Abstract
This study explored using big data, totaling 66 terabytes over 10 years, captured from sensor systems installed in independent living apartments to predict falls from pre-fall changes in residents’ Kinect-recorded gait parameters. Over a period of 3 to 48 months, we analyzed gait parameters continuously collected for residents who actually fell (n = 13) and those who did not fall (n = 10). We analyzed associations between participants’ fall events (n = 69) and pre-fall changes in in-home gait speed and stride length (n = 2,070). Preliminary results indicate that a cumulative change in speed over time is associated with the probability of a fall (p < .0001). The odds of a resident falling within 3 weeks after a cumulative change of 2.54 cm/s is 4.22 times the odds of a resident falling within 3 weeks after no change in in-home gait speed. Results demonstrate using sensors to measure in-home gait parameters associated with the occurrence of future falls.
Keywords: sensors, falls, gait speed, stride length, older adults
The ability of nurses to detect changes in health conditions, functional decline, or increasing fall risk in aging residents who live in the community is a critical part of patient assessment. Historically, these types of assessments have included direct observation, surveys, and interviews to evaluate a resident’s condition change or declining functional status (Rubenstein et al., 2004; Tideiksarr, 2003; Tinetti, 2003). Although many of these assessments used by nurses have been validated and are reliable sources of data for trending status changes in community-dwelling residents, they require a health care provider to be present for the data collection and evaluation. Cutting edge models of care using sensor technology that collects data 24/7 and results in many terabytes of data over several years are being incorporated into residents’ living quarters in elder living communities to facilitate faster decisions about nursing care needed and to make selected living environments safe for older people (Dawadi, Cook, & Schmitter-Edgecombe, 2014; Reeder et al., 2013; Skubic, Alexander, Popescu, Rantz, & Keller, 2009). However, because of their age, frail state, and often times declining health, these residents may require enhanced nursing care coordination. Sensor technology is being used to detect changes in a resident’s condition or an episode of functional decline sooner, enhancing nurses’ ability to react to episodic condition changes, perform a resident assessment more quickly, and possibly suggest treatment options sooner (Rantz et al., 2013). We describe prediction of older adult fall risk using big data sets captured over many years by multiple sensing devices and nurse care coordinators’ use of these data in the care of these adults.
Fall Detection and Activity Monitoring Using Sensor Technology
Falls are the primary cause of injury in older adults, occurring at an annual rate of 33% in persons above the age of 65 years (Centers for Disease Control and Prevention [CDC], 2015a). Early and efficient identification of older adults at risk for falls could prevent costly injuries and loss of quality of life. The extant literature shows that people who walk slower with shorter strides are more likely to fall (Barak, Wagenaar, & Holt, 2006; Quach et al., 2011), but older adults do not receive regular gait evaluations. In an effort to increase fall risk screening efforts, the CDC developed the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) toolkit for health care providers to use in clinical practice (CDC, 2015b). Toolkit materials instruct providers how to conduct specific tests known to predict fall risk, such as the Timed Up and Go, 30-s chair stand, and four-stage balance tests (Guralnik et al., 1994; Jones, Rikli, & Beam, 1999; Podsiadlo & Richardson, 1991). However, providers face time limitations, competing demands, and reimbursement constraints in evaluating and managing fall risk among their patients (Tinetti, Gordon, Sogolow, Lapin, & Bradley, 2006). Moreover, most falls go unreported, further limiting opportunities for providers to assess risk and recommend preventive measures (Shumway-Cook et al., 2009).
One solution to the problem of underreported falls and existing gaps in fall risk screening among older adults is in-home monitoring systems that passively and continuously capture gait parameters from which fall risk can be predicted (Barak et al., 2006). Until recently, human motion analysis using video required the attachment of body markers, as with the Vicon system or the use of multiple cameras, and intensive computations to extract enough silhouettes to fit a skeletal model (Stone & Skubic, 2011). In 2011, the Center for Eldercare and Rehabilitation Technology research team at the University of Missouri (MU) developed a methodology to obtain measurements of temporal and spatial gait parameters from the Microsoft Kinect sensor. Using both a Vicon motion capture system and a web-camera-based system to provide ground truth, researchers validated Kinect-recorded three-dimensional (3D) depth images against standardized gait and balance measures. In addition, fall-detection algorithms were initially developed with stunt actors performing falls in the laboratory and further validated using stunt actors in the apartments of residents of TigerPlace, an independent living community and MU research partner. Following iterative refinement of the fall-detection algorithms, the Kinect fall-detection system has been installed in a total of 39 TigerPlace apartments for continuous automated monitoring of gait parameters for fall risk as well as automated fall detection in the apartments.
As interest in smart home technologies burgeons, other applications of Kinect sensors are being tested (Reeder et al., 2013). Ejupi and colleagues (2016) used the Kinect in a prospective study of fall events in community-dwelling older adults. They demonstrated that upper extremity reaction time was significantly slower for older adults who experienced a fall in the subsequent 6 months compared with those with no fall events. Ejupi et al. envisioned the system could eventually be installed in clinical and home settings for ongoing monitoring of fall risk. In other research, a Kinect sensor was paired with inertial sensors attached to eating utensils for the purpose of tracking movements of interest to therapists (Hondori, Khademi, & Lopes, 2012). In addition, rehabilitation exercise games using the Kinect sensor are under development for use in the home setting (Shapi’i, Bahari, Arshad, Zin, & Mahayuddin, 2015). Although this research demonstrates a variety of clinical uses for the Kinect sensor, our research has advanced smart home technology by real-world operation of the Kinect sensor in older adults’ residences.
Currently, novel sensor systems at TigerPlace use multimodal data sources to collect an array of data 24/7 about residents. Some types of sensor systems are listed and described in Table 1. These data sources extend the ability of TigerPlace’s nurses to detect baseline changes in a resident’s activity levels, without having to be physically present for the assessment. This is a shift from traditional models of assessment. For example, wall-mounted sensor systems help nurses detect when a resident is not as active in their whole apartment, and are spending more time in bed than usual.
Table 1.
Sensor System Modalities and Descriptions.
| Type of sensor | Description |
|---|---|
| Passive infrared (PIR) |
Installed to detect presence in a particular room (e.g., living room, by the door or bathroom) as well as for specific activities. For example, a motion sensor installed on the ceiling above the shower detects showering activity. |
| Bed sensor | The bed sensor is a set of four hydraulic transducers installed under the mattress which captures a ballistocardiogram, respiration, and bed restlessness as someone lies on the bed. Specialized signal processing is used to compute heart rate, respiration rate, and restlessness every 15 s. |
| Depth camera | A depth camera is used to compute gait parameters (gait speed, walks/day, and stride length). The depth camera also uses a fall-detection algorithm to detect falls in real-time and send alerts to designated individuals (e.g., clinical staff) with a link to a depth video (shadow-like silhouette images) showing the fall. |
| Doppler radar | Doppler radar systems have been tested to measure gait parameters and to detect falls. A Doppler radar transmits an electromagnetic wave at a specific frequency and measures the shifts in the reflected waves, like weather radars. These frequency shifts can then be used to obtain the velocities of the person’s body parts in the radar’s direction. |
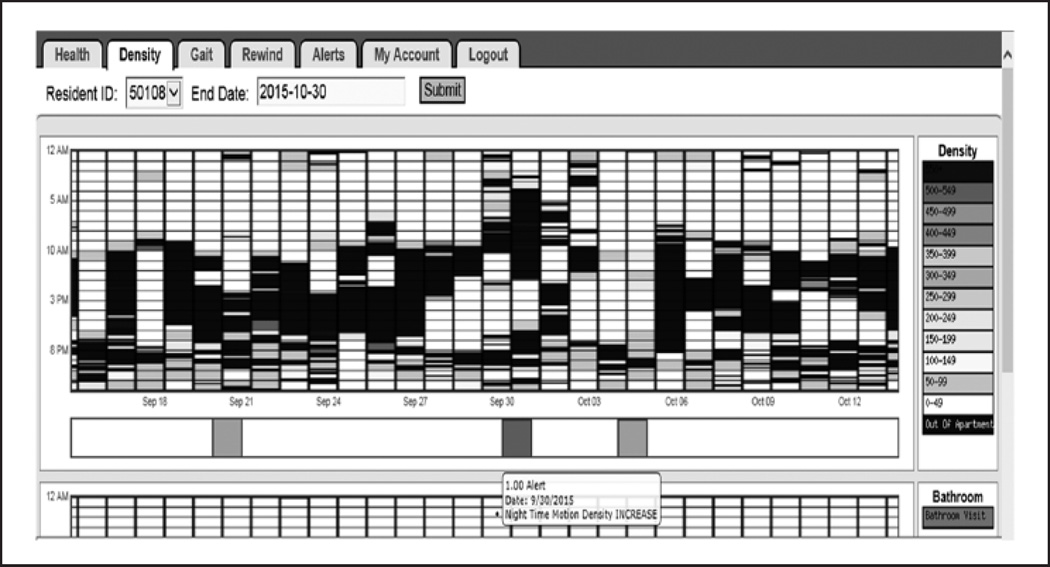
Figure 1 illustrates motion density sensor data visualized through an electronic interface used by nurses to evaluate activity in resident apartments in independent living. This specific illustration also shows that an alert was generated based on a computation using a pre-determined number of standard deviations change from the resident’s normal activity level.
Figure 1.
Motion sensor data density visualization including night-time motion density: Increase alert.
An alert email was also sent to a nurse indicating that the resident was having increased motion in their apartment on September 30, 2015. This increased motion can be seen by the light gray highlighted areas between 2:00 and 6:00 a.m. on September 30, 2015. In addition, the resident appears to be leaving the apartment (black areas between 2:00 and 6:00 a.m. on September 30, 2015) during this same time frame. Based on the patterns observed in this interface, this activity is irregular activity for this person compared with other nights in this density map. This irregular activity is a situation that a nurse may want to review. Case study analyses indicate that increasing periods of inactivity (decreased motion density) could indicate the resident is experiencing higher levels of depression (Galambos, Skubic, Wang, & Rantz, 2013), or it could indicate that the resident is experiencing an illness that is causing greater fatigue and weakness, prompting more rest. Inactivity (black areas) could also mean that the resident has left the apartment at unusual periods of the night or day which may be an indicator of confusion or altered cognitive state.
The sensor system used in this research provides a complex and challenging opportunity to combine different modes of sensor data input that can be triangulated to help nurses detect changes in health conditions and functional decline in frail elders. Not only do sensor system modalities help build a better picture of a resident’s current health status, but with the addition of the Kinect sensors, they provide automated assessment of in-home gait parameters and actual falls. Obtaining gait pattern data provides supplemental information about residents’ health status because research has shown that—down to the 10th of a meter per second—an older person’s pace, along with their age and gender, can predict their life expectancy just as well as the complex battery of other health indicators (Harmon, 2011). Therefore, to investigate whether Kinect sensor data could be used to identify individuals at increased risk of falling, we analyzed the association between pre-fall changes in Kinect-recorded gait parameters and known fall events in TigerPlace residents with Kinect sensors.
Method
Setting
TigerPlace is a senior housing community in Columbia, Missouri, with 54 independent living apartments. Named for the MU mascot, it is an innovative living environment built and operated by Americare Senior Living, in affiliation with the MU Sinclair School of Nursing. Infrastructure is in place to support sensor networks in TigerPlace apartments. TigerPlace provides a unique opportunity in which to develop and evaluate technology in a collaborative setting with researchers from MU departments of Electrical and Computer Engineering, Computer Science, Health Management and Informatics, and Schools of Nursing, Health Professions, Social Work, and Medicine. These researchers form an interdisciplinary team to develop and implement projects that improve the quality of life and care of seniors. No other setting in the United States offers the population of subjects, research infrastructure, faculty, and resources like TigerPlace; research projects are encouraged, and residents who choose to participate enjoy the experience of developing new technologies to help seniors’ age in place. TigerPlace residents, like other seniors in Missouri and the United States, are concerned about maintaining independence and dignity.
TigerPlace is a key component of the Sinclair School of Nursing Aging in Place project that was designed with MU faculty working with Americare Systems, Inc., Sikeston, Missouri, to promote the independence of older adults. Nurses, physical therapists, occupational therapists, and architects with an emphasis in environmental design participated in the building plan. At TigerPlace, residents can age in place without fear of being moved to a traditional nursing home unless they choose to leave. Findings indicate that with the right supportive and restorative services, it is possible to help elders improve their health and well-being and delay or prevent nursing home placement (Rantz et al., 2005). Registered nurse (RN) care coordinators direct the wellness center that offers exercise and other health-related classes, and conduct regular health assessments to promote residents’ well-being and vitality. An electronic health record is used to document day-to-day care. Aging in Place staff provide an array of home care services such as medication management, assistance with activities of daily living, care coordination of health conditions, communication with residents’ physicians and other health care providers, psychosocial services, and Medicare home health care when residents need and qualify for that service.
Sample
Data required for the analysis in the present study were available for a convenience sample of 23 TigerPlace participants with Kinect sensor systems and were collected over intervals ranging from 3 to 48 months, the length of which depended on the duration of participants’ enrollment in the study and length of stay in the community. We excluded participants living with another person because when co-habiting individuals have similar height and gait velocities, their unique clusters of gait data are not discernable in the collective data. All participants were Caucasian and 70% were female. At the time of admission to TigerPlace, participants were, on average, 85.2 years of age, and at the time of data analysis, had a mean length of stay of 49 months. As with TigerPlace research, the institutional review board at MU approved the research and participants provided written informed consent.
Sensor Data Collected
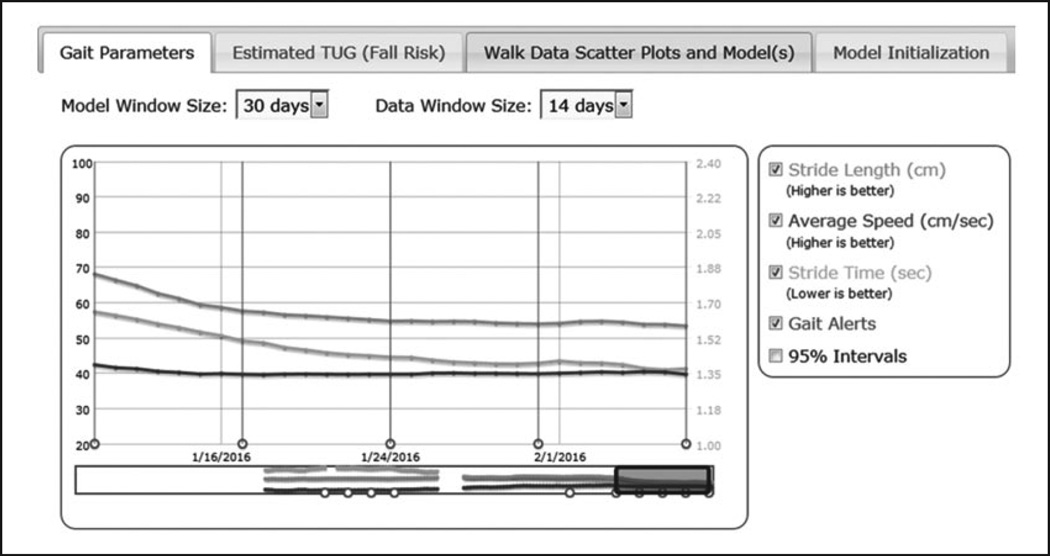
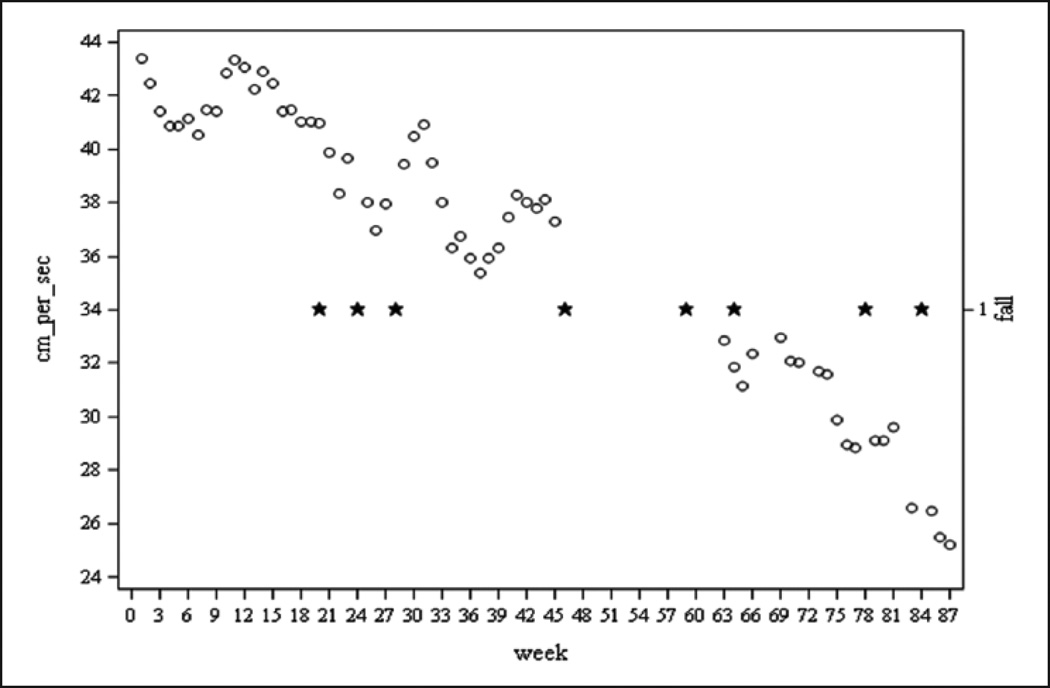
The Kinect sensor continuously monitors and records residents’ in-home movement occurring within sensor range. The Kinect sensor is typically located on a small shelf above the front door to maximize the camera’s view of activity in the main living area. A computer that logs and transmits the Kinect depth image data is located in a nearby kitchen cabinet. Data are processed as depth images that appear as silhouettes to protect privacy. If the Kinect system detected a potential fall, an alert was sent to staff who responded to check on the resident. If the resident was found on the floor in response to a fall alert or the resident self-reported a fall in response to the alert, the fall was recorded in the resident’s health record. In the present study, a fall was defined as an observed or reported unexpected event in which the resident came to rest on the ground or lower surface. In addition, falls that did not generate an alert but that TigerPlace staff observed or falls that were otherwise reported, for example, by residents themselves or family members, were recorded in residents’ health records. After extracting fall event data from health records, we were able to determine the frequency of falls for TigerPlace residents with Kinect system installations and then analyze the association between participants’ fall events and change in in-home gait speed and stride length. Figure 2 provides an illustration of the interface developed to display gait parameter sensor data, longitudinally for 30 days. Figure 3 represents fall events for a participant plotted along weekly gait speed estimates during an 87-week period.
Figure 2.
Gait parameter interface showing calculated stride length and time, gait speed, and alerts.
Note. TUG = Timed Up and Go.
Figure 3.
Weekly gait speed averages with falls plotted on in-home gait speed graph.
Note. ○ = average gait speed; ★ = fall event.
Data Collection
Skeletal tracking with the Kinect Software Development Kit is limited to a range of 1.5 to 4 m, which is insufficient to capture walking sequences in some areas of TigerPlace apartments. Therefore, raw disparity values from the Kinect depth stream, which is a subtraction technique to separate foreground 3D objects (e.g., the person walking) from background stationary objects, such as furniture, are processed to yield walk data for distances of up to 8 m from the Kinect (Stone & Skubic, 2013). Algorithms developed for the Kinect sensor automatically identify, segment and analyze walking segments of at least 1.2 m occurring within sensor range for gait speed, stride time, stride length, and height of the individual walking. The height of each resident was measured a priori so that a cluster, or mode, in the dataset is recognized as belonging to that resident. Modes that closely match the known height of a resident are used for resident model initialization. Typically, a range of 4 to 35 walks per day are required to identify walks belonging to a resident and not another person. Assuming a dataset of walks exists for a resident, the model is updated using data from a given time interval, or model window size, which may be as short as 2 weeks or as long as 3 months. A longer model window size may be required to initialize a model for a resident who walks infrequently. Stride parameters are extracted only for walks for which at least five sequential steps can be identified. Further information on data science methods can be accessed in related papers at the following website: https://www.eldertech.missouri.edu/.
A recent subset of the data (e.g., 1–2 weeks) used in model initialization is used to calculate gait parameters. A 2-week gait parameter window size reflects longer term changes compared with short-term fluctuations that may be represented in a 1-week gait parameter window. Gait parameter estimates for any given day are calculated as a weighted average of gait data from all walks identified in that resident’s apartment within the gait parameter window. A weight is applied to each walk based on the likelihood that it reflects the resident model. The window for both the model estimation and gait parameter estimation slide forward one day and the process of model estimation repeats itself using the previous model estimate for the update procedure. The process of identifying walking segments, extracting gait parameters, updating resident models, and calculating gait parameters was and continues to be completely automated. Data recorded by the sensor systems are continuously logged 24/7 by participant identification number and stored on a secure server, of which Kinect data account for 66 terabytes being used to develop algorithms for gait speed change and fall detection. In totality, sensor network data account for 82 terabytes of storage space.
Depending on the length of time over which gait data are collected, daily gait parameter data may be available in model window sizes of 30, 60, and 90 days and gait parameter window sizes of 7 and 14 days, yielding up to six possible estimates each day for each gait parameter (i.e., gait speed, stride length, stride time). For this study, window sizes of 30 days and 14 days were used for the model and gait parameter estimation steps, respectively. These window sizes were selected so that a sufficient number of walks were included to allow accurate resident modeling but not excluding cases lacking data that would be needed to compute model window sizes of 60 or 90 days.
Data Analysis
Daily gait parameter estimates were available for 23 participants. For those residents that had falls during the study period, we calculated cumulative change in gait parameters from 30 days before a fall. For those residents that had no falls during the study period, we chose a random 30-day window to serve as a control. For a fall to be included in the model, the resident had to have at least 14 days of gait parameter estimates (not necessarily consecutive) or no more than 16 days missing for the entire 30-day window before a fall event. A total of 69 falls met the aforementioned criteria, which resulted in 2,070 observations of gait parameters. We estimated a logistic regression model to predict the odds and the probability of a fall event based on cumulative change in gait parameters at intervals of 7, 14, 21, and 28 days. The outcome was whether a resident had a fall at the end of the 30-day window, and the predictor variable was cumulative change stratified by time (numerical day in the 30-day window). Two separate models were run for cumulative change in in-home gait speed and cumulative change in in-home stride length stratified by time. All analyses were run in SAS 9.4 with a significance level of .05.
Results
Ten of the 23 participants had no falls during the monitoring period, which varied by length of residence from 2011 to 2015. Participants with no fall events were, on average, 85 years of age on admission to TigerPlace and had resided there for an average of 44 months at the time of data collection. Residents who had fallen (n = 13) had between 1 and 12 fall events, were 85.4 years of age, and had resided at TigerPlace for an average of 52 months.
Preliminary results indicate that cumulative change in speed over time is significantly associated with probability of a fall (p < .0001). The odds of a resident falling within 3 weeks after a cumulative decline of 2.54 cm/s over 7 days is 4.22 (95% confidence interval [CI] = [2.14, 8.30]) times the odds of a resident falling within 3 weeks after no change in in-home gait speed. The model estimates that a cumulative decrease of 5.1 cm/s over 7 days in in-home gait speed is associated with an 86.3% probability of falling within the next 3 weeks compared with a 19.5% probability for those with no change. The area under the curve (ROC) is 0.86 indicating that cumulative change in gait speed is good at separating residents that have fallen from non-fallers.
Similarly, preliminary results show that cumulative changes in stride length over time are significantly associated with probability of a fall (p value < .0001). The odds of a resident falling within 3 weeks after a cumulative change of 2.54 cm over 7 days is 6.78 (95% CI = [2.69, 17.07]) times the odds of a resident falling within 3 weeks after no change in in-home stride length. This model estimates that a cumulative decrease of 7.6 cm over 7 days in in-home stride length is associated with a 50.6% probability of falling within the next 3 weeks compared with 11.4% probability for those with no change. The ROC is 0.88 which indicates that cumulative change in stride length is good at separating residents who have fallen from non-fallers.
Discussion
Our results demonstrate the feasibility of using environmentally embedded sensors to measure in-home gait parameters associated with the occurrence of falls. The Kinect sensor system holds promise for unobtrusively monitoring older adults in their homes while maintaining privacy and eliminating the burden of additional monitoring procedures. The Kinect sensor system does not require the older adult to perform gait tests, wear devices, or push a button after a fall. In addition, in-home gait parameters can be measured continuously so that changes over time can be automatically and promptly detected, alerts generated, and appropriate medical or therapy referrals arranged. In response to deterioration in gait speed or stride length, best practice guidelines for screening and assessment and fall prevention interventions could be initiated before a fall occurs and significant injury or disability ensues (Kenny et al., 2011). Residents report feeling more secure in their home environment knowing that the sensors will detect falls and that assistance will be provided when needed (Jacelon & Hanson, 2013; Rantz et al., 2015).
Our model estimated that a 5.1 cm/s (i.e., 0.051 m/s) decrease in in-home gait speed was associated with a high probability of falling within 3 weeks, and this is consistent with published thresholds of 0.05 m/s for a small meaningful change in gait speed assessed over distances of 10 foot, 10 m, or 4 m (Perera, Mody, Woodman, & Studenski, 2006). Similarly, Kwon and colleagues’ (2009) analysis of gait speed change for 424 older adults in a clinical exercise trial showed that a change of 0.03 to 0.05 m/s corresponded to an effect size of 0.2 and a change of 0.08 m/s corresponded to an effect size of 0.5. More importantly, that we can detect similar declines in gait speed by recording and analyzing walking segments as older adults go about their everyday activity means that decline may be detected earlier and clinical interventions initiated sooner than would occur by intermittent clinical evaluation. Benefits of early interventions in the presence of declining walk parameters extend beyond reducing fall risk. Improvement, as opposed to decline, in gait speed of 0.1 m/s over 1 year, has been associated with a 58% reduction in relative risk of mortality over the subsequent 8 years (Hardy, Perera, Roumani, Chandler, & Studenski, 2007).
Another approach to unobtrusive and ongoing gait assessment involves using passive infrared motion sensors (Kaye et al., 2012). Kaye and colleagues (2012) used sensors positioned in a sensor line (e.g., attached to the ceiling of a hallway or corridor) in the homes of 76 community-dwelling older adults to estimate gait speed from the pattern and time intervals of sensor firings and validated these estimates against performance-based mobility tests. Furthering this work, Rana, Austin, Jacobs, Karunanithi, and Kaye (2013) demonstrated that transition time between rooms, measured with infrared sensors positioned throughout the dwelling, not only correlated highly with gait velocity measured along the “sensor line” (R2 = .98) but yielded a greater number and variety of gait velocity estimates. Although infrared sensors offer a compelling alternative to camera-based sensors for measuring in-home gait speed, they lack the fall-detection functionality that our team has developed with Kinect sensors.
The relevance of continuous in-home gait speed analysis is to be able to apply these findings to the ongoing, real-time data and to automatically send alerts about increasing risk of a fall to the older adult, nearby family members, and/or health care staff. With 3 weeks of lead time, the older person could seek assistance to improve their functional capacity or health status and possibly avoid the fall. Having lead time to alert the older person and others has enormous potential to change the loss of functional abilities, trauma, and potentially death that result from falls.
In addition, by identifying the in-home gait speed change threshold at which fall risk is substantially increased, alert algorithms can be further refined for greater specificity. Rather than use the pre-determined standard deviation multiplier developed initially through retrospective analysis and clinician expertise, new alert parameters based on absolute change in gait speed and stride length can be tested alongside the current alert algorithm. Refining alerts for greater specificity is important not only to promptly identify decline in elders’ physical function but also to prevent false alarms that cause clinicians to become alert-fatigued and desensitized to safety alerts (Agency for Healthcare Research and Quality, 2015). Our team is committed to ongoing efforts that advance sensor technology research and optimize clinical relevance to support aging in place for the older adult population.
Our analysis is not without several limitations. One set of limitations is related to generalizability of the findings. Although our sample of fall events included 69 falls, these fall events came from a participant sample of 23 individuals and were restricted to TigerPlace residents. Because TigerPlace residents receive RN care coordination services and may age in place as their health and function decline, it is unclear how representative the sample is of other independent living community residents.
Second, as noted above, not all falls were directly observed or captured by the Kinect sensor. The accuracy of fall history could not be confirmed in some cases. That being said, many studies on fall risk factors and fall incidence rely on self-reports of fall events as most falls go unwitnessed (Barak et al., 2006; Rosen, Mack, & Noonan, 2013; Shumway-Cook et al., 2009). However, “falls” were not explicitly defined within the health record at TigerPlace and thus were subject to clinicians’ interpretation of post-fall circumstances or residents’ self-report.
Third, our analysis was a retrospective analysis of previously recorded sensor data. Use of existing data not only has the advantages of reduced cost and burden but also, in the present study, has the disadvantages of missing data related to sensor system failure and missing data related to inadequate number of walks for resident modeling. It is not possible to know whether residents with too few walks to compute individual models had fall events that were not included in the analysis. Finally, apartments with greater than one resident were excluded from the analysis because resident models could not be computed accurately at the time the data were analyzed.
Future research could involve intervention trials to determine whether fall rates differ for senior housing residents who receive therapeutic interventions based on real-time gait parameter data from Kinect sensors compared with senior housing residents who receive standard of care. Assisted living would be an ideal setting in which to test the Kinect sensor-alert system because 24-hr staff are available to respond to fall alerts and falls are a major problem in this setting, affecting 21% of residents in any 90-day period (Sengupta, Harris-Kojetin, & Caffrey, 2015). In addition, future research to refine the alert algorithms as described above could occur in tandem with a clinical trial or large-scale deployment to yield greater accuracy in algorithmic predictions.
Sensor systems that assist nurse care coordinators to detect functional decline including changes in gait that indicate an increased fall risk and actual falls are sorely needed to facilitate earlier detection, treatment, and prevention of these costly events. Traditional systems of assessment that require nurses to complete unidimensional instruments are risky, because they are not as timely and they typically do not incorporate multiple assessment modalities in a living environment like the sensors described in this study. Another benefit of sensor data collected over months and years on the same residents is the longitudinal nature of this big data that enhances the nurse’s ability to detect changes in baseline over time much more effectively than do traditional assessment methods.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (R01NR014255).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency for Healthcare Research and Quality. Patient safety primer: Alert fatigue. 2015 Retrieved from https://psnet.ahrq.gov/primers/primer/28.
- Barak Y, Wagenaar RC, Holt KG. Gait characteristics of elderly people with a history of falls: A dynamic approach. Physical Therapy. 2006;86:1501–1510. doi: 10.2522/ptj.20050387. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Important facts about falls. 2015a Retrieved from http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html.
- Centers for Disease Control and Prevention. STEADI materials for health care providers. 2015b Retrieved from http://www.cdc.gov/steadi/materials.html.
- Dawadi P, Cook DJ, Schmitter-Edgecombe M. Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct publication. New York, NY: Association for Computing Machinery; 2014. Sep, Smart home-based longitudinal functional assessment; pp. 1217–1224. [Google Scholar]
- Ejupi A, Gschwind YJ, Brodie M, Zagler WL, Lord SR, Delbaere K. Kinect-based choice reaching and stepping reaction time tests for clinical and in-home assessment of fall risk in older people: A prospective study. European Review of Aging and Physical Activity. 2016;13(1):2. doi: 10.1186/s11556-016-0162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galambos C, Skubic M, Wang S, Rantz M. Management of dementia and depression utilizing in-home passive sensor data. Gerontechnology: International Journal on the Fundamental Aspects of Technology to Serve the Ageing Society. 2013;11:457–468. doi: 10.4017/gt.2013.11.3.004.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. Journal of the American Geriatrics Society. 2007;55:1727–1734. doi: 10.1111/j.1532-5415.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- Harmon K. Walking speed predicts life expectancy of older adults. 2011 Retrieved from http://www.scientificamerican.com/article/walking-speed-survival/ [Google Scholar]
- Hondori HM, Khademi M, Lopes CV. Monitoring intake gestures using sensor fusion (Microsoft Kinect and inertial sensors) for smart home tele-rehab setting; 2012 1st Annual IEEE Healthcare Innovation Conference; 2012. Nov, Retrieved from http://www.ics.uci.edu/~mkhademi/files/Publications/HIC2012.pdf. [Google Scholar]
- Jacelon CS, Hanson A. Older adults’ participation in the development of smart environments: An integrated review of the literature. Geriatric Nursing. 2013;34:116–121. doi: 10.1016/j.gerinurse.2012.11.001. [DOI] [PubMed] [Google Scholar]
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport. 1999;70:113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- Kaye J, Mattek N, Dodge H, Buracchio T, Austin D, Hagler S, Hayes T. One walk a year to 1000 within a year: Continuous in-home unobtrusive gait assessment of older adults. Gait & Posture. 2012;35:197–202. doi: 10.1016/j.gaitpost.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny RA, Rubenstein LZ, Tinetti ME, Brewer K, Cameron KA, Capezuti L, Peterson EW. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- Kwon S, Perera S, Pahor M, Katula JA, King AC, Groessl EJ, Studenski SA. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study) The Journal of Nutrition, Health & Aging. 2009;13:538–544. doi: 10.1007/s12603-009-0104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “up & go”: A test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Quach L, Galica AM, Jones RN, Procter-Gray E, Manor B, Hannan MT, Lipsitz LA. The non-linear relationship between gait speed and falls: The MOBILIZE Boston Study. Journal of the American Geriatrics Society. 2011;59:1069–1073. doi: 10.1111/j.1532-5415.2011.03408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana R, Austin D, Jacobs PG, Karunanithi M, Kaye J. Gait velocity estimation using “time interleaved” between consecutive passive IR sensor activations. 2013 Retrieved from http://arxiv.org/pdf/1310.4880.pdf. [Google Scholar]
- Rantz MJ, Dorman-Marek K, Aud M, Johnson RA, Otto D, Porter R. TigerPlace: A new future for older adults. Journal of Nursing Care Quality. 2005;20:1–4. doi: 10.1097/00001786-200501000-00001. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Miller S, Galambos C, Alexander GL, Keller J, Popescu M. Sensor technology to support aging in place. Journal of the American Medical Directors Association. 2013;14:386–391. doi: 10.1016/j.jamda.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Popescu M, Galambos C, Koopman RJ, Alexander GL, Miller SJ. A new paradigm of technology-enabled “vital signs” for early detection of health change for older adults. Gerontology. 2015;61:281–290. doi: 10.1159/000366518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeder B, Meyer E, Lazar A, Chaudhuri S, Thompson HJ, Demiris G. Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: A systematic review. International Journal of Medical Informatics. 2013;82:565–579. doi: 10.1016/j.ijmedinf.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Mack KA, Noonan RK. Slipping and tripping: Fall injuries in adults associated with rugs and carpets. Journal of Injury and Violence Research. 2013;5:61–69. doi: 10.5249/jivr.v5i1.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubenstein LZ, Solomon DH, Rothe CP, Young RT, Shekelle PG, Chang JT, Wenger NS. Detection and management of falls and instability in vulnerable elders by community physicians. American Geriatrics Society. 2004;52:1527–1531. doi: 10.1111/j.1532-5415.2004.52417.x. [DOI] [PubMed] [Google Scholar]
- Sengupta M, Harris-Kojetin LD, Caffrey C. Variation in residential care community resident characteristics, by size of community: United States, 2014 (NCHS data brief, No. 223) Hyattsville, MD: National Center for Health Statistics; 2015. Nov, [PubMed] [Google Scholar]
- Shapi’i A, Bahari NN, Arshad H, Zin NAM, Mahayuddin ZR. 2nd International Conference on Biomedical Engineering (ICoBE), 2015. Piscataway, NJ: Institute of Electrical and Electronics Engineers; 2015. Mar, Rehabilitation exercise game model for post-stroke using Microsoft Kinect camera; pp. 1–6. [Google Scholar]
- Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: Incidence, associated factors, and impact on health care. Physical Therapy. 2009;89:324–332. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skubic M, Alexander GL, Popescu M, Rantz MJ, Keller J. A smart home application to eldercare: Current status and lessons learned. Technology in Health Care. 2009;17:183–201. doi: 10.3233/THC-2009-0551. [DOI] [PubMed] [Google Scholar]
- Stone E, Skubic M. Evaluation of an inexpensive depth camera for in-home gait assessment. Journal of Ambient Intelligence and Smart Environments. 2011;13:349–361. [Google Scholar]
- Stone E, Skubic M. Unobtrusive, continuous, in-home gait measurement using the Microsoft Kinect. IEEE Transactions on Biomedical Engineering. 2013;60:2925–2932. doi: 10.1109/TBME.2013.2266341. [DOI] [PubMed] [Google Scholar]
- Tideiksarr R. Best practice approach to fall prevention in community-living elders. Topics in Geriatric Rehabilitation. 2003;19:199–205. [Google Scholar]
- Tinetti ME. Preventing falls in elderly persons. The New England Journal of Medicine. 2003;348(1):42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Gordon C, Sogolow E, Lapin P, Bradley EH. Fall risk evaluation and management: Challenges in adopting geriatric care practices. The Gerontologist. 2006;46:717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]