Abstract
Background and Objectives:
Benign duodenal neoplasm is a rare occurrence. Minimally invasive tumor resection and anastomosis formation with an OrVil catheter is a novel approach to treating this disease. In this article, we present a new technique for duodenojejunal anastomosis. This technique was applied in 4 patients with benign distal duodenal tumors who were treated with minimally invasive surgery with robotic assistance.
Methods:
In 4 patients, after the removal of distal duodenal masses with a robotic technique, an orifice in the duodenum was opened to allow for the passage of a guidewire. The guidewire was removed from the orifice by holding it with forceps during an upper endoscopy. An OrVil catheter was sutured to the guidewire outside to allow 2 catheters to proceed consecutively. After the removal of the anvil, an end-lateral duodenojejunostomy was performed with a circular stapler.
Results:
The patients included 3 men and 1 woman (average age, 56). The durations of the operations were 215, 175, 180, and 185 minutes. No complications were observed in any of the patients during the postoperative period. The patients began oral intake on the fifth day of the postoperative period, and they were discharged on the sixth postoperative day. Histopathologic analyses indicated that the removed tumors were adenomas in 2 patients and gastrointestinal stromal tumors (GISTs) in 2 patients. Clear surgical margins were observed in all of the patients.
Conclusion:
The placement of an OrVil catheter for anastomosis in benign neoplasms with distal duodenum localization and the subsequent achievement of duodenojejunal anastomosis with a circular stapler constitute a novel treatment approach.
Keywords: Duodenojejunal anastomosis, Duodenal neoplasms, Robotic resection, OrVil catheter
INTRODUCTION
Primary duodenal neoplasms are not common, accounting for only 2% of all gastrointestinal system (GIS) tumors that localize to the duodenum.1 Most of these neoplasms are malignant and originate in the periampullary region. Benign duodenal neoplasms are rare. The most commonly observed types of benign duodenal neoplasms are adenomas, followed by gastrointestinal stromal tumors (GISTs) and angiomas.2,3 The symptoms of patients with benign duodenal neoplasms are not specific, and the disease may present with a mass, bleeding, and abdominal pain. Tumor removal via an endoscopic approach is an ideal treatment in selected cases.4
Although laparoscopic techniques have been used in practice around the world during the prior 20 years, a limited number of reports have described laparoscopic resection for benign duodenal tumors.5,6 Technical insufficiencies of laparoscopic methods related to their late adoption for resection and reconstruction may be why laparoscopic resection of duodenal tumor is rarely performed. Currently, robotic surgery, which represents the most advanced technological level for minimally invasive surgery, is the most promising method in numerous fields involving the GIS because of 3-dimensional capability and increased range of motion for instruments when compared with standard laparoscopy.7
A small number of benign tumors localize to the D3–D4 portion of the duodenum.1,3 However, in this region, there are difficulties associated with laparoscopic anastomosis after the resection of distally localized duodenal tumors. Robotic surgery may improve technical ability to perform hand-sewn anastomosis, but limitations include the time associated with these. Recently, OrVil (Covidien, Mansfield, Massachusetts, USA) has been used for anastomoses between the reconstructed intestine and either the esophagus or the stomach.8 The combined use of a stapler anvil placed in an orifice and a stapler placed through the jejunum enables these anastomoses to be securely performed within a short time. There are currently no published reports addressing the use of OrVil for duodenojejunal anastomoses. Reasons for this phenomenon may include the difficulty of advancing the OrVil catheter to the anastomosis site and technical insufficiencies relating to its removal from the region proximal to the anastomosis site. In this article, we present a new technique that we used for anastomoses in 4 patients with D3–D4 benign duodenal neoplasms that were resected with robotic surgery.
METHODS
Four patients with benign neoplasms localized to the D3–D4 portion of the duodenum were included in this study. Endoscopy, endosonography (EUS), and dynamic tomography were performed on each of the patients after a routine physical examination, and biochemical assessments were conducted during the preoperative period. Robotic operations were performed in all patients using the da Vinci SI Surgical System (Intuitive Surgical, Inc., Sunnyvale, California, USA). A gastroenterologist (ID) was provided with information regarding the endoscopic processes that would be performed during the operation, the endoscopic device and the additional equipment that was placed in the operating room.
Surgical Procedure
After pneumoperitoneum was achieved by CO2 insufflation, the 12-mm port for the robotic camera was located 1 cm below the umbilicus. Four additional trocars (three 8-mm reusable ports for the robotic instruments and one 12-mm port for the assistant) were inserted into the abdomen. Docking was performed with the patient supine in a 30° reverse Trendelenburg position. The primary gastrocolic ligament was opened, and the duodenum was revealed. Complete mobilization of the duodenum was achieved, and a Kocher maneuver was performed. The mass in the distal duodenum was revealed (Figure 1). Additional dissection was conducted distally along the ligament of Treitz, and the proximal jejunum was exposed. The jejunum was then dissected and divided with a 60-mm blue cartridge Endo-GIA stapler (Covidien) located at least 2 cm distal to the mass. The duodenum dissected from the pancreas was then divided at least 1 cm proximal to the mass with the Endo-GIA stapler (Covidien). Complete resection of the tumor with adequate surgical margins was performed (Figure 2). The specimen was placed into an endobag and removed from the abdomen. We created a small opening in the duodenum that was used to advance the endoscopic catheter from outside the abdomen into the duodenum (Figure 3). The catheter was endoscopically grasped with foreign-body forceps in the duodenum and removed by way of the mouth. After the endoscopic catheter and the OrVil catheter were attached to each other with two 2-0 silk sutures, the end of the endoscopic catheter outside the abdomen was pulled, and both catheters were advanced into the upper GIS in a controlled manner. The OrVil catheter was passed through the pylorus of the stomach using endoscopy, with a Buscopan ampoule applied immediately before this passage. The endoscopic catheter and the OrVil catheter were removed from the opening in the duodenum (Figure 4). The anvil was removed after the polyester thread holding it was cut. Subsequently, a 25-mm long circular stapler (Covidien) was placed in the jejunum, and end-to-lateral duodenojejunal anastomosis was performed (Figure 5). The section of the jejunum into which the circular stapler had been inserted was transected with the Endo-GIA device (Covidien) (Figure 6). After the ligament of Treitz was re-formed, the operation was terminated by placing a silicone drain into the anastomosis region.
Figure 1.
Intraoperative view of the tumor. A cylinder-like projection toward the abdomen from the duodenal wall.
Figure 2.
Transection of the duodenum and jejunum with a linear stapler and complete resection of the tumor.
Figure 3.
Moving the catheter into the duodenum.
Figure 4.
Removing the catheters from the duodenum: endoscopic catheter first and then the OrVil catheter.
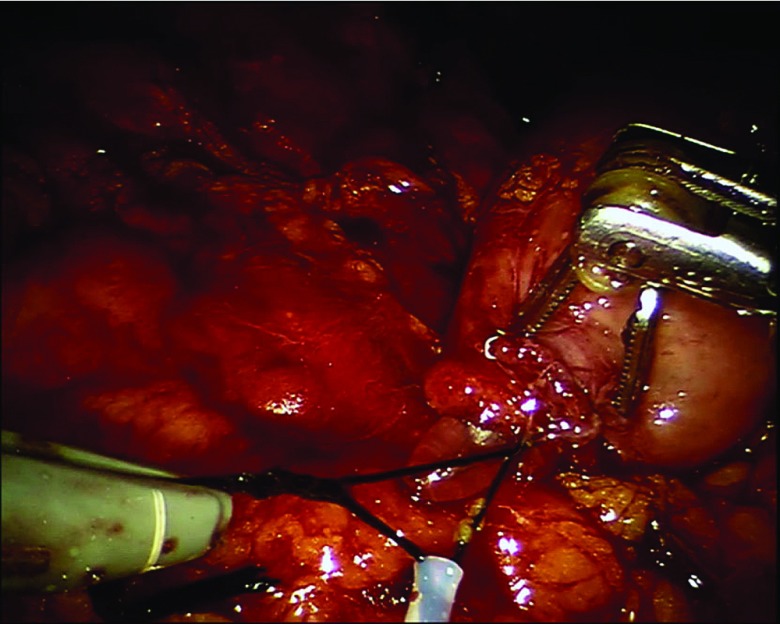
Figure 5.
End-to-lateral duodenojejunal anastomosis formed with a 25-mm circular stapler.
Figure 6.
Circular stapler inserted into the jejunal segment and transected with a linear stapler.
RESULTS
The patients were 3 men and 1 woman (average age, 56 years). The durations of the operations were 215, 175, 180, and 185 minutes, and the average docking duration was 17 minutes. No complications were observed in any of the patients during the postoperative period. Oral intake by the patients was begun after passage X-rays had been performed on the second of the postoperative period. All of the patients were discharged on the sixth day of the postoperative period (Table 1). The histopathological diagnoses were adenoma for 2 patients and GIST for 2 patients. Clear surgical margins were observed in all of the patients. Tumor sizes were 3 and 4 cm, mitotic rates were 1 and 2, Ki-67 indexes were 1 and 4. One of the patients had adjuvant therapy. Tumor sizes were 1.5 and 2.2 cm. Both tumors had low-grade dysplasia.
Table 1.
Patients' Characteristics
| Age | Sex | Localization | Surgery/Setup Times (min) | Length of Stay (d) | Histology |
|---|---|---|---|---|---|
| 52 | Male | D4 | 215/22 | 6 | GIST |
| 58 | Male | D3 | 175/18 | 6 | Adenoma |
| 43 | Female | D4 | 180/15 | 6 | Adenoma |
| 67 | Male | D4 | 185/14 | 6 | GIST |
DISCUSSION
Current treatment strategies for benign tumors in the duodenum include endoscopic mucosal resection, endoscopic submucosal dissection, and papillectomy.4,9 Open surgery is used in cases involving large lesions for which endoscopic methods are insufficient and in cases involving unsuccessful endoscopic interventions. However, high complication rates have been reported for certain techniques (duodenal sleeve resection, segmental resection, transduodenal ampullary resection, and radical pancreaticoduodenectomy) used in open surgeries.10 The unreliability and insufficiency of endoscopic treatments and the high complication rates in open surgery for benign tumor present difficulties in the treatment of benign duodenal tumor. Endoscopic treatment of a benign duodenal lesion is associated with difficulty in obtaining an R0 specimen, and it represents an alternative for small lesions and in patients who have high surgical risk.11
Laparoscopic surgery is infrequently used to treat benign duodenal tumor.5 Encouraging clinical results related to the surgical treatment of these tumors by robotic methods have recently been reported.7 The most important aspect of these surgeries is the anastomosis stage, which occurs after benign duodenal tumors have been removed by laparoscopic or robotic methods. Although robotic methods provide an advantage relative to laparoscopic methods with respect to the use of sutures for double-layer anastomosis of the duodenal region, anastomosis is a time-consuming procedure. Anastomosis performed at the end of an operation may be difficult for surgical teams. Thus, relative to the suture-based anastomosis, an anastomosis performed with the assistance of a stapler is preferred in the upper GIS, because stapler use shortens anesthesia duration and more effectively secures the anastomosis.12 The handsewn method led to a longer operation in 3 of 4 studies, but only 1 of the times showed a statistically significant difference.13–15
OrVil is a system designed for performing circular anastomoses in upper GIS surgeries using minimally invasive methods. After the removal of an OrVil catheter that has been advanced through an orifice from either the esophagus or stomach, anastomoses can be performed quickly and safely with assistance from a long circular stapler placed into the jejunal loop.8 One difficulty of duodenal anastomosis is determining how the OrVil catheter will be passed through the pylorus; even if this passage is successfully accomplished, other challenges include successfully advancing the catheter to its destination, particularly in cases of tumors localized to the distal duodenum, and determining how the anvil will be removed from the region proximal to the anastomosis site. In this study, we have presented a novel endoscopically assisted technique that involves placing OrVil catheters for use in anastomoses in 4 patients with benign distal duodenal tumors treated with robotic surgery. An endoscopic catheter is placed in an ascending manner from an orifice opening through the duodenum; with the assistance of endoscopic foreign-body forceps in the duodenum, this catheter is removed by way of the mouth and is fixed to the OrVil catheter. The circular stapler's anvil is advanced to the proximal anastomosis site by pulling on the end of the catheter that is located outside of the abdomen. In our series of 4 patients, we attempted to advance the OrVil catheter to the appropriate site in a traditional manner in the first patient. Although the passage of the OrVil catheter through the pylorus was accomplished with endoscopic forceps, we were unable to advance the catheter to further segments of the duodenum. Therefore, we were successful with the method we have described. We did not try traditional methods of catheter advancement in any of the other patients, but instead chose to apply the approach described herein. We believe that one reason for the increased operation duration for the first patient was the time required for placing the OrVil catheter using the traditional approach.
When using the traditional approach, large incisions can sometimes be necessary for the removal of the OrVil device16; additional sutures may be needed to close these incisions after the OrVil device is removed. In this case, the opening of an incision narrower than the OrVil device for the catheter achieves the appearance of complete coverage of the orifice by the OrVil catheter's outflow; thus, no additional sutures are necessary. Therefore, although we lack experience with other types of anastomoses, our method may provide advantages for anastomoses in the upper esophagus and stomach regions, which are frequently performed using OrVil.
In conclusion, circular stapler anastomosis was successfully performed in distal duodenal tumors through the placement of an endoscopy-assisted OrVil catheter by using the method described herein. Further studies are needed to determine whether this method provides advantages for other upper GIS anastomoses in which the OrVil catheter is extensively used.
Contributor Information
Abdulkadir Bedirli, Department of General Surgery.
Bulent Salman, Department of General Surgery.
Mahir Nasirov, Department of General Surgery.
Ibrahim Dogan, Department of Gastroenterology, Gazi University Medical Faculty, Ankara, Turkey..
References:
- 1. Zollinger RM., Jr Primary neoplasms of the small intestine. Am J Surg. 1986;151:654–658. [DOI] [PubMed] [Google Scholar]
- 2. Chong KC, Cheah WK, Lenzi JE, Goh PM. Benign duodenal tumors. Hepatogastroenterology. 2000;47:1298–1300. [PubMed] [Google Scholar]
- 3. Bal A, Joshi K, Vaiphei K, Wig JD. Primary duodenal neoplasms: a retrospective clinico-pathological analysis. World J Gastroenterol. 2007;13:1108–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Honda W, Ohmiya N, Hirooka Y, et al. Enteroscopic and radiologic diagnoses, treatment, and prognoses of small-bowel tumors. Gastrointest Endosc. 2012;76:344–354. [DOI] [PubMed] [Google Scholar]
- 5. Kokosis G, Ceppa EP, Tyler DS, Pappas TN, Perez A. Laparoscopic duodenectomy for benign nonampullary duodenal neoplasms. Surg Laparosc Endosc Percutan Tech. 2015;25:158–162. [DOI] [PubMed] [Google Scholar]
- 6. Lee JH, Han HS, Kim YW, Min SK, Lee HK. Laparoscopic wedge resection with handsewn closure for gastroduodenal tumors. J Laparoendosc Adv Surg Tech A. 2003;13:349–353. [DOI] [PubMed] [Google Scholar]
- 7. Downs-Canner S, Van der Vliet WJ, Thoolen SJ, et al. Robotic surgery for benign duodenal tumors. J Gastrointest Surg. 2015;19:306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hirahara N, Tanaka T, Yano S, et al. Reconstruction of the gastrointestinal tract by hemi-double stapling method for the esophagus and jejunum using EEA OrVil in laparoscopic total gastrectomy and proximal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:11–15. [DOI] [PubMed] [Google Scholar]
- 9. Jung JH, Choi KD, Ahn JY, et al. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 2013;45:133–135. [DOI] [PubMed] [Google Scholar]
- 10. Yan JQ, Peng CH, Yang WP, et al. Surgical management of benign duodenal tumours. ANZ J Surg. 2010;80:526–530. [DOI] [PubMed] [Google Scholar]
- 11. Gincul R, Ponchon T, Napoleon B. Endoscopic treatment of sporadic small duodenal and ampullary neuroendocrine tumors. Endoscopy. 2016;48:979–986. [DOI] [PubMed] [Google Scholar]
- 12. Knight BC, Rice SJ, Devitt PG, Lord A, Game PA, Thompson SK. Proximal anastomosis using the OrVil circular stapler in major upper gastrointestinal surgery. J Gastrointest Surg. 2014;18:1345–1349. [DOI] [PubMed] [Google Scholar]
- 13. Hirahara N, Tanaka T, Yano S, et al. Reconstruction of the gastrointestinal tract by hemi-double stapling method for the esophagus and jejunum using EEA OrVil in laparoscopic total gastrectomy and proximal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:e11–e15. [DOI] [PubMed] [Google Scholar]
- 14. Nunobe S, Hiki N, Tanimura S, et al. Three-step esophagojejunal anastomosis with atraumatic anvil insertion technique after laparoscopic total gastrectomy. J Gastrointest Surg. 2011;15:1520–1525. [DOI] [PubMed] [Google Scholar]
- 15. Baigrie RJ, et al. Synchronous combined oesophagectomy in the ‘French’ position. Dis Esophagus. 1996;9:226–227. [Google Scholar]
- 16. Bedirli A, Yucel D, Ekim B. Laparoscopic anterior resection: new anastomosis technique in a pig model. JSLS. 2014;18:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]