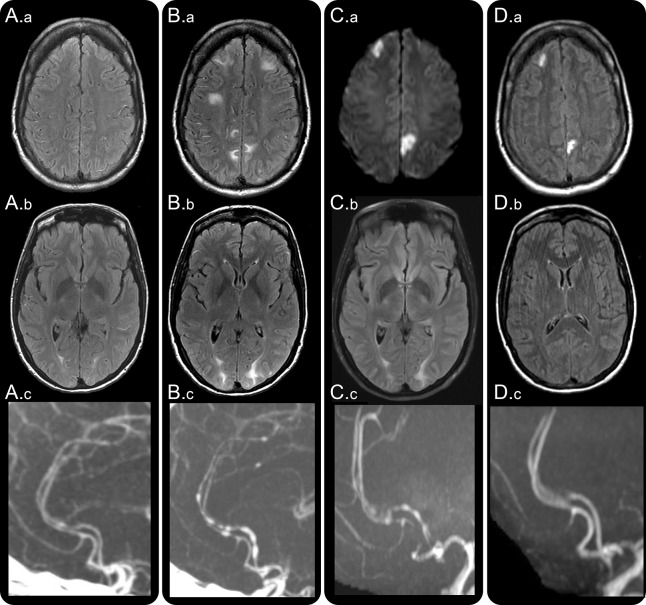
Figure 1. Clinical, radiologic, and angiographic worsening in reversible cerebral vasoconstriction syndrome (RCVS).
A 43-year-old woman with malabsorption syndrome, on parental nutrition, was hospitalized for treatment of port-a-cath infection. On day 2, she developed a thunderclap headache. Head CT and CSF examination were normal. Hydrocortisone 100 mg three times daily was administered for suspected adrenal insufficiency and sepsis. On day 4, brain MRI fluid-attenuated inversion recovery (FLAIR) images showed multiple dot and linear shaped sulcal hyperintensities suggesting dilated cortical surface arteries (A.a) and subtle bilateral white matter vasogenic edematous lesions (A.b) consistent with posterior reversible encephalopathy syndrome (PRES). Headaches recurred, and on day 7 she developed cortical blindness. Head CT angiography (A.c) showed segmental narrowing of multiple intracranial arteries. Brain MRI showed new PRES lesions and progression of prior PRES lesions (B.a, B.b). She was transferred to our hospital. Neurologic examination showed features of the Balint syndrome and aphasia. Repeat CT angiography showed worsening cerebral vasoconstriction (B.c). Hydrocortisone was tapered to 25 mg twice daily; nimodipine and magnesium were administered for suspected RCVS. Repeat MRI on day 9 showed new bilateral ischemic lesions on diffusion-weighted images (C.a), persistent PRES (C.b), and stable cerebral vasoconstriction (C.c). The port-a-cath infection was successfully treated. She was discharged on day 19 on oral prednisone 5 mg daily and nimodipine. Follow-up imaging on day 42 showed established infarctions on FLAIR images (D.a), reversal of PRES lesions (D.b), and resolution of vasoconstriction (D.c). Neurologic examination showed no residual deficits.