Abstract
Early diagnosis of bacteremia for patients with suspected sepsis is 1 way to improve prognosis of sepsis. Systemic inflammatory response syndrome (SIRS) has long been utilized as a screening tool to detect bacteremia by front-line healthcare providers. The value of SIRS to predict bacteremia in elderly patients (≥65 years) with suspected sepsis has not yet been examined in emergency departments (EDs).
We aimed to evaluate the performance of SIRS components in predicting bacteremia among elderly patients in EDs.
We retrospectively evaluated patients with suspected sepsis and 2 sets of blood culture collected within 4 hours after admitting to ED in a tertiary teaching hospital between 2010 and 2012. Patients were categorized into 3-year age groups: young (18–64 years), young-old (65–74 years), and old patients (≥75 years). Vital signs and Glasgow Coma Scale with verbal response obtained at the triage, comorbidities, sites of infection, blood cultures, and laboratory results were retrieved via the electronic medical records.
A total of 20,192 patients were included in our study. Among them, 9862 (48.9%) were the elderly patients (young-old and old patients), 2656 (13.2%) developed bacteremia. Among patients with bacteremia, we found the elderly patients had higher SIRS performance (adjusted odds ratio [aOR]: 2.40, 95% confidence interval [CI]: 1.90–3.03 in the young-old and aOR: 2.66, 95% CI: 2.19–3.23 in the old). Fever at the triage was most predictive of bacteremia, especially in the elderly patients (aOR: 2.19, 95% CI: 1.81–2.65 in the young-old and aOR: 2.27, 95% CI: 1.95–2.63 in the old), and tachypnea was not predictive of bacteremia among the elderly patients (all P > 0.2).
The performance of SIRS to predict bacteremia was more suitable for elderly patients in EDs observed in this study. The elderly patients presented with more fever and less tachypnea when they had bacteremia.
Keywords: bacteremia, elderly, emergency department, old, systemic inflammatory response syndrome, young-old
1. Introduction
Bacteremia is a major issue in daily practice at the critical care settings such as emergency departments (EDs). Diagnosis of bacteremia with early adequate antibiotic use can increase survival in patients with sepsis.[1] In order to replace the time-consuming conventional blood culture methods, many studies attempted to develop predictive models or biomarkers to risk stratify or early detect patients with bacteremia,[2–7] and some of them focused on the elderly patients.[8,9] Due to the growing population over the age of 65 years worldwide, special attentions for elderly patients (≥65 years) is necessary. Early detection for bacteremia in elderly patients is more difficult than in younger population because they commonly have vague statements of symptoms due to declined cognition, altered consciousness, or atypical symptoms and signs.[10–12]
Systemic inflammatory response syndrome (SIRS) is closely related to sepsis, and the criteria of SIRS to define sepsis were proposed by the consensus conference of the American College of Chest Physicians in 1992.[13] After Rangel-Frausto discussed about progression of SIRS, sepsis, severe sepsis, and septic shock,[14] there were many studies worked on the predictive value of SIRS to severe sepsis and found that SIRS had less predictive value for severe sepsis or septic shock.[15,16] However, SIRS was regarded as an adequate predictor for bacteremia in some studies,[17,18] and we found there was no study focused on performance of SIRS in elderly patients with bacteremia in EDs. Due to the great challenge of early diagnosing bacteremia of elderly patients in EDs, we aimed to evaluate the components of SIRS and their performance in predicting bacteremia among elderly patients in EDs.
2. Methods
2.1. Patients and setting
We collected data of patients admitted to the ED of Chang Gung Memorial Hospital in Linkou, a tertiary academic medical center in Northern Taiwan serving approximately 180,000 patients in ED annually. We reviewed electronic medical charts and constructed a retrospective cohort study from 2010 to 2012. Two-step inclusion algorithm was utilized in this study: all adult patients (older than 18 years) with international classification of disease, 9th revision, clinical modification (ICD-9-CM) diagnosis codes of infectious diseases (appendix 1); patients with clinically suspected bacteremia as indicated by 2 sets of blood cultures ordered on physician's discretion within 4 hours after admitting to ED. Patients who had cardiac arrest before ED visit and visited ED owing to traumatic injury were excluded from this study. Only the first ED visit of each patient during the study period was included in the final analysis. The institutional review board of the Chang Gung Memorial Hospital approved the study and waived requirement for informed consent.
2.2. Measurements
The vital signs and Glasgow Coma Scale with verbal response at the triage, basic demographic data, comorbidities, sites of infection, laboratory, and microbiological results and the final discharge status were retrieved via the electronic medical records (EMRs) for all patients. All variables were defined before data collected and recorded in a standardized format during information collection. Structured Query Language was utilized by trained research coordinators with predefined data collection forms to retrieve EMRs, and EMRs were stored in Microsoft Access (Microsoft, Redmond, WA) for subsequent chart review and data management. The data abstractors were blinded to the study objectives and hypothesis. Different program codes were used to double-check the results of the EMRs. Charlson Comorbidity Index (CCI) was obtained from ICD-9-CM diagnosis codes the patients ever had in the EMRs. The SIRS criteria were defined as more than one of the below parameters met: body temperature more than 38 or less than 36 °C; heart rate more than 90 bpm; tachypnea with respiratory rate more than 20 bpm; and white blood cell count greater than 12,000/mm3 or below 4000/mm3 or band form greater than 10% as established by the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference in 1992. Presumed sites of infection were identified as ED diagnoses and categorized into respiratory, genitourinary, soft tissue, intra-abdominal, others (such as meningitis and osteomyelitis), and unknown origin.
2.3. Criteria for bacteremia
Bacteremia was defined as both 2 sets of blood culture grew the same microorganism or 1 set of blood culture had bacteria except possible contaminated resource, that is, coagulase-negative Staphylococci, Corynebacterium species, Propionibacterium species, Bacillus species, Aerococcus species, and Micrococcus species. Blood cultures were verified from the microbiology laboratory database, and results were confirmed by the microbiology laboratory.
2.4. Mortality
The mortality record was retrieved from the EMRs and classified into 3 groups; within 24 hours, 72 hours, and 28 days after admitting to ED. Patients discharged critically were categorized in the mortality group.
2.5. Statistical analysis
Statistical analysis was performed with R software version 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria) and STATA 13.0 (StataCorp, College Station, TX). Descriptive analysis was used to summarize the demographics and characteristics of our patients with 3 age groups as young (18–64 years), young-old (65–74 years), and old (75 years and over). Categorical variables were reported as number and percentages. Continuous variables were reported as mean and standard deviation. Continuous variables of clinical data were converted into categorical variables by cutoff points, which referred to clinical practice, protocols in other studies, or associated laboratory references. The categorical variables were examined by chi-square test or Fisher exact test when appropriate. A linear association between the row categorical variable and the column categorical variable were examined by Mantel–Haenszel chi-square test. An Allen-Cady backward stepwise multivariable logistic regression was used to adjust potential confounders between bacteremia and components of SIRS criteria, for example, comorbidities using CCI, DM, and history of malignancy, sites of infection, and verbal response at the triage. Interaction between SIRS score and age groups was examined by multivariable logistic regression. We also performed another Allen-Cady backward stepwise multivariable logistic regression to analyze the risk factors between 28-day mortality and bacteremia, components of SIRS criteria, age categories, comorbidities, sites of infection, and verbal response at the triage.
3. Results
From 2010 to 2012, 130,869 patients visited our ED with infection. Among them, 110,378 patients were excluded due to either younger than 18 years old, visiting ED owing to traumatic injury, out-of-hospital cardiac arrest, or not drawing blood cultures within 4 hours after admitting to ED. After further excluding 299 patients with incomplete data or uncertain discharge time (1.5%), 20,192 patients were included in our final analysis (Fig. 1).
Figure 1.
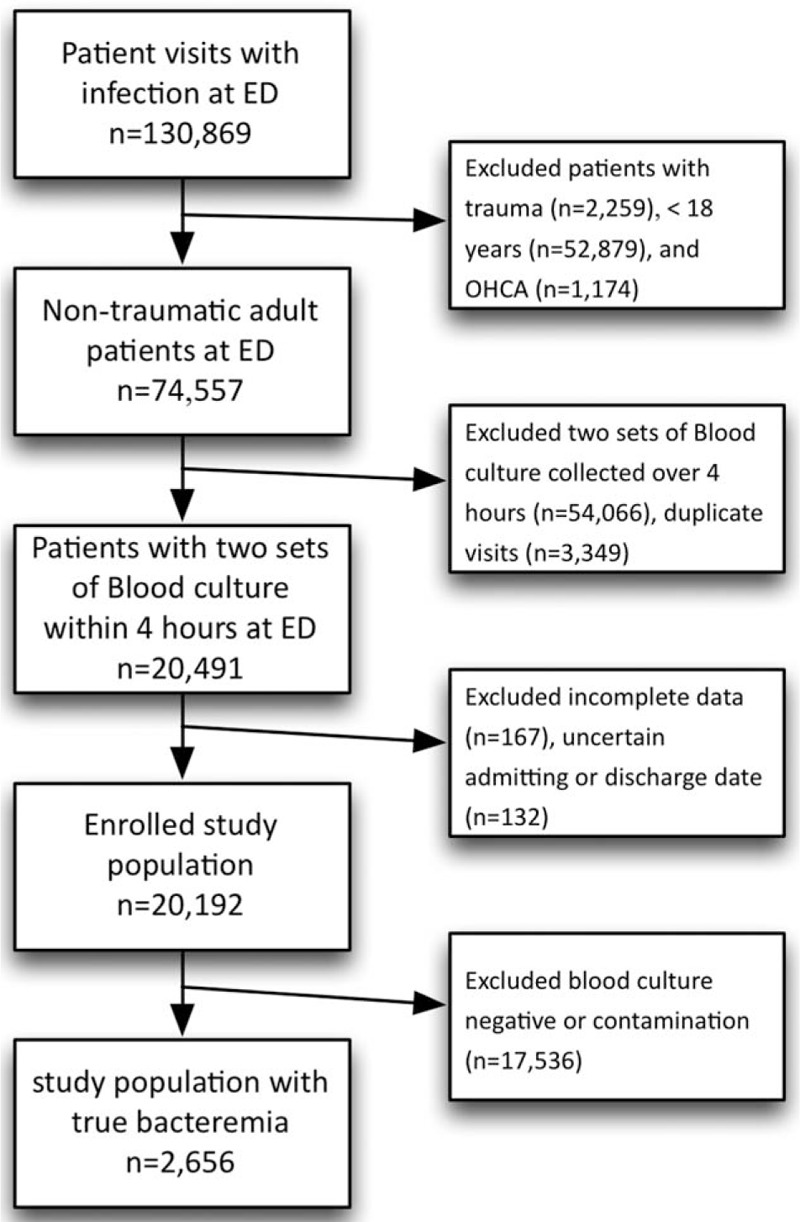
Flowcharts of enrollment of study population.
3.1. Patient characteristics
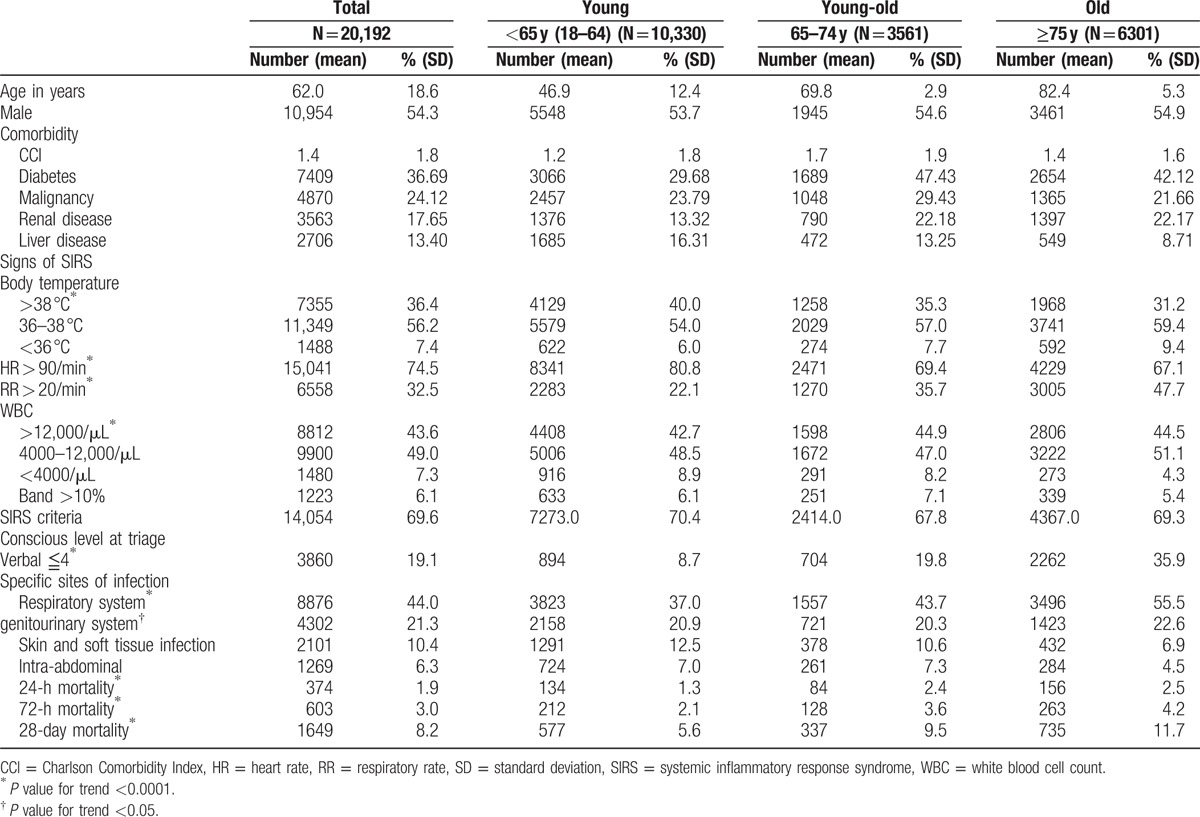
In 20,192 enrolled patients, 10,954 were male (54.3%), and the mean age was 62 ± 18.6 (standard deviation) years (Table 1). Of all patients, 10,330 (51.2%) were younger than 65 years, 3561 (17.6%) between 65 and 74 years and 6301 (31.2%) older than 75 years. No gender difference was found in all 3 age groups. Highest CCI was observed in the young-old group (young: 1.2, young-old: 1.7, and old: 1.4; P < 0.0001). The young-old group also had highest proportion of diabetes (47.43%, P < 0.0001) and malignancy (29.43%, P < 0.0001). The trend of impaired consciousness with manifestation of declined verbal response at the triage was significant. In the old group, there was almost 1/3 patients could not converse normally or were not verbally oriented (young: 8.65%, young-old: 19.77%, and old: 35.90%; P for trend <0.0001). The most common site of infection overall was respiratory tract infection (44%), and it was found in more than half of the old group (55.5%, P < 0.0001). Genitourinary system was the second most common site of infection (21%), and there was a trend toward more prevalence among the older patient groups (P = 0.02).
Table 1.
Basic characteristics of study population stratified by age groups.
3.2. Bacteremia
In 20,192 enrolled patients, bacteremia was confirmed by the microbiology laboratory in 2656 patients (13.15%). The percentage of bacteremia in the young group was 12.11% (N = 1251), and patients in young-old and old groups had higher percentage of bacteremia (15.84%, N = 564 and 13.35%, N = 841, respectively, P < 0.0001, Table 2). Gram-negative bacteremia accounted for the largest proportion of bacteremia (65.4%, Table 2).
Table 2.
SIRS of patients with bacteremia stratified by age groups.
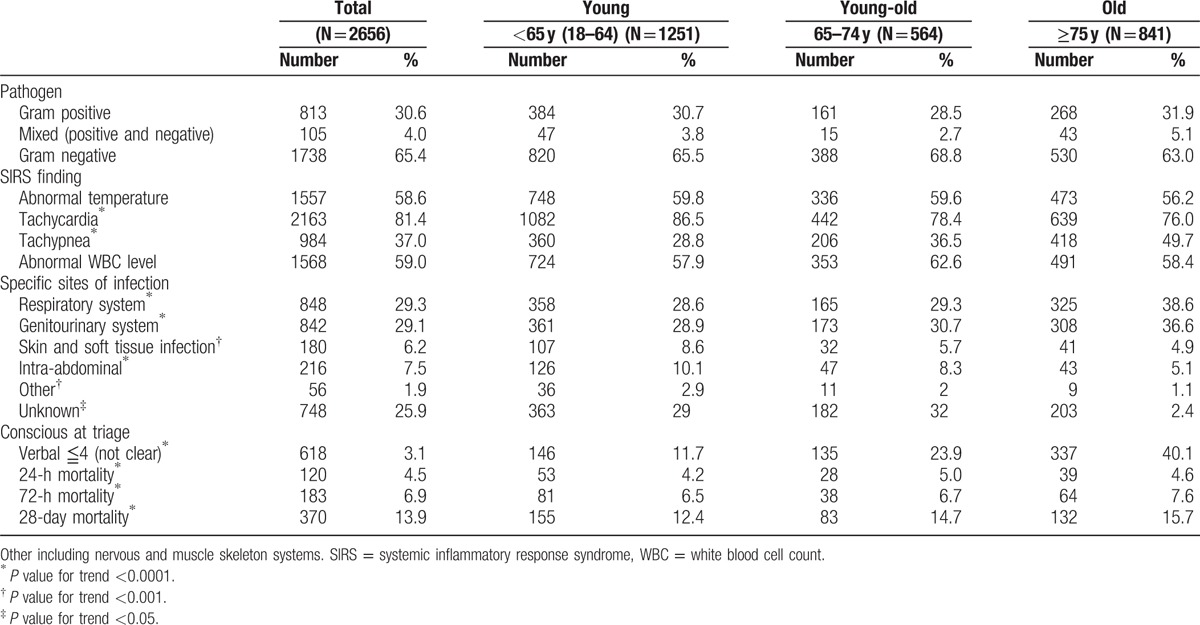
3.3. SIRS criteria
There were nearly 2/3 of all enrolled patients with clinically suspected sepsis met the SIRS criteria (N = 14,054, 69.6%). The elderly patients were less likely to have abnormal body temperature, tachycardia, or abnormal white blood cell count but more likely to have tachypnea (all P for trend <0.0001, Table 1). Among patients with confirmed bacteremia, the elderly patients tended to be less likely to present with tachycardia but more like to present with tachypnea (young: 28.8%, young-old: 36.5%, and old: 49.7%; P < 0.0001, Table 2).
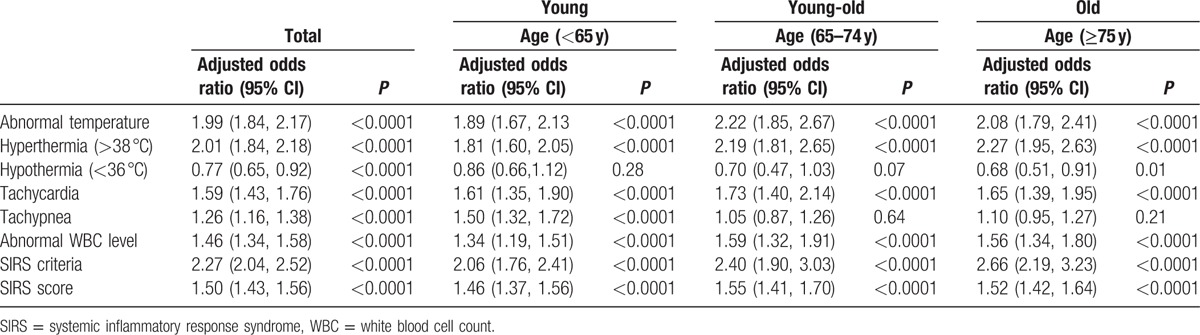
Table 3 illustrated the performance of SIRS score to predict bacteremia among patients with suspected sepsis in different age groups. Overall, SIRS was marginally more likely to predict bacteremia among the elderly patients, compared to young patients (adjusted area under the curve: 0.63 vs 0.60, adjusted for site of infection and comorbidities). SIRS performed better among the elderly patients (young: adjusted odds ratio [aOR] 2.06, young-old: aOR 2.40, and old: aOR 2.66). Abnormal body temperature at the triage was most predictive of bacteremia, especially in the young-old group (aOR: 2.22, 95% confidence interval [CI]: 1.85–2.67, all P < 0.0001, adjusting for CCI, comorbidities, site of infection, and verbal response, same adjustment for aOR below). Hyperthermia (>38 °C) indicated the highest risk for bacteremia in the old group (aOR: 2.27, 95% CI: 1.95–2.63, all P < 0.0001, interaction P = 0.003). On the contrary, hypothermia (<36 °C) was associated negative blood culture results among the old patient groups (old group aOR: 0.68, 95% CI: 0.51–0.91, P = 0.01). Tachycardia and abnormal white blood cell count were both risk factors for bacteremia for the elderly patients but not as significant as abnormal body temperature (all P < 0.0001), and both were more likely to be found in the young-old group than in the old group. Lastly, tachypnea was least predictive of bacteremia among the elderly patients (all P > 0.2, Table 3).
Table 3.
The performance of SIRS score to predict bacteremia among patient with suspected sepsis in different age groups.
3.4. Mortality
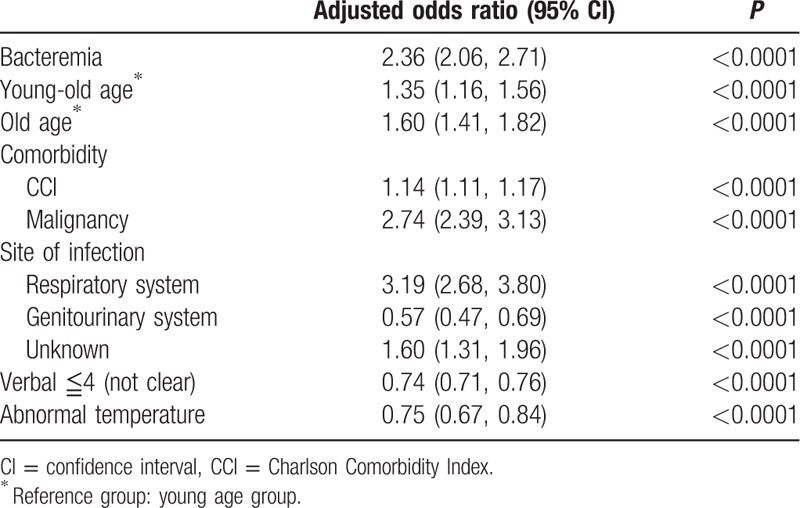
The mortality rate of all enrolled patients within 24 hours after admission to our ED was 1.9%, and the mortality rate was higher among the elderly patients (young: 1.3%, young-old: 2.4%, and old: 2.5%; P for trend <0.0001, Table 1). The same trends were also observed in mortality within 72 hours (P for trend = 0.04), and within 28 days (P for trend <0.0001, Table 1). Table 2 showed the mortality rates of patients with confirmed bacteremia. Similarly, the elderly groups had higher mortality within 24 hours, 72 hours, and 28 days (all P for trend <0.0001). Furthermore, in the final multivariable logistic regression model, we found that the 28-day mortality was positively associated with bacteremia, age, CCI, malignancy, and respiratory and unknown site of infection, and negatively associated with genitourinary site of infection, and verbal response and body temperature at the triage (all P < 0.001, Table 4).
Table 4.
Multivariable logistic regression evaluating the association between 28-day mortality and risk factors.
4. Discussion
Due to the rapid growing of elderly population (aged over 65 years), we encounter increasing proportion of elderly patient in ED.[19] SIRS, a combination of physiological responses to a nonspecific insult of either infectious or noninfectious, had been thought to be predictive of severity of infection such as bacteremia.[7,20] In this retrospective cohort study, we illustrated the capacity of SIRS criteria to predict bacteremia in the elderly patients in ED. We found the elderly patients with suspected sepsis had less abnormal body temperature, tachycardia or abnormal white blood cell count but more tachypnea than the young patients. Furthermore, the SIRS criteria were more likely to predict bacteremia among the elderly patients. Lastly, after adjusting for potential confounders, hyperthermia was more predictive of laboratory-confirmed bacteremia among the elderly patients than the young group. Surprisingly, tachypnea was found unlikely to be predictive of bacteremia among the elderly patients.
Abnormal vital signs are commonly used to predict the severity of infection.[21] The relationship between fever and bacteremia has been examined in some studies, and some indicated that fever had no predictive value for bacteremia in adults, especially for catheter-related bacteremia.[22–24] In our study, we observed that the elderly patients with suspected bacteremia were less likely to present with fever. This phenomenon could be explained by the blunted response to endogenous pyrogens with aging or the lower baseline body temperature of the elder population.[25,26] It could also be possible that clinician would be more cautious to survey the possibility of bacteremia among the elderly in our ED. Furthermore, bacteremia was more likely to be associated with fever among the elderly than the young patients in our study, which was also seen in Tomohiro study.[24]
Tachycardia is one of the physiological effects of endogenous mediators induced by inflammation and has been found as an independent factor of mortality for elderly patients with infection.[27] It is also associated with bacteremia for all patients independent of their age.[28,29] In our study, tachycardia was less likely to be observed in elderly patients, but more indicative for bacteremia than the young group. As Green et al[30] observed decreased likelihood of tachycardia in octogenarians with bacteremia, the old group with tachycardia in our study also had less risk of bacteremia than the young-old group (old group aOR: 1.65, 95% CI: 1.39–1.95, P<0.0001). This phenomenon could be explained by multiple factors associated with heart rates among the elderly patients, including declining intrinsic heart rate, changes in response to adrenergic mediated stress, or medication for chronic disease.[31]
In our study, the elderly patients with suspected bacteremia tended to present with tachypnea and had higher probability to suffer from respiratory tract infection. However, tachypnea was not a significant predictor for bacteremia in the elderly patients after adjustment for comorbidities, sites of infection, and verbal response in our study. The medical comorbidities could potential influence the baseline respiratory rate, and we observed elderly patients did have higher CCI.[32] Although tachypnea had been thought one of the host responses to severe infection,[27,33] it was not a significant predictor of mortality.[30] Further studies to clarify for this phenomenon is merited.
The only criterion of SIRS requiring laboratory confirmation is white blood cell count or bandemia. In the present study, we did not find the phenomenon of blunt leukocytosis in elderly patients with suspected bacteremia as Lai et al[34] on 2011, and abnormal white blood count and bandemia in the elderly patients is a weak predictor to bacteremia in our study (young-old group aOR: 1.59, 95% CI: 1.32–1.91; old group aOR: 1.56, 95% CI: 1.34–1.80, P<0.0001 and P<0.0001, compared to the young group). Furthermore, we found that leukocytosis was more important among the young-old patients, of whom more diabetes, malignancy and other comorbidities were found. Complicated interaction between aging and these comorbidities might be the reason of this phenomenon and needs further studies to disentangle.
Altered mental status could serve as an indicator of mortality for elderly patients with bacteremia.[35–38] In our study population, we observed patients with bacteremia also had the trend of declined verbal response with aging. Progressive degeneration or previous neurovascular event could make the elderly have trouble in communication and verbal response, which might be worsened by bacteremia. This condition will make a dilemma about early diagnosis and treatment for the elderly patients with bacteremia.
As illustrated, we observed higher probability of bacteremia in elderly patients. Respiratory tract infection was the most common suspected source for bacteremia, especially in the elderly patients. We found both respiratory tract and urogenital system infection were common sources of bacteremia in the elderly patients. It may be related to institution resident or indwelling urinary catheters usually seen in the elderly patients and increases the risk of catheter-associated infection, but we did not verify that from EMRs in this study. Other possible hypotheses include lower sensitivity of the immune system, changes in host defense mechanism and increased incidences of underlying illness, which might explain the lower resistance to infection among the elderly patients.[39]
This study showed the trend of increasing mortality with age among patients with suspected sepsis and laboratory-confirmed bacteremia. The elderly had higher mortality rate compared to the younger patients in 24 hours, 72 hours, and 28 days after admitting to ED significantly. Some unique aspects of infections in the elderly, such as reduced physiologic reserve capacity of aging, may contribute to higher morbidity and mortality in this population.[40] Hence, early diagnosis of bacteremia for the front-line emergency physicians in order to start adequate management for the elderly patients with sepsis to improve outcome is mandatory.
5. Limitation
There were some limitations in our study. First, due to all the data were retrieved via the EMRs, there was incomplete information regarding patient sources and the prevalence of indwelling urinary catheter. Second, respiratory rate was counted by triage nurses visually and was not highly reliable, which could potentially contribute to its poor performance to predict bacteremia. Third, we may underestimate the prevalence of fever at the triage because patients may have antipyretic before visiting ED, which could also influence the performance of hyperthermia to predict bacteremia. Fourth, although we have attempted to adjust the potential confounders such as comorbidities, we caution the reader to generalize our results before comparing their own patient population. Lastly, although we included patients with infectious diseases and clinically suspected bacteremia as indicated by 2 sets of blood cultures ordered on physician's discretion and excluded patients who had cardiac arrest before ED visit and visited ED owing to traumatic injury, it is still possible that bacteremia is a secondary effect that associated with diseases and disorders accompanied with SIRS other than infections.
6. Conclusion
In conclusion, the elderly patients usually present vague symptoms and signs of sepsis. SIRS is slightly more accurate to predict bacteremia for the elderly patients with suspected sepsis in ED. If the elderly patients present with fever or tachycardia they have higher possibility to have bacteremia.
Acknowledgment
The authors thank Mr Bin-Zhe Hong for the assistance of statistics.
Footnotes
Abbreviation: aOR = adjusted odds ratio, CCI = Charlson comorbidity index, CI = confidence interval, ED = emergency department, EMRs = electronic medical records, SIRS = systemic inflammatory response syndrome.
S-TH, C-FY, and I-ST have contributed equally to the article.
Funding/support: This study was supported by the National Science Council and Chang Gung Memorial Hospital in Taiwan (100-2314-B-182A-038-MY3, CMRPG2C0202, CIRPG2E0022, CMRPG2B0124, CMRPG2B0273, CMRPG2B0373, and CPRPG2D0012).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
References
- [1].Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 2010;38:1045–53. [DOI] [PubMed] [Google Scholar]
- [2].Morrison J, Zweitzig D, Riccardello N, et al. Retrospective analysis of clinical data associated with patients enrolled in a molecular diagnostic feasibility study highlights the potential utility for rapid detection of bloodstream infection. Am J Emerg Med 2014;32:511–6. [DOI] [PubMed] [Google Scholar]
- [3].Hoenigl M, Raggam RB, Wagner J, et al. Diagnostic accuracy of soluble urokinase plasminogen activator receptor (suPAR) for prediction of bacteremia in patients with systemic inflammatory response syndrome. Clin Biochem 2013;46:225–9. [DOI] [PubMed] [Google Scholar]
- [4].Bell K, Wattie M, Byth K, et al. Procalcitonin: a marker of bacteraemia in SIRS. Anaesth Intensive Care 2003;31:629–39. [DOI] [PubMed] [Google Scholar]
- [5].Lin KJ, Lin J, Hanasawa K, et al. Interleukin-8 as a predictor of the severity of bacteremia and infectious disease. Shock 2000;14:95–100. [DOI] [PubMed] [Google Scholar]
- [6].Falguera M, Trujillano J, Caro S, et al. A prediction rule for estimating the risk of bacteremia in patients with community-acquired pneumonia. Clin Infect Dis 2009;49:409–16. [DOI] [PubMed] [Google Scholar]
- [7].Wildi K, Tschudin-Sutter S, Dell-Kuster S, et al. Factors associated with positive blood cultures in outpatients with suspected bacteremia. Eur J Clin Microbiol Infect Dis 2011;30:1615–9. [DOI] [PubMed] [Google Scholar]
- [8].Marti L, Cervera C, Filella X, et al. Cytokine-release patterns in elderly patients with systemic inflammatory response syndrome. Gerontology 2007;53:239–44. [DOI] [PubMed] [Google Scholar]
- [9].Lai CC, Chen SY, Wang CY, et al. Diagnostic value of procalcitonin for bacterial infection in elderly patients in the emergency department. J Am Geriatr Soc 2010;58:518–22. [DOI] [PubMed] [Google Scholar]
- [10].Wester AL, Dunlop O, Melby KK, et al. Age-related differences in symptoms, diagnosis and prognosis of bacteremia. BMC Infect Dis 2013;13:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Fontanarosa PB, Kaeberlein FJ, Gerson LW, et al. Difficulty in predicting bacteremia in elderly emergency patients. Ann Emerg Med 1992;21:842–8. [DOI] [PubMed] [Google Scholar]
- [12].Girard TD, Opal SM, Ely EW. Insights into severe sepsis in older patients: from epidemiology to evidence-based management. Clin Infect Dis 2005;40:719–27. [DOI] [PubMed] [Google Scholar]
- [13].Bone RC BR, Cerra FB, Dellinger RP, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992;101:1644–55. [DOI] [PubMed] [Google Scholar]
- [14].Rangel-Frausto MS, Pittet D, Costigan M, et al. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA 1995;273:117–23. [PubMed] [Google Scholar]
- [15].Gille-Johnson P, Hansson KE, Gardlund B. Severe sepsis and systemic inflammatory response syndrome in emergency department patients with suspected severe infection. Scand J Infect Dis 2013;45:186–93. [DOI] [PubMed] [Google Scholar]
- [16].Bossink AW, Groeneveld AB, Koffeman GI, et al. Prediction of shock in febrile medical patients with a clinical infection. Crit Care Med 2001;29:25–31. [DOI] [PubMed] [Google Scholar]
- [17].Leth RA, Forman BE, Kristensen B. Predicting bloodstream infection via systemic inflammatory response syndrome or biochemistry. J Emerg Med 2013;44:550–7. [DOI] [PubMed] [Google Scholar]
- [18].Jones GR, Lowes JA. The systemic inflammatory response syndrome as a predictor of bacteraemia and outcome from sepsis. Q J Med 1996;89:515–22. [DOI] [PubMed] [Google Scholar]
- [19].George G, Jell C, Todd BS. Effect of population ageing on emergency department speed and efficiency: a historical perspective from a district general hospital in the UK. Emerg Med J 2006;23:379–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Baitello AL, Colleoni Neto R, Herani Filho B, et al. Bacteremia—prevalence and associated factors in patients with acute calculous cholecystitis. Rev Assoc Med Bras 2004;50:373–9. [DOI] [PubMed] [Google Scholar]
- [21].Nolt BR, Gonzales R, Maselli J, et al. Vital-sign abnormalities as predictors of pneumonia in adults with acute cough illness. Am J Emerg Med 2007;25:631–6. [DOI] [PubMed] [Google Scholar]
- [22].Al-Solaiman Y, Estrada E, Allon M. The spectrum of infections in catheter-dependent hemodialysis patients. Clin J Am Soc Nephrol 2011;6:2247–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Coburn B, Morris AM, Tomlinson G, et al. Does this adult patient with suspected bacteremia require blood cultures? JAMA 2012;308:502–11. [DOI] [PubMed] [Google Scholar]
- [24].Taniguchi T, Tsuha S, Takayama Y, et al. Shaking chills and high body temperature predict bacteremia especially among elderly patients. Springerplus 2013;2:624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Castle SC, Norman DC, Yeh M, et al. Fever response in elderly nursing home residents: are the older truly colder? J Am Geriatr Soc 1991;39:853–7. [DOI] [PubMed] [Google Scholar]
- [26].Gomolin IH, Aung MM, Wolf-Klein G, et al. Older is colder: temperature range and variation in older people. J Am Geriatr Soc 2005;53:2170–2. [DOI] [PubMed] [Google Scholar]
- [27].Caterino JM, Kulchycki LK, Fischer CM, et al. Risk factors for death in elderly emergency department patients with suspected infection. J Am Geriatr Soc 2009;57:1184–90. [DOI] [PubMed] [Google Scholar]
- [28].Lee CC, Chen SY, Chang IJ, et al. Comparison of clinical manifestations and outcome of community-acquired bloodstream infections among the oldest old, elderly, and adult patients. Medicine 2007;86:138–44. [DOI] [PubMed] [Google Scholar]
- [29].Phua J, Ngerng W, See K, et al. Characteristics and outcomes of culture-negative versus culture-positive severe sepsis. Crit Care 2013;17:R202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Green JE, Ariathianto Y, Wong SM, et al. Clinical and inflammatory response to bloodstream infections in octogenarians. BMC Geriatr 2014;14:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Christou DD, Seals DR. Decreased maximal heart rate with aging is related to reduced {beta}-adrenergic responsiveness but is largely explained by a reduction in intrinsic heart rate. J Appl Physiol 19852008;105:24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- [33].Cardoso T, Teixeira-Pinto A, Rodrigues PP, et al. Predisposition, insult/infection, response and organ dysfunction (PIRO): a pilot clinical staging system for hospital mortality in patients with infection. PLoS One 2013;8:e70806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Lai WA, Chen SF, Tsai NW, et al. Clinical characteristics and prognosis of acute bacterial meningitis in elderly patients over 65: a hospital-based study. BMC Geriatr 2011;11:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Deulofeu F, Cervelló B, Capell S, et al. Predictors of mortality in patients with bacteremia: the importance of functional status. J Am Geriatr Soc 1998;46:14–8. [DOI] [PubMed] [Google Scholar]
- [36].Rebelo M, Pereira B, Lima J, et al. Predictors of in-hospital mortality in elderly patients with bacteraemia admitted to an Internal Medicine ward. Int Arch Med 2011;4:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Calle A, Márquez MA, Arellano M, et al. Geriatric assessment and prognostic factors of mortality in very elderly patients with community-acquired pneumonia. Arch Bronconeumol 2014;50:429–34. [DOI] [PubMed] [Google Scholar]
- [38].Ruiz LA, Zalacain R, Capelastegui A, et al. Bacteremic pneumococcal pneumonia in elderly and very elderly patients: host- and pathogen-related factors, process of care, and outcome. J Gerontol A Biol Sci Med Sci 2014;69:1018–24. [DOI] [PubMed] [Google Scholar]
- [39].Nasa P, Juneja D, Singh O. Severe sepsis and septic shock in the elderly: an overview. World J Crit Care Med 2012;1:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Yoshikawa TT. Epidemiology and unique aspects of aging and infectious diseases. Clin Infect Dis 2000;30:931–3. [DOI] [PubMed] [Google Scholar]


