Abstract
Rationale:
Ethambutol-induced optic neuropathy (EON) is a well-known complication that results from the use of ethambutol. The ocular manifestations of EON include painless loss of central vision and cecocentral scotomas in the visual field.
Patient concerns:
A 75-year-old Chinese Han man suffered from this rare ocular disorder because he took ethambutol for about 8 months.
Diagnoses:
He was diagnosed as EON based on series of ophthalmic examinations performed.
Interventions:
Since he has stopped taking this drug for 3 months, we just offered some neurotrophic agents to him.
Outcomes:
One month later, he came back for return visit. The ophthalmic examinations indicated recovery of the visual function very well.
Lessons:
The EON is a reversible optic neuropathy if the ocular toxicity is monitored closely among the tuberculosis patients that take ethambutol.
Keywords: ethambutol-induced optic neuropathy, retinal nerve fiber layer, visual field
1. Introduction
Tuberculosis that is caused by Mycobacterium is one of the most important systemic infections around the world.[1] Ethambutol is a first-line medication that is used in the tuberculosis therapies. However, it can lead to side effects including problems with vision, liver problems, and allergies.[2] Ethambutol-induced optic neuropathy (EON) is a well-known complication arising from the use of ethambutol, the severity of which is in a dose-dependent manner. The toxicity is usually reversible on discontinuation of the therapy.[3] However, there have been several reports of permanent damage to the visual function.[4,5] The clinical characteristics of EON include painless loss of central vision and cecocentral scotomas in the visual field. There have been several studies regarding the incidence of EON in different countries, which is close to 1%.[6,7] However, there have been rare case reports on the clinical features and prognosis of EON in the Chinese Han population till now.[8] In the present case report, we aimed to report 1 EON case that came to our hospital recently to evaluate the clinical characteristics of EON in Chinese patients and the natural course of the disease. Also, we provided a brief review on the current knowledge in the field.
2. Case presentation
A 75-year-old Chinese Han man weighting 65 kg came to the Department of Ophthalmology, Beijing Tsinghua Changgung Hospital on March 11, 2016, and complaint of mistiness of vision since February 2016. He received treatment of ethambutol (1500 mg/day) from April 2015 to December 2015 because he suffered from tuberculosis. He did not have any family history of neuropathy.
This study was approved by the Institutional Review Board for the Protection of Human Subjects of Beijing Tsinghua Changgung Hospital and adhered to the tenets of the Declaration of Helsinki. The patient signed an informed consent before the start of examinations.
We performed series of ophthalmic examinations to see the severity of his ocular condition. His BCVA (best-corrected visual acuity) was 0.12 (OS) and 0.15 (OD), whereas the IOP (intraocular pressure) was 10.4 mm Hg and 12.2 mm Hg (Goldmann applanation tonometry, Suzhou City, Jiangsu Province, China), respectively. The slit-lamp microscope examination of bilateral anterior segments indicated no abnormity. The pupils were normal with no relative afferent pupillary defect (RAPD). The funduscopy examination did not indicate any abnormity, either (Fig. 1). Automated perimetry (Humphrey Field Analyzer, Carl Zeiss Meditec, Inc, Dublin, CA, and Octopus Perimeter, Haag-Streit, Mason, OH) indicated typical cecocentral visual field defects (Fig. 2). The retinal nerve fiber layer (RNFL) thickness was measured using optical coherence tomography (OCT) (spectral-domain OCT, Heidelberg Engineering, Heidelberg, Germany). The results showed that the bilateral RNFL thickness was within the normal range (Fig. 3). Furthermore, we took electroretinogram (ERG) examination and found that the amplitude of b-wave was definitely decreased. Based on the ocular examinations listed above, this patient was diagnosed as EON. Since he stopped taking ethambutol in the end of 2015, we just offered some neurotrophic agents to him and asked him to come back for return visit within 1 month.
Figure 1.
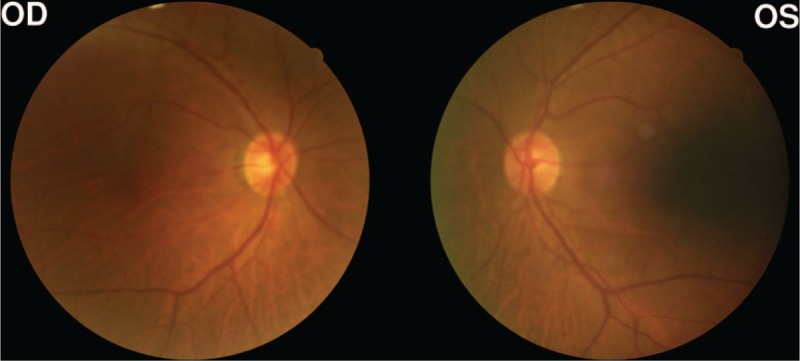
Bilateral fundal photography of the patient at the initial visit. The bilateral funduscopy examination of the patient did not indicate any abnormity at the initial visit on March 11, 2016.
Figure 2.
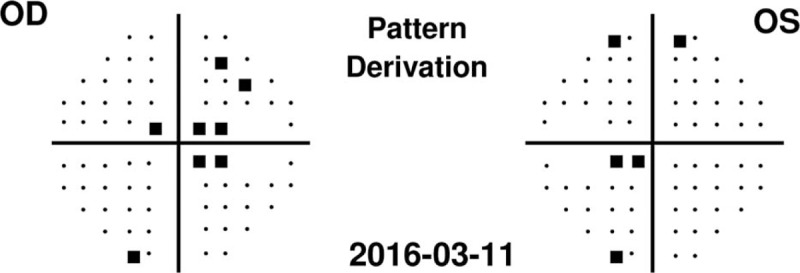
Automated perimetry examination results of the patient at the initial visit. The bilateral automated perimetry by Humphrey Field Analyzer indicated typical cecocentral visual field defects at the initial visit on March 11, 2016.
Figure 3.
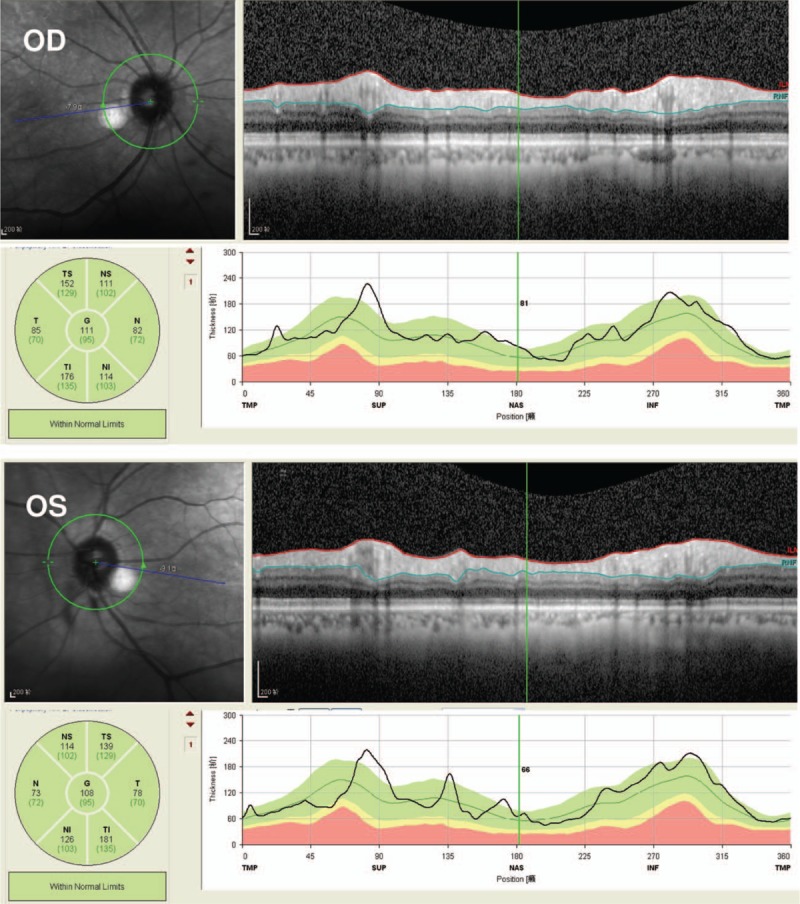
The RNFL thickness measurements at the peripapillary region at the initial visit. The peripapillary RNFL thickness measurements were performed with 360° circle OCT scanning. The results indicated that bilateral RNFL thickness was within the normal range. OCT = optical coherence tomography.
On May 5, 2016, the patient came back to the Department of Ophthalmology, Beijing Tsinghua Changgung Hospital for return visit. This time, his BCVA (best-corrected visual acuity) was 0.8 (OS) and 0.8 (OD), whereas the IOP was 11.9 mm Hg and 11.2 mm Hg (Goldmann applanation tonometry), respectively. The examinations of bilateral anterior segments and fundus also indicated no abnormity. The Goldmann perimetry was performed again to see the outcome of therapies with neurotrophic agents. The results showed completely recovery of cecocentral scotoma (Fig. 4). Thus, the prognosis of the disease in the present case-report was pretty good.
Figure 4.
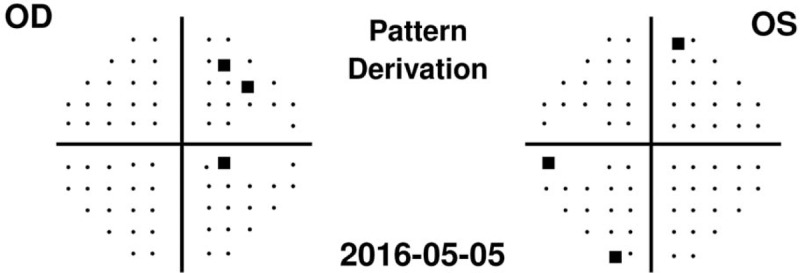
Automated perimetry examination results of the patient at the return visit. The bilateral automated perimetry by Humphrey Field Analyzer indicated complete recovery of cecocentral scotoma at the return visit on May 05, 2016.
3. Discussion
The overall incidence of ethambutol-induced optic neuropathy in tuberculosis cases receiving ethambutol was about 1% that is correlated to the dosage.[8] Among the patients who received ethambutol at dose as low as 12.3 mg/mg/day, some still represented ocular ethambutol toxicity.[9] However, among the patients receiving high dosage of 15 to 25 mg/kg/day of the drug that was close to the case presented above, the reported incidence was up to 5% to 6% when taking for at least 2 months.[10] Therefore, there is no safe dose for ethambutol in the clinical practice. The ocular toxicity should be monitored closely during the therapies and short after the stoppage, especially for the ones that are taking high dosage.
The onset time of EON is not predicable. The ocular symptoms develop from a few days to 2 years after the initiation of drug use.[11] In the present case, the vision impairments occurred short after the patient stopped taking the drug. As to the ocular manifestations, many patients represented bilateral blurred vision, scotomas in the visual field. This patient showed typical cecocentral scotomas, which was common among majority of the patients (Fig. 2). Although the dosage of the drug that the patient took was within high dosage range, neither clinical symptoms nor manifestations were severe. The reason for this phenomenon may be the short period of receiving the drug. In some severe cases, the automated perimetry examination indicated bitemporal hemianopia, which may resulted from involvement of optic chiasm in the development of ethambutol-induced optic neuropathy.[12,13]
As to the RNFL thickness changes, results got from multiple research works were extremely different. Chai and Foroozan detected the RNFL thickness changes after the patients stopped taking ethambutol. The follow-up comparison was performed within 12 months. The results indicated that the RNFL thickness was definitely decreased by comparing with the initial RNFL thickness.[14] In another longitudinal study performed by Han et al, [15] the RNFL thickness was within normal range after the patients stopped taking the drug. In a recent study, Kim and Park[16] reported the thickening of RNFL thickness among the tuberculosis patients with administration of ethambutol at the dosage range of 15 to 19 mg/kg/day.
It is still controversial that whether EON is reversible or not. Early studies indicated some of the ethambutol-induced vision impairments were irreversible,[5,17] which included visual field defects and contrast sensitivity deterioration.[18] However, much more research works demonstrated reversal of the toxicity induced by ethambutol after 1 month of stoppage of the drug in majority of the patients.[19] The reported recovery rate among the patients who stopped taking the drug for more than 1 month was around 50%.[5,17] For the Chinese Han population, 1 observational study performed in Southern Taiwan reported that the recovery rate was 50% after discontinuation of ethambutol for 6 months.[8] The prognostic factors for EON may be related to patients’ age. Tsai and Lee[5] demonstrated that only 1 out of 5 patients aged >60 year-old got recovered, but 4 out of 5 patients aged < 60 year-old got recovered. Reversibility of the toxicity can be indicated by conventional ophthalmic examinations, including visual acuity, color vision, and visual field.
There are some limitations in the present case-report as follows: (1) only 1 typical EON patient was presented here, because it is a rare optic neuropathy in the ophthalmic clinic. We are not able to reach any convincing conclusions about the clinical features and prognosis of this disease in the Chinese Han population. More subjects should be recruited in the future. (2) The follow-up time (1 month) for the patient was too short. Unfortunately, he has not come back for further examinations since the first return visit on May 05, 2016. (3) More specific ocular examinations such as multifocal electroretinogram (mfERG) and visual evoked potential (VEP) should be performed in the patient at the initial visit and return visit.
Footnotes
Abbreviations: BCVA = best-corrected visual acuity, EON = ethambutol-induced optic neuropathy, ERG = electroretinogram, IOP = intraocular pressure, mfERG = multifocal electroretinogram, OCT = optical coherence tomography, RAPD = relative afferent pupillary defect, RNFL = retinal nerve fiber layer, VEP = visual evoked potential.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Varma D, Anand S, Reddy AR, et al. Tuberculosis: an under-diagnosed aetiological agent in uveitis with an effective treatment. Eye (Lond) 2006;20:1068–73. [DOI] [PubMed] [Google Scholar]
- [2].Chan RY, Kwok AK. Ocular toxicity of ethambutol. Hong Kong Med J 2006;12:56–60. [PubMed] [Google Scholar]
- [3].Carr RE, Henkind P. Ocular manifestations of ethambutol, toxic amblyopia after administration of an experimental antituberculous drug. Arch Ophthalmol 1962;67:566–71. [DOI] [PubMed] [Google Scholar]
- [4].Woung LC, Jou JR, Liaw SL. Visual function in recovered ethambutol optic neuropathy. J Ocul Pharmacol Ther 1995;11:411–9. [DOI] [PubMed] [Google Scholar]
- [5].Tsai RK, Lee YH. Reversibility of ethambutol optic neuropathy. J Ocul Pharmacol Ther 1997;13:473–7. [DOI] [PubMed] [Google Scholar]
- [6].Lim SA. Ethambutol-associated optic neuropathy. Ann Acad Med Singapore 2006;35:274–8. [PubMed] [Google Scholar]
- [7].Lee EJ, Kim SJ, Choung HK, et al. Incidence and clinical features of ethambutol-induced optic neuropathy in Korea. J Neuroophthalmol 2008;28:269–77. [DOI] [PubMed] [Google Scholar]
- [8].Chen SC, Lin MC, Sheu SJ. Incidence and prognostic factor of ethambutol-related optic neuropathy: 10-year experience in southern Taiwan. Kaohsiung J Med Sci 2015;31:358–62. [DOI] [PubMed] [Google Scholar]
- [9].Choi SY, Hwang JM. Optic neuropathy associated with ethambutol in Koreans. Korean J Ophthalmol 1997;11:106–10. [DOI] [PubMed] [Google Scholar]
- [10].Leibold JE. The ocular toxicity of ethambutol and its relation to dose. Ann N Y Acad Sci 1966;135:904–9. [DOI] [PubMed] [Google Scholar]
- [11].Chatterjee VK, Buchanan DR, Friedmann AI, et al. Ocular toxicity following ethambutol in standard dosage. British J Dis Chest 1986;80:288–91. [DOI] [PubMed] [Google Scholar]
- [12].Kho RC, Al-Obailan M, Arnold AC. Bitemporal visual field defects in ethambutol-induced optic neuropathy. J Neuroophthalmol 2011;31:121–6. [DOI] [PubMed] [Google Scholar]
- [13].Osaguona VB, Sharpe JA, Awaji SA, et al. Optic chiasm involvement on MRI with ethambutol-induced bitemporal hemianopia. J Neuroophthalmol 2014;34:155–8. [DOI] [PubMed] [Google Scholar]
- [14].Chai SJ, Foroozan R. Decreased retinal nerve fibre layer thickness detected by optical coherence tomography in patients with ethambutol-induced optic neuropathy. Brit J Ophthalmol 2007;91:895–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Han J, Byun MK, Lee J, et al. Longitudinal analysis of retinal nerve fiber layer and ganglion cell-inner plexiform layer thickness in ethambutol-induced optic neuropathy. Graefe's Arch Clin Exp Ophthalmol 2015;253:2293–9. [DOI] [PubMed] [Google Scholar]
- [16].Kim KL, Park SP. Visual function test for early detection of ethambutol induced ocular toxicity at the subclinical level. Cutan Ocul Toxicol 2016;35:228–32. [DOI] [PubMed] [Google Scholar]
- [17].Kumar A, Sandramouli S, Verma L, et al. Ocular ethambutol toxicity: is it reversible? J Clin Neuroophthalmol 1993;13:15–7. [PubMed] [Google Scholar]
- [18].Goyal JL, De S, Singh NP, et al. Evaluation of visual functions in patients on ethambutol therapy for tuberculosis: a prospective study. J Commun Dis 2003;35:230–43. [PubMed] [Google Scholar]
- [19].Menon V, Jain D, Saxena R, et al. Prospective evaluation of visual function for early detection of ethambutol toxicity. Brit J Ophthalmol 2009;93:1251–4. [DOI] [PubMed] [Google Scholar]


