Abstract
The American Heart Association (AHA) advocates for CPR education as a requirement of secondary school curriculum. Unfortunately, many states have not adopted CPR education. Our aim was to investigate a low-cost, time effective method to educate students on Basic Life Support (BLS), including reeducation. This is a prospective, randomized study. Retention was assessed at 4 months post-initial education. Education was performed by AHA-certified providers during a 45-minute physical education class in a middle school in Florida. This age provides opportunities for reinforcement through high school, with ability for efficient learning. The study included 41 Eighth grade students. Students were randomized into two groups; one group received repeat education 2 months after the first education, the second group did not. All students received BLS education limited to chest compressions and usage of an Automated External Defibrillator. Students had skills and knowledge tests administered pre- and post-education after initial education, and repeated 2 and 4 months later to assess retention. There was a significant increase in CPR skills and knowledge when comparing pre- and post-education results for all time-points (p < 0.001). When assessing reeducation, a significant improvement was noted in total knowledge scores but not during the actual steps of CPR. Our study indicates significant increase in CPR knowledge and skills following a one-time 45-minute session. Reeducation may be useful, but the interval needs further investigation. If schools across the United States invested one 45–60-minute period every school year, this would ensure widespread CPR knowledge with minimal cost and loss of school time.
Keywords: Cardiopulmonary resuscitation, Education, BLS, AED, Middle school
Highlights
-
•
School age children can efficiently learn Basic Life Support in one physical education period.
-
•
Middle school students show good CPR knowledge and skills retention 2 and 4 months post-education,
-
•
Middle school students can effectively learn the use of an Automated External Defibrillator.
-
•
Basic Life Support education can change the attitude of middle school students towards CPR.
-
•
Reeducation may improve CPR knowledge, skills and Automated External Defibrillator use.
1. Introduction
Since Cardiopulmonary Resuscitation (CPR) was first established in 1960, it has been performed by trained bystanders, rescuing many lives in out-of-hospital cardiac arrests (OHCA). Timely bystander CPR increases the likelihood of survival to 2–4 times (Van Hoeywegen et al., 1993). Unfortunately, the current bystander rate of CPR in the United States is thought to be approximately 31% (Nichol et al., 2008, Chan et al., 2014). In countries where educating school children in CPR is mandatory such as in Denmark, lay resuscitation is performed in 41% of cases, and in cases of witnessed bystander, the odds ratio of survival was three times as more (Wissenberg et al., 2013).
Children as young as 10 years of age have the ability to perform chest compression as efficiently as adults (Bohn et al., 2012, American Heart Association, n.d, Cave et al., 2011). We targeted middle school children as this would be an ideal age for the primary introduction for CPR education with opportunities for reinforcement through high school. This age group also would have mental maturity for recognition as well as timely response in a crisis (Kelley et al., 2006, Bohn et al., 2015). Several studies have demonstrated the ability of school students to perform BLS successfully after CPR education (Jones et al., 2007). The American Heart Association (AHA) advocates CPR education as a required element of secondary and high school curricula (Wissenberg et al., 2013). Regrettably, only 25 states explicitly require CPR training as part of their school curriculum by the 2016–2017 school year, with time and cost being the main barriers for implementation (Bohn et al., 2012).
Automated External Defibrillator (AED) usage is essential to improving sudden cardiac arrest outcome (Hallstrom et al., 2004, La Torre et al., 2008), and is a vital part of CPR education (Reder & Quan, 2003). Previous studies have shown successful CPR training in school-aged children (Jones et al., 2007, Connolly et al., 2007), but only few have included AED education as part of their program (Kelley et al., 2006). Over the past few years, the amount of schools and public facilities that have introduced Automated External Defibrillators (AED) has increased. Unfortunately, the incorporation of AED usage in the BLS teaching algorithm at schools continues to be inadequate.
The objective of our study was to investigate the effectiveness and feasibility of a cost effective method to educate 8th grade middle school students on BLS and AED usage during a physical education (PE) class period. We elected to teach hands-only CPR as most causes of out of hospital cardiac arrest are usually cardiac in nature with noted reluctance among older age students to perform rescues breaths due to fear of infections. Hands-only CPR (Hubble et al., 2003) has been noted by the AHA to have similar outcomes as standard CPR (Sayre et al., 2008).
2. Methods
This is a prospective, randomized, interventional study. The study was approved by the University of Florida's Institutional Review Board (IRB) and by the Alachua County IRB prior to initiation. Parental signed informed consent was obtained for all participating students prior to enrollment. Student's assent was also required. We obtained consent from 78% of eligible students. Each student was assigned a subject identification number. No demographic or identifiable information was collected.
2.1. Study design
The study was a prospective interventional study. All middles schools in Alachua County (home to University of Florida), Florida were invited, with one of eight schools electing to participate. We are unclear about the lack of participation but the common critique was a fixed school curriculum in spite of the PE period being used. Inclusion criteria were 8th grade middle school students who were in good enough health to participate in a physical education class. The demographic profile of the county is 69.9% White, 20.3% Black or African American, 5.4% Asian, and 4.4% from two or more races; 8.4% of the population is Hispanic or Latino. We did not collect demographic data as per agreement from the school. The study method is summarized in Fig. 1. Prior to the course, students were asked to complete a questionnaire, a knowledge test and underwent a skills assessment to evaluate baseline performance. The knowledge test included 7 questions tailored at evaluating each student's baseline knowledge of CPR and AED.
Fig. 1.
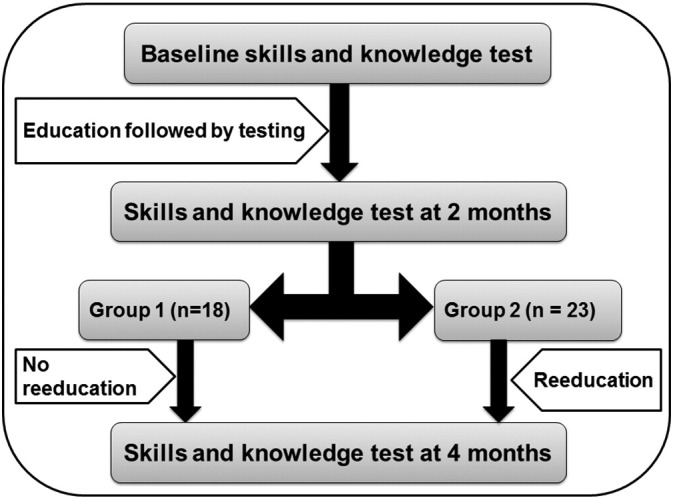
Flowsheet summarizing study design, timeline and randomization.
To test the ability to perform CPR and use of the AED hands, each student was given an out-of-hospital cardiac arrest scenario. Both observers noted for specific actions and received a single score as agreed by both observers. They were then asked to demonstrate their subsequent actions with a manikin placed on the floor mimicking the victim. There were two observers present in the room. The students were then given the following scenario: “Imagine this manikin is a person who collapsed in front of you. You are the only one that knows how to perform CPR. Do whatever you think needs to be done next.” After the student demonstrated what he/she would do in the given situation, the student was sent to a second room and asked to complete the knowledge assessment test.
The CPR training session was completed in one class period. We conducted this class in 5 physical education periods. The session duration was 45 min and was provided by “Gator CPR”, a local CPR education provider group who is AHA approved. Each class consisted of one lecturer. The curriculum consisted of AHA approved Basic Life Support Course with the focus on hands only CPR and use of AED. The session agenda consisted of a lecture, including basic cardiac physiology and signs of cardiac arrest, followed by hands on training on a manikin. There was one instructor per 25 students and 2 students shared one manikin. After the course, students underwent repeat testing of knowledge and skills. The tests were repeated at 2 months and 4 months post-education without prior notification.
After the first BLS education and the testing at 2 months, the students were randomly divided into two groups; group 2 (reeducation group) received a second session of teaching after testing done at 2 months, while group 1 (non-reeducation group) did not. Group one had a normal PE class during reeducation for group 2. At 4 months, all students underwent a final skills and knowledge test to assess for knowledge retention and to assess the effect of re-enforcement. At the end of the study, the students were asked to complete a questionnaire and survey about their BLS education.
2.2. Statistical methods
Statistical analysis was performed using SAS version 9.3. Paired analysis comparing each student's differences in scores for 4 time points (later minus earlier) were performed using two-sided paired t-tests. Group comparisons for the effect of retraining (after potential retraining minus first post test and after potential retraining minus second post-test) were compared by two-sample t-tests with Satterthwaite corrections. A p ≤ 0.05 was considered significant and p > 0.05 but p < 0.1 as marginally significant. These analyses require no distributional assumptions, since prospectively, we expected few outliers, and the sample size (41) was sufficient for the central limit theorem to apply. The primary endpoints were changes in total skills score and total knowledge score.
3. Results
We enrolled 41 8th grade students; 18 students were randomized to the non-reeducation group, and 23 students to the reeducation group. Demographics, including gender, height and weight, were not recorded.
3.1. Initial questionnaire
Prior to CPR education, 63% of the students perceived that learning CPR was difficult. Ninety-five percent of the students knew the meaning of the term CPR and the number to call for an emergency. Only one student had previous BLS training. Only 15% of the students knew what an AED was and of these, none knew its location in school (Table 1).
Table 1.
Initial questionnaire administered at baseline and post-education to assess student's general BLS knowledge.
| Question | Baseline Yes n (%) |
Post-education Yes n (%) |
|---|---|---|
|
1 (2%) | NA |
|
33 (82%) | 31 (79%) |
|
38 (95%) | 40 (100%) |
|
26 (63%) | 5 (12%) |
|
6 (15%) | 38 (95%) |
|
0 | 31 (78%) |
3.2. Knowledge test results
Pre-education knowledge test scores showed that all students had some baseline theoretical CPR knowledge, scoring a median of 4.5/7 (3.7–5) (Table 2). When we compared each student's difference between the pre-education knowledge test total score to the total score for post-education tests at 0, 2 and 4 months, we observed an increase in scores of 1.7 ± 1.2 points, 1.7 ± 1.2 points, and 1.6 ± 1.3 points, respectively (Table 3). All reached statistical difference (p < 0.001). When we compared the difference in scores post testing at 0, 2 and 4 months, the differences in scores were − 0.05 ± 1.11 (p = 0.77), 0.02 ± 1.07 (p = 0.85) and 0.5 ± 1.03 (p = 0.75), respectively. None of the differences in scores post-education achieved statistical significance when assessing all students. The percentage of students selecting the correct answer on the knowledge test during the 4 testing times as well as mean scores are summarized in Table 2.
Table 2.
Knowledge Test scores at different time points.
| Question | Correct Baseline n (%) (mean ± SD) | Correct post-education n (%) (mean ± SD) | Correct 2 months n (%) (mean ± SD) | Correct 4 months n (%) (mean ± SD) Reeducation Group |
Correct 4 months n (%) (mean ± SD) No reeducation Group |
|---|---|---|---|---|---|
| You should use an AED on a person when | 35 (88%) | 41 (100%) | 38 (100%) | 22 (100%) | 17 (100%) |
| 0.88 ± 0.33 | 1 ± 0 | 1 ± 0 | 1 ± 0 | 1 ± 0 | |
| The important qualities when doing CPR include | 25 (63%) | 30 (73%) | 29 (76%) | 17 (77%) | 11 (65%) |
| 0.63 ± 0.48 | 0.73 ± 0.44 | 0.76 ± 0.43 | 0.77 ± 0.42 | 0.65 ± 0.48 | |
| The correct order of operating an AED is | 15 (38%) | 31 (76%) | 21 (55%) | 18 (82%) | 14 (82%) |
| 0.38 ± 0.48 | 0.76 ± 0.43 | 0.55 ± 0.50 | 0.82 ± 039 | 0.82 ± 0.42 | |
| You are doing chest compressions on a man who doesn't wake up and isn't breathing. A friend comes with an AED. What is the next step? | 30 (75%) | 37 (90%) | 36 (95%) | 20 (91%) | 13 (76%) |
| 0.75 ± 0.43 | 0.9 ± 0.3 | 0.95 ± 0.22 | 0.91 ± 0.29 | 0.76 ± 0.42 | |
| The chance of saving the life of a victim of cardiac arrest is best when you | 22 (55%) | 32 (78%) | 30 (79%) | 20 (91%) | 8 (47%) |
| 0.55 ± 0.5 | 0.78 ± 0.41 | 0.79 ± 0.41 | 0.91 ± 0.29 | 0.47 ± 0.50 | |
| What should you do if you tap and shout and the person doesn't respond? | 10 (25%) | 30 (73%) | 32 (84%) | 19 (86%) | 14 (82%) |
| 0.25 ± 0.43 | 0.73 ± 0.44 | 0.84 ± 0.36 | 0.86 ± 0.34 | 0.82 ± 0.38 | |
| You found a friend on the floor who was not breathing. You made sure the area was safe and sent for help and an AED. What should you do next? | 31 (78%) | 39 (95%) | 36 (95%) | 20 (91%) | 17 (100%) |
| 0.78 ± 0.42 | 0.95 ± 0.22 | 0.95 ± 0.22 | 0.91 ± 0.29 | 1 ± 0 | |
| Total score | 4.2 ± 1.2 | 5.8 ± 0.9 | 5.8 ± 0.9 | 6.2 ± 0.7 | 5.5 ± 1.1 |
| Total score median [IQR] | 4.5 [3.7,5] | 6 [5,7] | 6 [5,6] | 6 [6,7] | 6 [5,6] |
Table 3.
Differences in total scores for knowledge and skills tests and use of AED (paired analysis) calculated as later time minus earlier time.
| Time points compared | Score difference | p value |
|---|---|---|
| Knowledge test: | ||
| Pre-test vs Post-test | 1.7 ± 1.2 | < 0. 001 |
| Pre-test vs Post-test at 2 months | 1.7 ± 1.2 | < 0.001 |
| Pre-test vs Post-test at 4 months | 1.6 ± 1.3 | < 0.001 |
| Post-test vs Post-test at 2 months | − 0.05 ± 1.11 | 0.77 |
| Post-test vs Post-test at 4 months | 0.03 ± 1.07 | 0.88 |
| Post-test at 2 months Post-test at 4 months | 0.05 ± 1.03 | 0.75 |
| Skills test: | ||
| Pre-test vs Post-test | 9.3 ± 4.0 | < 0.001 |
| Pre-test vs Post-test at 2 months | 8.6 ± 3.7 | < 0.001 |
| Pre-test vs Post-test at 4 months | 9.4 ± 3.8 | < 0.001 |
| Post-test vs Post-test at 2 months | − 0.7 ± 3.3 | 0.19 |
| Post-test vs Post-test at 4 months | 0.2 ± 3.6 | 0.76 |
| Post-test at 2 months Post-test at 4 months | 0.9 ± 3.7 | 0.14 |
| AED usage: | ||
| Pre-test vs Post-test | 1.4 ± 0.8 | < 0.001 |
| Pre-test vs Post-test at 2 months | 0.8 ± 0.9 | < 0.001 |
| Pre-test vs Post-test at 4 months | 1.3 ± 0.8 | < 0.001 |
| Post-test vs Post-test at 2 months | − 0.6 ± 1.05 | 0.001 |
| Post-test vs Post-test at 4 months | − 0.03 ± 0.92 | 0.99 |
| Post-test at 2 months Post-test at 4 months | 0.6 ± 1.1 | 0.003 |
Bold numbers indicate significance at p < 0.05.
3.3. Skills test
When we compared each student's difference between the pre-education skills test total score to the total score for post-education tests at 0, 2 and 4 months, we observed an increase in scores of 9.4 ± 4.0 points, 8.6 ± 3.7 points, and 9.4 ± 3.8 points, respectively. All reached statistical difference (p < 0.001). When we compared the difference in scores post testing at 0, 2 and 4 months, the difference in scores were − 0.7 ± 3.3, 0.2 ± 3.6 and 0.9 ± 3.7. None of the results achieved statistical significance (Table 3).
During the initial skills test (Table 4), only one student asked for and used the AED correctly. This student was the only one who had been previously taught CPR and AED usage. No one checked area safety, responsiveness or assessed respiration. Twenty-six (65%) students called for 911 and 26 (65%) initiated chest compressions; none within 20 s. Of the 26 students that initiated CPR, 10 (38.5%) had adequate depth and 17 (65%) had adequate compression rate and 15 students (58%) had adequate hand positioning. Several students stopped chest compression after delivering 4–5 compressions.
Table 4.
Skills Test scores at different time points.
| Question | Baseline (mean ± SD) | Post-education (mean ± SD) | 2 months (mean ± SD) | 4 months (mean ± SD) Reeducation Group |
4 months (mean ± SD) No reeducation Group |
|---|---|---|---|---|---|
| Verbalizes scene is safe (2pt) | 0.1 ± 0.44 | 1.71 ± 0.71 | 1.47 ± 0.88 | 1.30 ± 0.93 | 1.76 ± 0.64 |
| Check consciousness (2 pt) | 0.3 ± 0.71 | 1.32 ± 0.87 | 1.47 ± 0.79 | 1.48 ± 0.73 | 1.53 ± 0.78 |
| Check respiration for 5–10s (2pt) | 0.35 ± 0.76 | 1.8 ± 0.59 | 1.37 ± 0.93 | 1.44 ± 0.86 | 1.53 ± 0.85 |
| Calls for help and AED (2pt) | 0.65 ± 0.48 | 1.68 ± 0.56 | 1.26 ± 0.75 | 1.61 ± 0.62 | 1.29 ± 0.75 |
| Starts CPR within 20 s (2pt) | 0.65 ± 0.94 | 0.83 ± 0.99 | 1.42 ± 0.91 | 1.44 ± 0.86 | 1.29 ± 0.96 |
| Correct hand position (2pt) | 0.75 ± 0.97 | 1.76 ± 0.65 | 1.68 ± 0.73 | 1.73 ± 0.64 | 1.41 ± 0.91 |
| Compression depth (2pt) | 0.5 ± 0.87 | 1.85 ± 0.52 | 1.84 ± 0.54 | 1.80 ± 0.56 | 1.76 ± 0.64 |
| Compression rate (2pt) | 0.85 ± 0.99 | 1.12 ± 0.99 | 1.26 + ± 0.96 | 1.58 ± 0.77 | 1.29 ± 0.96 |
| Used AED correctly (2pt) | 0.05 ± 0.31 | 1.41 ± 0.73 | 0.82 ± 0.85 | 1.40 ± 0.67 | 1.41 ± 0.77 |
| Total score Total score median [IQR] |
4.2 ± 2.8 4 [2,6] |
13.5 ± 3.2 14 [12,16] |
12.6 ± 2.8 13 [10,14] |
13.6 ± 2.7 14 [12,16] |
13.3 ± 4.2 13 [12,17] |
| Time to AED shock (sec) Time to AED shock median [IQR] |
215 (only 1) | 116 ± 30 111 [100,134] |
100 ± 19 99 [87,110] |
97 ± 37 88 [80,106] |
88 ± 16 86 [75,106] |
During the immediate post-education skills test, 35 (85%) students checked area safety, 30 (73%) checked responsiveness, 37 (90%) assessed respiration, and 39 (95%) called for help. Thirty-five (85%) students delivered a shock with the AED. Of the 40 students that initiated chest compressions, 17 (42.5%) students started within 20 s, 36 (90%) had adequate hand positioning, 38 (95%) had adequate depth and 23 (57.5%) had adequate rate. The improvement in skills testing was consistently noted during subsequent skills testing.
Median time from test initiation to delivering a shock was 111 (100, 134) seconds after the initial class (Table 2). Interestingly, time to shock decreased at 2 months and 4 months post-education, with a mean of 91 (79, 107) seconds at the 4 month re-evaluation.
3.4. Assessing the effect of re-education on knowledge retention
When comparing total scores for the knowledge test between groups at 0 and 4 months, the reeducation group improved by 0.3 ± 0.9 points and the non-reeducation got worse by − 0.3 ± 1.1 points, which was marginally significant (p value 0.061, Table 5). When comparing total scores for the knowledge test between groups at 2 and 4 months, the reeducated group improved by 0.4 ± 0.9 points and the non-reeducated group got worse by − 0.4 ± 0.9 points, which was of statistical significance (p value 0.0097).
Table 5.
Differences in total scores for knowledge and skills tests per group (later time minus earlier time).
| Time points compared | Score difference No-reeducation Group |
Score difference Reeducation Group |
p value |
|---|---|---|---|
| Knowledge test: | |||
| Post-test vs Post-test at 4 months | − 0.33 ± 1.14 | 0.32 ± 0.96 | 0.061 |
| Post-test at 2 months vs 4 months | − 0.44 ± 0.95 | 0.43 ± 0.93 | 0.0097 |
| Skills test: | |||
| Post-test vs Post-test at 4 months | − 1.06 ± 3.91 | 1.05 ± 3.15 | 0.08 |
| Post-test at 2 months vs 4 months | 0 ± 4.74 | 1.43 ± 2.71 | 0.31 |
On comparing total scores for the skills test between groups at 0 and 4 months, the re-educated improved by one unit and the non-reeducated group got worse by one unit. Also, comparison between sessions at 2 and 4 months between both groups showed that the re-educated group improved by 1.4 units and the non-reeducated group was unchanged. Neither of these data points had statistical significance (Table 5). The correct usage of AED was increased in the re-educated group, with 61% of the retrained students showing correct usage of the AED after retraining vs 50% of the students with no reeducation. The time to deliver a shock with the AED was also smaller for the reeducated group vs the non-reeducated group.
3.5. Post-education questionnaire and survey
At the end of the study, 95% of the students knew what and where the AED was located in the school. None of the students felt that learning CPR was hard and 100% stated that they enjoyed the class. Thirty-one percent of the students had taught a family member or friend about CPR and AED by the end of the first education day (Table 6).
Table 6.
Survey after initial education.
| Question | Yes |
|---|---|
| Did you think the lesson was hard? | 0 |
| Did you have fun during the lesson? | 41 (100%) |
| Did you prefer the lecture over use of manikin? | 39 (95%) |
| Did you teach your friends and family about CPR? | 13 (32%) |
| Would you be interested in becoming BLS certified? | 32 (78%) |
4. Discussion
The critical observation of our study is that a 45 min BLS/AED class taught during a PE period is effective in teaching compressions-only CPR and the use of an AED. There was a marked difference on how middle school students approached a cardiopulmonary arrest situation after education. Furthermore, our study demonstrated that 31% of the students shared the gained knowledge at home (Stroobants et al., 2014). Our study provides evidence to educational institutions around the country that implementing BLS education as part of the school curriculum is feasible. Mandatory BLS education has national importance as, in countries where CPR is a mandatory part of the school curriculum, bystander CPR is performed in > 40% of OCHA and survival rates have doubled or tripled (Wissenberg et al., 2013). The middle school setting is ideal to introduce BLS education as it can reach particular populations where health education is likely to have the most effect. Studies have shown that, although children exposed to BLS training at grades 1–5 are better than counterparts, the most efficient learning and application is noted in children approaching middle school age (Lubranoa et al., 2005, Van Kerschaver et al., 1989). The middle school age also provides the opportunity for repeated training through high school. Furthermore, as noted from our survey, the students enjoyed the class and were eager to share their gained knowledge with friends and family, thus increasing awareness of the importance of CPR education beyond the school setting.
An important aspect of our education program was the inclusion of AED usage. Prior to education, students lacked awareness on AEDs. In a recent survey among American university students, 88% were able to identify an AED from images, but only about a quarter stated they could use an AED without assistance (Bogle et al., 2013). Discussion on AED during our 45 min class was limited to 5–10 min, but it was sufficient to teach the use of an AED, as evident by the fact that 85% of students successfully delivered a shock with the AED in the post-education skills test. Furthermore, knowing the existence and importance of an AED will help create awareness among students of its location in public areas. We did observe that many students forgot the name “AED”, when asking for it. An infrequent, but important point we observed was that some students removed AED pads after shock. Students should be reminded that resuming chest compressions is always a number one priority after shock.
As for the quality of chest compression, most students had adequate hand position and depth at the end of the study. Unfortunately, the rate of compressions continued to be inadequate with 25% of the students not achieving an adequate rate even after education. The fact that students were facing a simulated situation may have contributed to the lack of urgency. The AHA has been working on promoting chest compressions through music with a beat that matches with the “100 beats per minute”, which could have been useful during our class (Roach et al., 2014).
In our study, an AHA certified CPR team was responsible for the education. In previous studies, there has not been a description about the instructional background of the CPR instructors. As the cost of CPR training in schools is mostly attributed to the need of AHA certified instructors, training PE school teachers as certified BLS instructors could easily address the issue. This is a prerequisite in most schools, considering high levels of physical stressors in school athletics. PE teacher education can be accomplished using AHA instructional videos with hands on session with certified AHA programs in the area. BLS training can then be incorporated into the PE curriculum and provided by the PE teacher.
As for re-education, there was a significant increase in the knowledge test scores in the reeducation group. There was an improvement noted in all aspects of the skills test although the difference was not significant. Nonetheless, the p value for the difference in skill test scores from the post-test at 0 vs 4 months was 0.08. Notably, AED usage was improved in the reeducated group. There was also a decrease in time to AED and time to CPR, which could be related to the increased exposure to the CPR process and AED usage through the number of tests conducted. This could have contributed to the lack of a significant difference in the skills testing in the reeducated group.
The interval between retraining is difficult to address in this study as it only spanned 4 months. Kerschaver et al. noted improvement in critical areas of CPR performance with reeducation 6 months apart while Corne et al. showed an improvement in knowledge scores over the same time period (Roach et al., 2014, Van Kerschaver et al., 1989). In a prospective four-year study conducted in Germany, it was noted that yearly repetition was as good as biannual reeducation (Chan et al., 2014). The six-month reeducation curriculums lead to disinterest among the students. Previous studies indicate a clear benefit of annual reeducation. Annual training intervals will likely provide with the best results while assuring proper use of school hours and resources.
There are a number of limitations to our study. The first limitation is the small number of participants in the study due to the difficulties of obtaining both school and parental consent. The knowledge test used in our study was a modified version of the one AHA provides to match the curriculum used in our study and has not been externally validated. Our initial design was to assess retention at 6 months. Unfortunately, due to school curriculum restraints, we were only able to follow up the students in a 4-month span. The frequent knowledge and skills test may have actually helped the students refresh their memory to assist retaining knowledge.
Cities that have implemented training of school children such as Seattle have reached bystander CPR rates up to 50%. In January 2015, the WHO endorsed the “Kids Save Lives- Training school children in Cardiopulmonary Resuscitation Worldwide”, which promotes school based CPR training starting at 12 years of age. We hope further studies will help promote mandated CPR education in school education with reeducation at set time intervals. This will likely increase bystander CPR and AED usage rates.
5. Conclusion
One time BLS/AED education during a 45 min PE class is sufficient in teaching middle school students compressions-only CPR and AED usage with appropriate retention for at least 4 months. Re-education improved the knowledge behind CPR, performance too improved but not significantly. Our approach provides a tool to increase bystander rates in the United States and, thus improve survival after OHCA.
Conflict of interest and source of funding
The authors have no conflict of interest.
Transparency document
Transparency document.
Acknowledgements
This work was partially supported by NIH/NCATS Clinical and Translational Science Award UL1 TR000064. We would like to thank Gator CPR for their support and effort in the completion of this study.
Footnotes
The Transparency document associated with this article can be found, in the online version.
References
- American Heart Association CPR in schools. http://www.heart.org/HEARTORG/CPRAndECC/CommunityCPRandFirstAid/CPRinSchools/CPR-in-Schools_UCM_453682_SubHomePage.jsp (Accessed 15 December 2015, at.
- Bogle B., Mehrotra S., Chiampas G. Assessment of knowledge and attitudes regarding AED. Emerg. Med. J. 2013;30(10):837–841. doi: 10.1136/emermed-2012-201555. [DOI] [PubMed] [Google Scholar]
- Bohn A., Van Aken H.K., Möllhoff T. Teaching resuscitation in schools: annual tuition by trained teachers is effective starting at age 10. Resuscitation. 2012;83(5):619–625. doi: 10.1016/j.resuscitation.2012.01.020. [DOI] [PubMed] [Google Scholar]
- Bohn A., Lukas R., Breckwoldt J. ‘Kids save lives’: why schoolchildren should train in cardiopulmonary resuscitation. Curr. Opin. Crit. Care. 2015;21(3):220–225. doi: 10.1097/MCC.0000000000000204. [DOI] [PubMed] [Google Scholar]
- Cave D.M., Aufderheide T.P., Beeson J. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation. 2011;123:691–706. doi: 10.1161/CIR.0b013e31820b5328. [DOI] [PubMed] [Google Scholar]
- Chan P.S., McNally B., Tang F. CARES Surveillance Group. Recent trends in survival from out of hospital cardiac arrest in the United States. Circulation. 2014;130(21):1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly M., Toner P., Connolly D. The ‘ABC for life’ programme - teaching basic life support in schools. Resuscitation. 2007;72(2):270–279. doi: 10.1016/j.resuscitation.2006.06.031. [DOI] [PubMed] [Google Scholar]
- Hallstrom A.P., Ornato J.P., Weisfeldt M. Public access defibrillation trial investigators. Public access defibrillation and survival after out of hospital cardiac arrest. N. Engl. J. Med. 2004;351(7):637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- Hubble M.W., Bachman M., Price R., Martin N., Huie D. Willingness of high school students to perform cardiopulmonary resuscitation and automated external defibrillation. Prehosp. Emerg. Care. 2003;7(2):219–224. doi: 10.1080/10903120390936815. [DOI] [PubMed] [Google Scholar]
- Jones I., Whitfield R., Colquhoun M. At what age can schoolchildren provide effective chest compressions? An observational study from the Heartstart UK schools training programme. Br. Med. J. 2007;334:1201–1203. doi: 10.1136/bmj.39167.459028.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley J., Richman P.B., Ewy G.A. Eighth grade students become proficient at CPR and use of an AED following a condensed training programme. Resuscitation. 2006;71(2):229–236. doi: 10.1016/j.resuscitation.2006.03.015. [DOI] [PubMed] [Google Scholar]
- La Torre G., de Waure C., Scapigliati A. Cardiopulmonary resuscitation alone vs. cardiopulmonary resuscitation plus automated external defibrillator use by non-healthcare professionals: a meta-analysis on 1583 cases of out-of-hospital cardiac arrest. Resuscitation. 2008;76(2):226–232. doi: 10.1016/j.resuscitation.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Lubranoa R., Romeroa S., Scoppia P. How to become an under 11 rescuer: a practical method to teach first aid to primary schoolchildren. Resuscitation. 2005;64(3):303–307. doi: 10.1016/j.resuscitation.2004.09.004. [DOI] [PubMed] [Google Scholar]
- Nichol G., Thomas E., Callaway C.W. Resuscitation outcomes consortium investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reder S., Quan L. Cardiopulmonary resuscitation training in Washington State public high schools. Resuscitation. 2003;56:283–288. doi: 10.1016/s0300-9572(02)00376-3. [DOI] [PubMed] [Google Scholar]
- Roach J.A., Langdon M.E., DeFalco R. Using music to maintain the correct rhythm during CPR. Nurs. Times. 2014;110(38):12–15. [PubMed] [Google Scholar]
- Sayre M.R., Berg R.A., Cave D.M. American Heart Association Emergency Cardiovascular Care Committee. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest. Circulation. 2008;22(117(16)):2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- Stroobants J., Monsieur K.G., Devriendt B. Schoolchildren as BLS instructors for relatives and friends: impact on attitude towards bystander CPR. Resuscitation. 2014;85(12):1769–1774. doi: 10.1016/j.resuscitation.2014.10.013. [DOI] [PubMed] [Google Scholar]
- Van Hoeywegen R.J., Bossaert L.L., Mullie A. Quality and efficiency of bystander CPR. Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- Van Kerschaver E., Delooz H.H., Moens G.F. The effectiveness of repeated cardiopulmonary resuscitation training in a school population. Resuscitation. 1989;17(3):211–222. doi: 10.1016/0300-9572(89)90037-3. [DOI] [PubMed] [Google Scholar]
- Wissenberg M., Lippert F.K., Folke F. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.


