Abstract
Gossypiboma (retained surgical sponge) occurs between 1 in 1000 and 1 in 1500 of all intra-abdominal operations. Patients with gossypibomas may present asymptomatically or with nonspecific symptoms, such as abdominal pain or bloating; identification frequently relies on imaging. Results of imaging alone, however, may appear nonspecific, and the gossypiboma may mimic other masses, such as neoplasms, hematomas, or abscesses. They require surgical removal for definitive diagnosis and treatment. Herein we present an unusual case of gossypiboma masquerading as an urachal mass in a 75-year-old woman. Diagnostic evaluation, natural history, and prevention of retained surgical materials are discussed.
Keywords: Gossypiboma, Urachal mass, Surgical errors, Patient safety
Gossypiboma (also known as textiloma or cottonoid) refers to a mass arising from a cottonoid matrix, most commonly a retained surgical sponge, surrounded by an inflammatory reaction.1 The term derives from Latin gossypium (cotton) and Kiswahili boma (place of concealment, or hiding). Though they most frequently occur in the abdominal or pelvic cavity, with a reported (and likely underestimated) incidence between 1 in 1000 and 1 in 1500 intra-abdominal operations, they may occur at any operative site.2 Diagnosis is not always straightforward,3 as some patients may be asymptomatic or present with nonspecific symptoms. Surgical removal is mandatory as life-threatening complications can result from untreated gossypiboma. Furthermore, although imaging studies often identify abnormalities at the site of gossypiboma, the differential diagnosis may entail alternative entities, such as a neoplasm, hematoma, or abscess. Here, we report an unusual case of gossypiboma mimicking an urachal mass following a remote open abdominal hysterectomy. We describe the clinical course and discuss diagnostic evaluation, natural history, and prevention of retained surgical materials.
Case Report
A 75-year-old Hispanic woman presented with a 2-week history of lower abdominal pain and fullness. She was afebrile and vital signs were normal. A 5-cm subcutaneous mass was palpable on examination, underlying a lower midline scar from an abdominal hysterectomy that she had undergone previously in Mexico. Results of preoperative laboratory investigations, including complete blood count, basic metabolic panel, and liver function tests, were normal. Computed tomography (CT) scan demonstrated a 5-cm cystic mass anterior to the rectus muscle (Figure 1A) which was in continuity with a larger (10.4 × 9.3 cm) intra-abdominal cystic mass (Figure 1B and Figure 1C). The abdominal mass had a 3.7 × 2.8cm solid component posteriorly (Figure 1B), and abutted the dome of the urinary bladder inferiorly. The imaging findings were concerning for urachal tumor. Preoperative biopsy of the superficial component of the mass revealed abundant histiocytes and multinucleate giant cells with no evidence of malignancy. The patient underwent laparotomy and surgical excision of the urachal mass with a cuff of adherent dome of bladder. Postoperative recovery was uneventful. Gross pathologic examination revealed a retained surgical gauze within the mass, presumably from her prior gynecologic surgery (Figure 2). Microscopic evaluation revealed exuberant histiocytic and foreign body giant cell reaction, and lymphoplasmacytic and acute inflammation with focal dystrophic calcification; there was no other evidence of malignancy.
Figure 1.

Computed tomography scan revealing a 5-cm cystic mass anterior to the rectus muscle (A, arrow) in continuity with a 10.4 × 9.3-cm intra-abdominal cystic mass containing a posterior 3.7 × 2.8-cm soft-tissue density component abutting the bladder dome, shown in sagittal (B, arrow) and axial (C) views.
Figure 2.
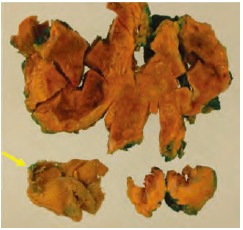
Gross pathologic examination revealing a retained surgical sponge (arrow).
Gross pathologic examination revealed a retained surgical gauze within the mass, presumably from her prior gynecologic surgery.
Discussion
The term gossypiboma has been used to describe a mass comprising retained surgical sponge material and surrounding reactive tissue.1 Most commonly, gossypibomas are due to retained laparotomy sponges identified in the abdominal or pelvic cavity. The reported incidence varies considerably, ranging between 1 in 300 and 1 in 1000 of all surgical interventions, and between 1 in 1000 and 1 in 1500 intraabdominal operations2; however, the true incidence is likely underreported due to potential medicolegal implications of reporting an avoidable error, and due to some patients who remain asymptomatic and are thus never discovered to harbor gossypibomas.4 Histologically, two types of foreign body reactions have been identified, including an exudative inflammatory reaction with abscess formation and an aseptic fibrinous reaction that tends to present much later and may be associated with adhesions or granuloma formation.5 Frequently, diagnosis is made via imaging, including plain films, ultrasonography, CT, or magnetic resonance imaging. Use of CT, as in our case, may reveal findings characteristic of intra-abdominal abscesses, such as air bubbles, calcifications, or rim enhancement with contrast.6 The most common site for gossypiboma is the abdominal and pelvic cavity; however, other sites of gossypiboma have included the thorax, neck, and even the orbital cavity.2 Several complications have been described, including fistula formation, foreign body migration, small bowel obstruction, abscess formation, and chronic pain. In rare instances, intraluminal migration of surgical gauze into the urinary bladder7 or urethra8 has been reported.
Gross pathologic examination revealed a retained surgical gauze within the mass, presumably from her prior gynecologic surgery.
Strategies to help prevent retained surgical materials include use of radiologically opaque sponges, methodologic examination by the operator, avoidance of small sponges in abdominal surgery whenever possible, and meticulous counting of instruments and sponges both prior to and following surgery.
Factors identified on multivariable analysis to increase the risk of gossypibomas include emergency surgery (relative risk [RR] 8.8; 95% confidence interval [CI], 2.4-31.9), unplanned changes during surgery (RR 4.1; 95% CI, 1.4-12.4), and patient obesity (RR for each one-unit increment in body-mass index 1.1; 95% CI, 1.0-1.2).9 Other factors associated with risk of gossypiboma include disorganization, poor communication, and inadequate or inexperienced staff in the operating room. Strategies to help prevent retained surgical materials include use of radiologically opaque sponges, methodologic examination by the operator, avoidance of small sponges in abdominal surgery whenever possible, and meticulous counting of instruments and sponges both prior to and following surgery.10 Sponges with tracking bar codes have been proposed; however, these can be subject to degradation over time and may not always be apparent on radiographic imaging postoperatively. Gossypiboma is completely preventable and relies most critically on thorough surgical exploration and accurate instrument count prior to abdominal closure.
Conclusions
Gossypiboma is an uncommon, yet avoidable surgical diagnosis that frequently poses a diagnostic dilemma. Gossypiboma may be misdiagnosed as a malignant tumor necessitating invasive interventions. Gossypiboma should be suspected in the differential diagnosis of abdominal masses in patients who have undergone previous surgery, particularly in regions of the world in which radio-opaque markers on surgical sponges may not be in routine use. Strict adherence to universal guidelines for instrument counts in the operating room and a meticulous exploration of the abdominal cavity prior to closure are key to prevention of gossypiboma.
Main Points.
Gossypiboma is defined as a mass arising from a cottonoid matrix, most commonly a retained surgical sponge, and surrounding inflammation. The reported incidence varies between 1 in 1000 and 1 in 1500 intra-abdominal operations, though these figures may be underestimates.
Symptoms related to gossypiboma may be absent or nonspecific. Imaging studies, such as computed tomography, may be helpful in revealing abnormalities, but the differential diagnosis may remain broad.
Management of gossypiboma consists of surgical removal in order to definitively establish the diagnosis and avoid potentially life-threatening complications.
Strict adherence to universal guidelines for instrument counts in the operating room and a meticulous exploration of the abdominal cavity prior to closure are key to prevention of gossypiboma.
References
- 1.Topal U, Gebitekin C, Tuncel E. Intrathoracic gossypiboma. AJR Am J Roentgenol. 2001;177:1485–1486. doi: 10.2214/ajr.177.6.1771485. [DOI] [PubMed] [Google Scholar]
- 2.Lincourt AE, Harrell A, Cristiano J, et al. Retained foreign bodies after surgery. J Surg Res. 2007;138:170–174. doi: 10.1016/j.jss.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Srivastava KN, Agarwal A. Gossypiboma posing as a diagnostic dilemma: a case report and review of the literature. Case Rep Surg. 2014;2014:713428. doi: 10.1155/2014/713428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uluçay T, Dizdar MG, SunayYavuz M, Asirdizer M. The importance of medico-legal evaluation in a case with intraabdominal gossypiboma. Forensic Sci Int. 2010;198:e15–e18. doi: 10.1016/j.forsciint.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Rappaport W, Haynes K. The retained surgical sponge following intra-abdominal surgery. A continuing problem. Arch Surg. 1990;125:405–407. doi: 10.1001/archsurg.1990.01410150127025. [DOI] [PubMed] [Google Scholar]
- 6.Sheward SE, Williams AG, Mettler FA, Lacey SR. CT appearance of a surgically retained towel (gossypiboma) J Comput Assist Tomogr. 1986;10:343–345. doi: 10.1097/00004728-198603000-00038. [DOI] [PubMed] [Google Scholar]
- 7.Kato K, Kawai T, Suzuki K, et al. Migration of surgical sponge retained at transvaginal hysterectomy into the bladder: a case report [in Japanese] Hinyokika Kiyo. 1998;44:183–185. [PubMed] [Google Scholar]
- 8.Lin TY, Chuang CK, Wong YC, Liao HC. Gossypiboma: migration of retained surgical gauze and spontaneous transurethral protrusion. BJU Int. 1999;84:879–880. doi: 10.1046/j.1464-410x.1999.00335.x. [DOI] [PubMed] [Google Scholar]
- 9.Gawande AA, Studdert DM, Orav EJ, et al. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229–235. doi: 10.1056/NEJMsa021721. [DOI] [PubMed] [Google Scholar]
- 10.Gibbs VC, Coakley FD, Reines HD. Preventable errors in the operating room: retained foreign bodies after surgery—Part I. Curr Probl Surg. 2007;44:281–337. doi: 10.1067/j.cpsurg.2007.03.002. [DOI] [PubMed] [Google Scholar]


