the biomechanical results. Our study was focused on baseline measurements of metacarpal-to-scaphoid distance in matched pairs, and we therefore wanted to avoid the possibility that adjacent joint arthritis or compromise of ligaments associated with thumb CMC OA would affect these measurements. Finally, it is important to note that removal of the entire trapezium in the TTCI technique would require removal of local ligamentous tissue attachments on the trapezium. Interposition was achieved by suturing the ligamentous attachments that remain on the metacarpal base to the deep capsular tissue, subsequently adding a level of stability and limiting subsidence. Yet, the TTCI procedure would be less stable and thereby represents a worst-case-scenario comparison to the PTCI technique.
In conclusion, in a cadaveric model under lateral pinch load, PTCI resulted in less proximal metacarpal subsidence and better maintenance of thumb length than TTCI. In addition, PTCI, unlike TTCI, retains all soft tissue tethers. In fact, the technique of reefing the periosteal flaps corrects for existing joint subluxation, thus enhancing stabilization of the joint. Moreover, PTCI does not require implants such as Artelon spacers, which have been shown to cause more pain and less satisfaction in patients compared with trapeziectomy using LRTI.3 Avoiding implants and allograft interposition material may minimize the technical demand of the surgical procedure and possibly improve success of the treatment. Finally, PTCI does not require tendon harvest, so harvest-site morbidity is avoided. We submit that the PTCI technique merits further investigation to determine whether its clinical outcomes are comparable with or superior to those of commonly used surgical procedures to treat thumb CMC OA.
Acknowledgments
The authors thank Zainab Cheema for assistance with experimental testing, Clifford Qualls for assistance with statistical analysis, and Renée Robillard and Sahar Freedman for editorial assistance.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This is purely a cadaveric study with no human subjects included; therefore, informed consent is not applicable.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19(3):340-341. [DOI] [PubMed] [Google Scholar]
- 2. Barron OA, Eaton RG. Save the trapezium: double interposition arthroplasty for the treatment of stage IV disease of the basal joint. J Hand Surg Am. 1998;2:196-204. [DOI] [PubMed] [Google Scholar]
- 3. Blount AL, Armstrong SD, Yuan F, Burgess SD. Porous polyurethaneurea (Artelon) joint spacer compared to trapezium resection and ligament reconstruction. J Hand Surg Am. 2013;38(9):1741-1745. [DOI] [PubMed] [Google Scholar]
- 4. Burton RI, Pellegrini VD., Jr Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11(3):324-332. [DOI] [PubMed] [Google Scholar]
- 5. Cheema T, Salas C, Morrell N, Lansing L, Reda Taha MM, Mercer D. Opening wedge trapezial osteotomy as possible treatment for early trapeziometacarpal osteoarthritis: a biomechanical investigation of radial subluxation, contact area, and contact pressure. J Hand Surg Am. 2012;37(4):699-705. [DOI] [PubMed] [Google Scholar]
- 6. Cooney WP, III, Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 1977;59(1):27-36. [PubMed] [Google Scholar]
- 7. Dillon CF, Hirsch R, Rasch EK, Gu Q. Symptomatic hand osteoarthritis in the United States: prevalence and functional impairment estimates from the third U.S. National Health and Nutrition Examination Survey, 1991-1994. Am J Phys Med Rehabil. 2007;86(1):12-21. [DOI] [PubMed] [Google Scholar]
- 8. Earp BE, Leung AC, Blazar PE, Simmons BP. Arthroscopic hemitrapeziectomy with tendon interposition for arthritis at the first carpometacarpal joint. Tech Hand Up Extrem Surg. 2008;12(1):38-42. [DOI] [PubMed] [Google Scholar]
- 9. Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55(8):1655-1666. [PubMed] [Google Scholar]
- 10. Edwards SG, Ramsey PN. Prospective outcomes of stage III thumb carpometacarpal arthritis treated with arthroscopic hemitrapeziectomy and thermal capsular modification without interposition. J Hand Surg Am. 2010;35(4):566-571. [DOI] [PubMed] [Google Scholar]
- 11. Fulton DB, Stern PJ. Trapeziometacarpal arthrodesis in primary osteoarthritis: a minimum two-year follow-up study. J Hand Surg Am. 2001;26(1):109-114. [DOI] [PubMed] [Google Scholar]
- 12. Gervis WH. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint. J Bone Joint Surg Br. 1949;31B(4):537-539. [PubMed] [Google Scholar]
- 13. Gray KV, Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am. 2007;32(1):23-29. [DOI] [PubMed] [Google Scholar]
- 14. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hobby JL, Lyall HA, Meggitt BF. First metacarpal osteotomy for trapeziometacarpal osteoarthritis. J Bone Joint Surg Br. 1998;80(3):508-512. [DOI] [PubMed] [Google Scholar]
- 16. Koff MF, Ugwonali OF, Strauch RJ, Rosenwasser MP, Ateshian GA, Mow VC. Sequential wear patterns of the articular cartilage of the thumb carpometacarpal joint in osteoarthritis. J Hand Surg. 2003;28(4):597-604. [DOI] [PubMed] [Google Scholar]
- 17. Mo JH, Gelberman RH. Ligament reconstruction with trapezium retention arthroplasty for carpometacarpal arthritis. J Hand Surg Am. 2004;29A:240-246. [DOI] [PubMed] [Google Scholar]
- 18. Moneim MS, Morrell NT, Mercer DM. Partial trapeziectomy with capsular interposition arthroplasty (PTCI): a novel technique for thumb basal joint arthritis. Tech Hand Surg. 2014;18(3):116-120. [DOI] [PubMed] [Google Scholar]
- 19. Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38(8):1134-1141. [DOI] [PubMed] [Google Scholar]
- 20. Putnam MD, Rattay R, Wentorf F. Biomechanical test of three methods to treat thumb CMC arthritis. J Wrist Surg. 2014;3(2):107-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rai JK, Singh P, Mendonca D, Porter M. Trapeziectomy with a capsular interposition flap. Ann R Coll Surg Engl. 2009;91(4):345-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shapiro PS, Diao E, Givens LM. Meniscal allograft arthroplasty for the treatment of trapeziometacarpal arthritis of the thumb. Hand. 2015;10:407-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smereka M, Duleba I. Circular object detection using a modified Hough transform. Int J Appl Math Comput Sci. 2008;18(1):85-91. [Google Scholar]
- 24. Swanson AB. Disabling arthritis at the base of the thumb: treatment by resection of the trapezium and flexible (silicone) implant arthroplasty. J Bone Joint Surg Am. 1972;54(3):456-471. [PubMed] [Google Scholar]
- 25. Trumble T, Rafijah G, Heaton D. Thumb carpometacarpal arthroplasty with ligament reconstruction and interposition costochondral arthroplasty. J Wrist Surg. 2013;2(3):220-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Varley GW, Calvey J, Hunter JB, et al. Excision of the trapezium for osteoarthritis at the base of the thumb. J Bone Joint Surg Br. 1994;76(6):964-968. [PubMed] [Google Scholar]
- 27. Xu L, Strauch RJ, Ateshian GA, Pawluk RJ, Mow VC, Rosenwasser MP. Topography of the osteoarthritic thumb carpometacarpal joint and its variations with regard to gender, age, site, and osteoarthritic stage. J Hand Surg Am. 1998;23(3):454-464. [DOI] [PubMed] [Google Scholar]
- 28. Yao J, Zlotolow DA, Murdock R, Christian M. Suture button compared with K-wire fixation for maintenance of posttrapeziectomy space height in a cadaver model of lateral pinch. J Hand Surg Am. 2010;35(12):2061-2065. [DOI] [PubMed] [Google Scholar]