Abstract
Chronic kidney disease (CKD) is a serious long-term condition, which if left untreated causes significant cardiovascular sequele. It is well recognized management of modifiable risk factors, such as blood pressure (BP), can lead to improved long-term outcomes. A novel information technology (IT) solution presents a possible solution to help clinicians in the community identify and manage at risk patients more efficiently.
The IMproving Patient care and Awareness of Kidney disease progression Together (IMPAKT) IT tool was used to identify patients with CKD and uncontrolled hypertension in the community. A CKD nurse utilized the tool at primary care practices to identify patients who warranted potential intervention and disseminated this information to clinical staff. Blood pressure management targets and incidence of coded CKD were used to evaluate the project.
Altogether 48 practices participated in an 18 month project from April 2014, and data from 20 practices, with a total adult population of 121,362, was available for analysis. Two full consecutive QI (Quality Improvement) audit cycles were completed. There was an increase in the mean recorded prevalence of coded CKD patients over the course of the project. Similarly, there was an increase in the percentage of patients with BP been recorded and importantly there was an accompanying significant increase in CKD patients achieving BP targets.
At the end of the project an additional 345 individuals with CKD achieved better blood pressure control. This could potentially prevent 9 cardiovascular events in the CKD group, translating to a cost saving of £320,000 for the 20 practices involved. The most significant change in clinical markers occurred during cycle 1 of the audit, the improvement was maintained throughout cycle 2 of the audit. Our results show the real-life clinical impact of a relatively simple and easy to implement QI project, to help improve outcomes in patients with CKD. This was achieved through more efficient working by targeting of high-risk groups, and improved communication between primary/secondary care. The project could be adapted for other chronic disease conditions. Despite the recorded improvements in blood pressure management, a large proportion of high-risk patients remained above ideal blood pressure, additional interventions in this area need to be explored.
Through collaborative and multi-professional working and utilizing IT resources, we have shown it is possible to deliver measurable and sustainable improvements in blood pressure control for patients with CKD in a real life clinical setting.
Problem
Individuals with chronic kidney disease (CKD) may develop end stage renal disease (ESRD) requiring renal replacement therapy (RRT) by dialysis and/or transplantation, and are at higher risk of major cardiovascular events.
Evidence from the UK East Midlands suggests that many CKD patients are undetected, and that those needing secondary care are referred late and thus exposed to worse clinical outcomes.1 2 Separation between secondary and primary care introduces obstacles into the patient pathway which also contribute to poor outcomes.3 The NHS 5 year forward plan has a strong focus on better collaborative working to try and overcome these barriers.4
To improve CKD risk factor management in primary care practices in west Leicestershire, West Leicester Clinical Commissioning Group (WLCCG) primary care clinicians and managers, East Midlands Collaboration for Leadership in Applied Health Research and Care (EM CLARHC) researchers, and nephrologists at University Hospitals of Leicester NHS Trust (UHL) delivered a collaborative quality improvement (QI) project using ‘Improving Patient care and Awareness of Kidney disease progression Together (IMPAKT)’, an innovative CKD-improvement focused software tool.5 IMPAKT was used to deliver 2 full audit cycles of a CKD-focused QI programme; ‘Making an IMPAKT’ in WLCCG. We now report the results of this QI project.
Background
Improving the management of chronic conditions is a global healthcare challenge.6 Chronic kidney disease (CKD) is associated with conditions such as diabetes and hypertension 7. CKD is estimated to contribute around 6,500 excess strokes and 12,000 excess heart attacks annually in England with an associated expenditure of £177 million, in addition to the cost of RRT.8 Patients who progress on to develop ESRD consume 2% of the NHS budget.
Simple management strategies, such as optimising blood pressure (BP) control, can improve long-term outcomes in CKD.9 In the UK, CKD management in primary care is incentivized to some extent through the Quality and Outcomes Framework (QOF), since early detection and treatment can avoid costly downstream medical interventions.10 QOF are a designed to encourage excellence in clinical practice by offering primary care practices that achieve certain targets (eg: measuring blood pressure in patients) financial benefits, these targets are reviewed on an annual basis. However CKD domains do not currently support achievement of the BP targets for diabetic or non-diabetic CKD patients recommended by the National Institute for Health and Care Excellence (NICE).11
Baseline measurement
The objective of the project was to deliver sustainable improvements in the care of patients with CKD. We aimed to improved the accuracy of the primary care CKD register by 5% over a 18 months. The coded prevalence of CKD in patients over the age of 17 for each practice was recorded. Any adult patient meeting CKD criteria based on biochemistry results but not coded for CKD was recorded as ‘uncoded' population. Changes in the coded and uncoded CKD population was analysed.
We aim to achieve a 5% improvement in the number of patient with CKD and diabetes meeting a blood pressure target of 130/80 mmHg for patients with CKD and diabetes, and 140/90 mmHg for patients with CKD and no diabetes as per NICE (National Institute for Health and Care Excellence) guideline over 18 months. All the results were reported using the IMPAKT tool and collected at the start of the project, and than during cycle 1 and 2 of the audit.
Design
IMPAKT was a collaborative development between EM CLAHRC, primary and secondary care clinicians. All general practices in WLCCG were invited to participate. A CKD nurse visited each participating practice to run the IMPAKT software and to support the associated QI project. The role of the CKD nurse included supporting practices to identify and appropriately code patients on practice CKD registers using IMPAKT outputs, and to implement appropriate changes in clinical CKD management focusing on BP control and the correct use of ACEi/ARBs.
Strategy
Currently primary care teams have to manually identify patients with CKD using their own IT solutions, but the number of patients registered are often large and difficult to monitor/update. During the first cycle of the project the aim was to help primary care teams understand how the IMPKAT tool could help improve clinical care, and to improve CKD case ascertainment at each practice. Thereafter patients at high risk of CV events were identified for more focused intervention. High risk patients were defined as those with CKD and BP >150/90 mmHg. This group of patients was of a manageable size, rarely more than 30 patients per practice. During the second cycle of project the focus was on ensuring the CKD register remained up to date, and BP targets in patients who were identified as high risk from cycle 1 were maintained and sustained. Practice nurses were encouraged to engage with the project.
Secondary care clinicians engaged with primary care clinicians at educational sessions to help disseminate key learning objectives on CKD, these education sessions took place during primary care protected teaching events during the 18 months period of the project. A ‘on-call’ nephrologist was also freely available by telephone to advise on management issues when needed. Practice clinical staff were free to determine the most appropriate changes to clinical management in response to IMPAKT.
Altogether 48 WLCCG practices agreed to participate. Of these, 2 practices provided data for the initial baseline data but then took no further part in the project, 10 practices completed one audit cycle of the project with at least 2 visits from the CKD nurse, and 36 practices took completed two 2 audit cycles with the CKD nurse completing at least 3 visits or more to each practice.
Results
Data from 20 participating practices that completed 2 full audit cycles was available for analysis. The first practice visits were in April 2014 and each practice had 3 CKD nurse visits. The combined adult population of these practices during the project was 121,362. The, mean adult practice size during the initial visit was 6068 ± 2676, at the second visit was 6088 ± 2699, and at the third visit was 6222 ± 2819. IMPAKT revealed a total prevalence of coded and uncoded CKD in these practices of 9.48 ± 2.3% at visit 1, 9.43 ± 2.3% at visit 2, and 9.35 ± 2.56% at visit 3. The mean length of time between first and second visits was 178 days, and 407 days between the first and third visit. The mean social deprivation index for the practices taking part was 12.47 (range 6.5-19.3), 8.14% of the study population was >75yrs (range 6.5-11.1%) and 2.67% of the population (range 0-13.6%) was recorded as from an ethic minority. Ethnicity data for 3 practices was unavailable.
An additional 273 patients were coded as CKD on practice registers between the first and second visit, with a significant increase in the coded CKD prevalence between the first (4.79 ± 1.98%) and second (4.98 ± 1.90%) visits (Table 1). However there was no significant difference in the coded CKD prevalence between the second and third visits. IMPAKT identified a significant difference in the percentage of patients with uncoded CKD at the initial visit (4.69 ± 1.60%) and second visit (4.46 ± 1.48%), a difference of 36 patients (Table 1).
Table 1.
Paired difference between mean prevalence of CKD and potential CKD between visit one, two, and three.
| Visit 1 | Visit 2 | Visit 3 | |
|---|---|---|---|
| Prevalence of coded CKD | 4.79%* | 4.98% | 4.89% |
| Prevalence of uncoded CKD | 4.69%* | 4.45% | 4.45% |
* Significant difference in paired difference in CKD prevalence between visit 1 and visit 2 (P<0.05)
There was a significant increase in the mean percentage of CKD patients having their BP recorded in the previous 12 months between the initial visit (91.78 ± 3.56%) and the third visit (93.67 ± 3.43%). There was also a significant increase in the mean percentage of patients achieving BP targets at the third visit (53.93 ± 7.62%) compared to the initial visit (49.43 ± 8.43%), in total an additional 345 CKD patients achieved BP targets at the end of the project (Table 2).
Table 2.
Paired difference between mean percentage of CKD patients with recorded BP check and achieving target BP between visit one, two, and three.
| Visit 1 | Visit 2 | Visit 3 | |
|---|---|---|---|
| Recorded BP check | 91.78% | 91.36%^ | 93.37% |
| Patients with BP at target | 49.43%* | 54.55% | 53.93% |
* Significant difference in paired difference in percentage of patients at BP target between visit 1 and visit 2 (P<0.05)
^ Significant difference in paired difference in percentage of patients with recorded BP check between visit 2 and visit 3 (P<0.05)
There was an increase in the mean percentage of patients with CKD and diabetes achieving BP targets at the third visit (30.00 ± 7.0%) compared to the initial visit (24.46 ± 8.66%) representing an additional 85 patients. Altogether 2343 non-diabetic patients with CKD achieved BP targets initially (59.87 ± 8.90%), and 2603 at the third visit (64.28 ± 7.84%), this difference was significant (Figure 1) (Table 2).
Figure 1.
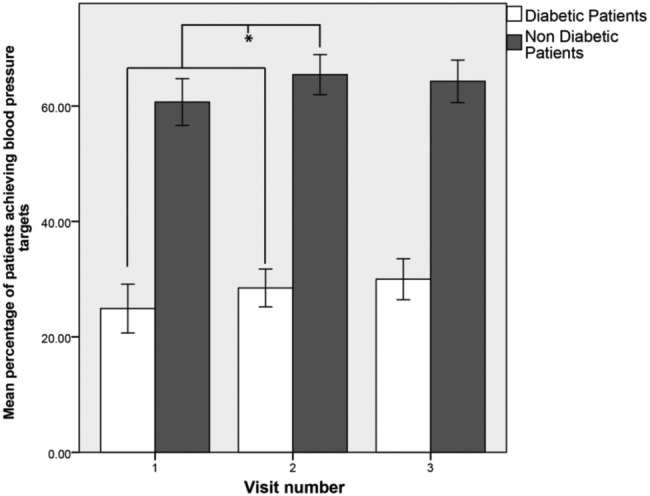
Changes in mean percentage of patients meeting BP targets during the project period, * Significant change in mean percentage of patients meeting BP targets for both diabetic and non-diabetic patients between visit 1 and 2 P<0.05.
Lessons and limitations
Prior to the implementation of this QI project IMPAKT software was freely available to practices, but uptake was low. The CKD nurse was the key component in the success of this project. By facilitating the download and running of IMPAKT on practice IT systems, and aiding in the interpretation of resulting data outputs the CKD nurse delivered essential support to practice teams, thus allowing patient identification and directing management changes.
The biggest changes to the prevalence of coded CKD patients came during the first audit cycle of the project, consistent with the initial focus on ensuring practice CKD disease registers were up to date. We also noted the most significant improvements in blood pressure control occurred early in the project period. However these improvements were maintained for the duration of the project. This was a gratifying finding given the recognised importance of robust BP management in the prevention of CKD related morbidity and mortality.
The overall cost of this project was modest. The IMPAKT software is freely available, and the majority of the project cost represented by the salary cost of a single CKD nurse. No direct financial incentives were provided to participating practices. It is estimated treating 35 CKD patients to BP targets over four years would result in one cardiovascular event prevented.12 The cost to the NHS of managing a stroke, for example, was estimated to be £35,868 in 2008.13 Therefore, given that 345 extra patients reached BP targets during this project, 9 cardiovascular events may have been prevented. If these were all strokes, then a cost saving of circa £320,000 would be achieved. If the findings of the project were replicated in all the practices of WLCCG this saving could be as high as £750,000. In addition, costs associated with treating complications of progressive CKD, such as need for renal replacement therapy and admissions to secondary care would also be mitigated, although were not measured in this project.
The prevalence of CKD changed during the project period, along with a corresponding fall in the number of patients with uncoded CKD. The percentage of patients having a documented BP check also increased from 91.78% to 93.37% indicating changes in clinical practices. Therefore, we are confident the results demonstrate the real life clinical impact of the project. Ten practices did not participate in the second audit cycle of the project for reasons which are unclear. However the majority of practices that started this QI project remained engaged over a period of 18 months. This was not a clinical trial and thus confounding factors such as access to other CKD resources and patient movements between practices were uncontrolled, and there was no matched control group.
The practices taking part in our project served relatively affluent areas. Poverty and deprivation are important factors in health economic outcomes, and this methodology may work less well in other areas with different demographics.14 We are now aiming to expand the project to cover other CCGs with more deprived populations.
The project methodology combined a specialist nurse and innovative informatics solution and effectively improved the parameters of CKD management in general practice. This approach could be tailored to many other chronic diseases in primary care. Improving the management of modifiable risk factors such as BP through accurate identification and targeted intervention in high risk patients will reduce the costs associated with managing complications of chronic conditions such as CKD. Worryingly, for 2015/16 several CKD QOF indicators were retired, and there is currently no QOF incentive to improve BP management in CKD.15 There is a probability that primary care colleagues will now ‘take their eye off the ball’ leading to worse clinical outcomes for patients with CKD, and we highlight this concern.
Other QI methodologies such as ‘Plan, Do, Study, Act’ (PDSA) may have been helpful in our project. Given more time and resource we would have liked to trial specific parts of the project in different primary care setups to help understand which elements worked best before disseminating to a larger group. To over come the limitation of not been able to carry out the PDSA methodology, our approach was very much focused on giving primary care teams different tools needed to make improvements in CKD care, but allowing each practice to be flexible in how they implemented those tools.
Overtime we aim to gather additional data points and understand better how to maintain the changes observed so far in the project, and also how changes in national QOF targets may affect the long-term sustainability of the project. If we had the opportunity to start the project again we would have placed more emphasis of the role of the CKD nurse when promoting the project, as we feel this would have helped to engage more practices to take part in the project.
Conclusion
This QI project assessed the feasibility of using disease-focused informatics combined with CKD nurse support in the community, along with better secondary care/primary care working, to improve care for patients with CKD. After 18 months of the project we observed both an increase in coded CKD and an improvement in BP control keeping with NICE CKD guidelines. The biggest improvements were achieved early, but maintained at the end of the project.
Acknowledgments
Deborah Oliver, CKD nurse, Community Nurse, West Leicester Clinical Commissioning Group
Footnotes
Declaration of interests: This project was developed with funding from the East Midlands Collaboration for Leadership in Applied Health Research and Care (CLARHC EM) and from West Leicester Clinical Commissioning Group. We also thank Baxter Healthcare for contributing to the funding of this project.
The research was supported by the NIHR Collaboration for Leadership in Applied Health Research and Care East Midlands (CLAHRC EM).The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Ethical approval: Based on local policy, this work met criteria for operational improvement activities and was therefore exempt from ethics review.
References
- 1.Caskey DA, Dawnay A, Farrington K et al. 16th Annual Report of the Renal Association UK Renal Registry, 2013. [Google Scholar]
- 2.Smart NA, Titus TT. Outcomes of early versus late nephrology referral in chronic kidney disease: a systematic review. Am J Med 2011;124:1073–80. [DOI] [PubMed] [Google Scholar]
- 3.Kvamme OJ, Olesen F, Samuelsson M. Improving the interface between primary and secondary care: a statement from the European Working Party on Quality in Family Practice (EQuiP). Quality in Health Care 2001;10:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.England N. NHS Trust Development Authority Five Year Forward View. In: Public Health England HEE, Monitor, Care Quality Commission, ed., 2014.
- 5.IMPAKT.IMproving Patient care and Awareness of Kidney disease progression Together, 2015. http://www.impakt.org.uk/. [Google Scholar]
- 6.Griffin SJ. The challenge of chronic conditions: WHO responds. Bmj 2000;321:405–12.10938048 [Google Scholar]
- 7.Atkins RC. The epidemiology of chronic kidney disease. Kidney international 2005;67:S14–S18. [DOI] [PubMed] [Google Scholar]
- 8.Kerr M, Bray B, Medcalf J et al. Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association 2012;27:iii73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravera M, Re M, Deferrari L et al. Importance of Blood Pressure Control in Chronic Kidney Disease. Journal of the American Society of Nephrology 2006;17:S98–S103. [DOI] [PubMed] [Google Scholar]
- 10.Public Health England. National General Practice Profiles. Secondary National General Practice Profiles 2015. http://fingertips.phe.org.uk/profile/general-practice. [Google Scholar]
- 11.National Institute for Health and Care Excellence. Chronic kidney disease early identification and management of chronic kidney disease in adults in primary and secondary care. (Clinical Guideline 73) 2015. [PubMed] [Google Scholar]
- 12.Hex N, Bartlett C, Wright D et al. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabetic medicine: a journal of the British Diabetic Association 2012;29:855–62. [DOI] [PubMed] [Google Scholar]
- 13.National Institute for Health and Care Excellence. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). (Clinical Guideline 68) 2008. [Google Scholar]
- 14.Thomson H, Petticrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. Bmj 2001;323:187–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NHSEmployers. Secondary 2015/16 General Medical Services (GMS) contract Quality and Outcomes Framework (QOF), 2014. http://www.nhsemployers.org/your-workforce/primary-care-contacts/general-medical-services/quality-and-outcomes-framework/changes-to-qof-2015-16. [Google Scholar]


