Abstract
Remifentanil is reported to reduce oral tissue blood flow. We performed a retrospective investigation using logistic regression analysis of anesthesia records to investigate whether the use of remifentanil infusion in a balanced anesthesia technique was useful as a primary technique to reduce blood loss during orthognathic surgery. Subjects were 80 patients who underwent Le Fort I osteotomy and sagittal split ramus osteotomy of the mandible. The variables included gender, age, weight, type of maintenance anesthetic, type and dose or infusion rate of opioid, mean systolic blood pressure (SBP-mean), coefficient of variation of systolic blood pressure (CVSBP) during surgery, mean heart rate (HR-mean), duration of surgery, total blood loss, volume of infusion used, amount of local anesthetic used, body temperature, and urine output. Gender, type of maintenance anesthetic, type of opioid, SBP-mean, CVSBP, HR-mean, and duration of surgery were used as candidates for independent variables. Logistic regression analysis was performed for the selected independent variables with the total blood loss as the dependent variable. The factors associated with the reduction of blood loss were the use of remifentanil (odds ratio, 3.112; 95% CI, 1.166–8.307; P = .023) and smaller CVSBP (odds ratio, 2.747; 95% CI, 1.07–7.053; P = .036). Use of remifentanil and smaller CVSBP were associated with a reduction of blood loss during orthognathic surgery.
Key Words: Remifentanil, Blood loss, Orthognathic surgery, General anesthesia, Logistic regression analysis
Major diseases requiring surgical treatment in the oral and maxillofacial region include malignant tumor, jaw deformity, and cleft lip and palate. Because both oral mucosa and bone marrow, which have abundant blood flow, are part of the surgical field, control of bleeding to ensure a clear surgical field is important for the smooth progression of surgery. Reduction of bleeding also helps to limit allogeneic blood transfusions and decrease the need for autologous blood transfusion, potentially enabling swifter postoperative recovery and fewer complications.
For this reason, several studies have investigated anesthesia management techniques to reduce bleeding. One such method is deliberate hypotension, generally defined as a mean arterial pressure less than 60 mm Hg or mean arterial pressure reduction more than 30% of the control value. It has been reported that oral tissue blood flow decreases depending on the mean arterial pressure and cardiac output and that reduction in these parameters reduces the volume of bleeding.1–4 Other studies, however, have reported complications such as brain damage from excessive hypotension5–8 as well as an increase in the incidence of postoperative complications caused by intraoperative hypotension and prolongation of hospital stays.9
In rabbit studies, Kemmochi et al10 reported that remifentanil reduced blood flow in lingual mucosa and mandibular bone marrow tissue without a major decrease in blood pressure. Koshika et al11 reported that remifentanil decreased blood flow in lingual mucosa, mandibular bone marrow tissue, masseter muscle, and maxillary and mandibular alveolar tissue in an infusion rate–dependent manner. However, the effect of the use of remifentanil during oral and maxillofacial surgery on bleeding in clinical practice is as yet not fully clarified.
In this study, we carried out a retrospective investigation using logistic regression analysis of anesthesia records to investigate whether or not the concomitant use of remifentanil was useful in reducing blood loss during orthognathic surgery under general anesthesia, and if it was, to identify whether or not the reason was because it lowered blood pressure.
METHODS
This study was approved by the Tokyo Dental College Ethics Committee (approval No. 464). The requirement for written informed consent was waived by the Tokyo Dental College Ethics Committee. The subjects were 80 patients (21 men, 59 female) who underwent Le Fort I osteotomy and sagittal split ramus osteotomy of the mandible performed by the same surgeon at the Chiba Hospital of Tokyo Dental College between January 2008 and December 2012.
General anesthesia was induced with propofol and fentanyl, and nasotracheal intubation was performed after muscle relaxation with rocuronium bromide or vecuronium bromide. Anesthesia was maintained with air, oxygen, and either 1% propofol using target controlled infusion (TE-371, Terumo Corporation, Tokyo, Japan) at 3–4 μg/mL, which correlates to a state of general anesthesia (commonly equivalent to 6–8 mg/kg/h or 100–133 μg/kg/min propofol infusion), or sevoflurane (1.5%–2.5%), and FIO2 was set to 0.4. Either remifentanil (continuous infusion at 0.05–0.25 μg/kg/min) or fentanyl (repetitive bolus amounts of 0.05 or 0.1 mg) was used as the intraoperative opioid. If fentanyl was used, it was administered at least once per hour or when blood pressure was elevated more than 20% from the baseline value during surgery. In the patients receiving remifentanil, transitional fentanyl was given after the conclusion of surgery and discontinuation of remifentanil. Other hypotensive adjuvants, such as β-blockers or vasodilators, were not used in any case in this study. End-tidal carbon dioxide concentration was maintained during anesthesia at 35–40 mm Hg through controlled mechanical ventilation. Acetate Ringer's solution was administered at approximately 10 mL/kg/h for fluid infusion during surgery, and rectal temperature was continuously monitored. Local anesthesia including infiltration anesthesia and nerve block using 1% lidocaine hydrochloride solution with 10 μg/mL epinephrine was used during surgery.
The parameters investigated included gender, age, weight, type of maintenance anesthetic, type and dose or infusion rate of opioid, mean systolic blood pressure (SBP-mean), coefficient of variation of systolic blood pressure (CVSBP; standard deviation of SBP during surgery divided by SBP-mean), mean heart rate (HR-mean) during surgery, duration of surgery, total blood loss, volume of infusion used, amount of local anesthetic used, body temperature, and urine output. SBP-mean was recorded from direct measurements from noninvasive blood pressure monitoring carried out at 5-minute intervals during surgery. Gender, type of maintenance anesthetic, type of opioid, SBP-mean, CVSBP, HR-mean, and duration of surgery were used as candidates for independent variables.
To carry out logistic regression analysis, cutoff values for the quantitative candidate for independent and dependent variables were determined from the means of each measured value, and the variables were converted to dummy variables in which values exceeding or less than those cutoff values were coded as 0 and 1, respectively. Thus, the sample was divided into 2 groups. Qualitative variables were also converted to dummy variables to divide the sample into 2 groups. To test the independence of each variable, multicollinearity was investigated by performing a chi-square test on each variable to generate a correlation matrix. A chi-square test was used to test the association between each independent variable and total blood loss and items for which P < .10 were selected as independent variables. Logistic regression analysis was then performed for these independent variables with total blood loss as the dependent variable, using the step-up procedure based on the likelihood ratio. A P value less than .05 was regarded as significant. PASW Statistics version 20 (IBM Corporation, Armonk, NY) was used for statistical analysis.
RESULTS
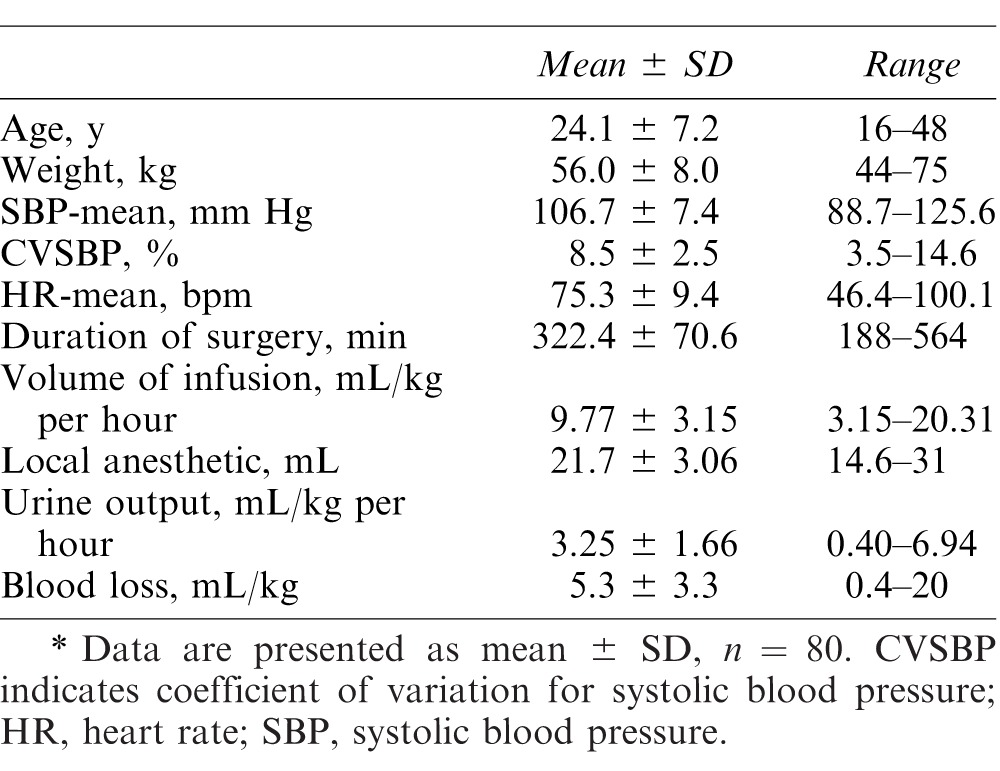
Table 1 shows the mean values of the parameters investigated. Sevoflurane was used for the maintenance anesthesia in 55 cases and propofol in 25, and remifentanil was used in 51 cases and fentanyl in 29; the total doses of remifentanil and fentanyl were 2.49 ± 1.25 mg and 0.895 ± 0.455 mg, respectively. The mean temperature of individual patients during anesthesia ranged from 35.6°C to 38.2°C.
Table 1. .
Mean Values for the Parameters Investigated*
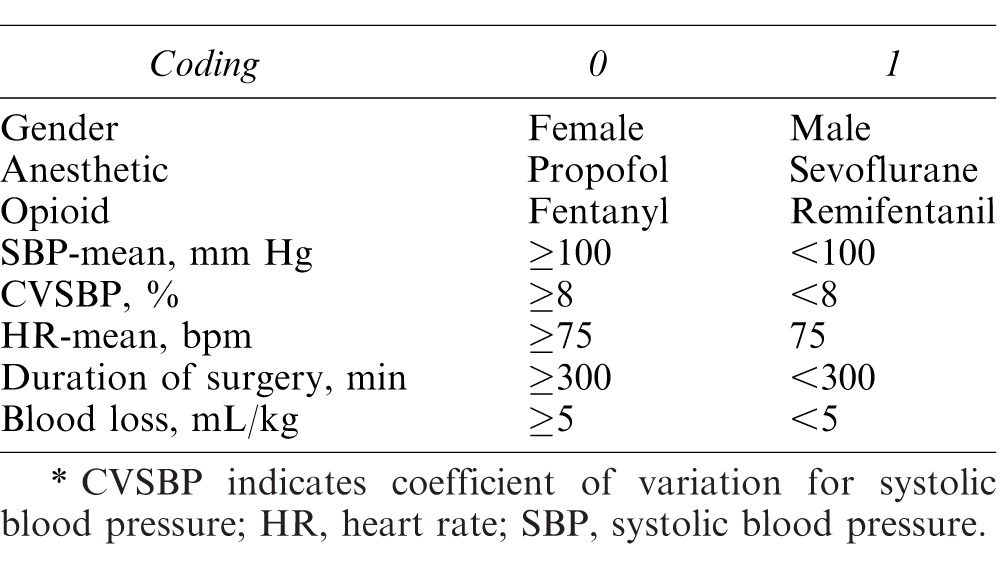
From the mean results, gender, type of maintenance anesthetic, type of opioid, SBP-mean (≥100 mm Hg/<100 mg Hg), CVSBP (≥8%/<8%), HR-mean (≥75bpm/<75bpm), and duration of surgery (≥300 min/<300 min) were used as candidates for independent variables and converted to dummy variables. Total blood loss (≥5 mL/kg/<5 mL/kg) was also converted to a dummy variable as the dependent variable (Table 2).
Table 2. .
List of the Coding for Each Variable
The relevance of each candidate was investigated by means of a correlation matrix (Table 3). The candidate for independent variables associated with the reduction of blood loss at P < .10 were the type of opioid and CVSBP. Multicollinearity was not observed between these 2 variables.
Table 3. .
Relevance of Each Candidate for Independent Variables Shown in Respective P Values*
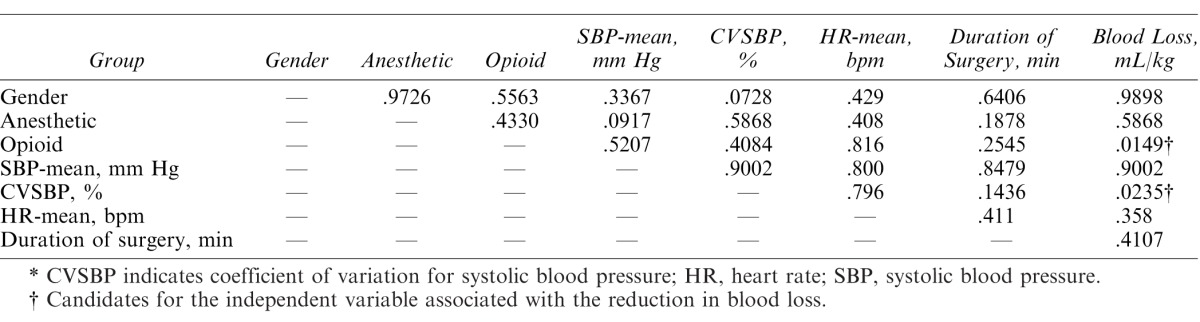
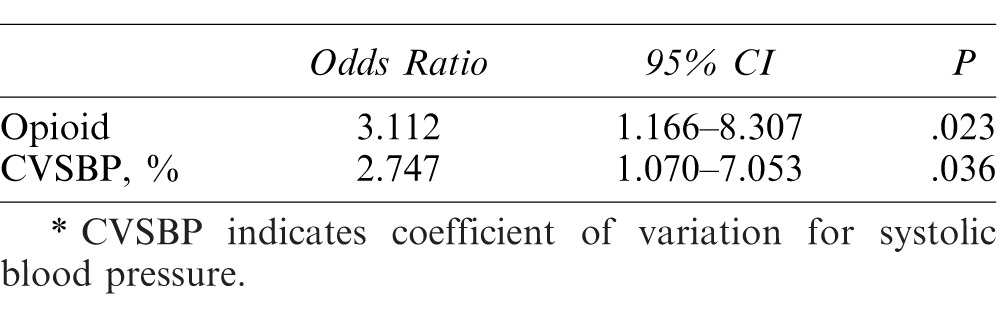
Table 4 shows the results of logistic regression analysis with the type of opioid and CVSBP as independent variables and blood loss as the dependent variable. The odds ratio for remifentanil was 3.112 (95% CI, 1.166–8.307; P = .023) and that for CVSBP was 2.747 (95% CI, 1.07–7.053; P = .036), respectively. The results of a model chi-square test were significant at P < .05, and the Hosmer-Lemeshow test showed satisfactory goodness-of-fit at P = .451, with a discrimination rate of 63.7%.
Table 4. .
Results of Logistic Regression Analysis*
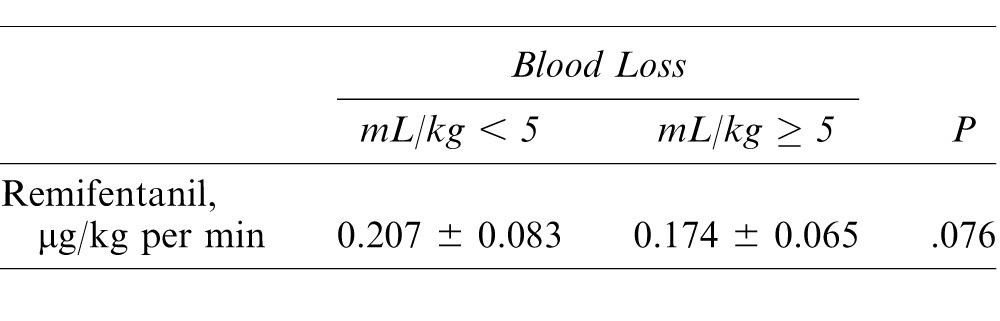
The mean infusion rate of remifentanil in patients with blood loss of <5 mL/kg was 0.207 ± 0.083 μg/kg/min. Although this was slightly higher than the value of 0.174 ± 0.065 μg/kg/min in patients with blood loss of ≥5 mL/kg, the difference was not significant (P = .076; Table 5).
Table 5. .
Mean Infusion Rate of Remifentanil
There were no adverse symptoms such as delayed awakening, respiratory depression, or hypotension that required drug administration caused by remifentanil or fentanyl in any of the cases.
DISCUSSION
This study showed that the factors related to reduction of blood loss were the use of remifentanil and smaller CVSBP, whereas there was no relationship between SBP-mean and blood loss.
Remifentanil is an ultrashort-acting opioid that possesses analgesic effect comparable to that of fentanyl. It suppresses the autonomic nervous response to noxious stimuli and hemodynamic changes during surgery; furthermore, because it is esterase metabolized quickly in plasma, it enables rapid titration and prompt emergence after anesthesia.12–14 This ease of adjustability suggests that remifentanil is useful in oral and maxillofacial surgical procedures.15
Research in rabbits has shown that remifentanil dose-dependently decreases blood flow in the oral tissue.11 There is one study that investigated the blood loss during remifentanil-based anesthesia with sevoflurane and with isoflurane during orthognathic surgery.16 In this comparative study between remifentanil and fentanyl, we indicated that the use of remifentanil was associated with the reduction of blood loss under propofol anesthesia.
A previous study of blood loss when remifentanil or fentanyl was used during spinal surgery under general anesthesia also found that blood loss was significantly less in patients given remifentanil and suggested that this was because remifentanil maintained lower blood pressure.17 In another study, when intraoperative blood pressure was maintained at either normal level or decreased level in patients undergoing Le Fort I osteotomy, blood loss was found to be less in patients maintained in a hypotensive state.18 Maintenance of hypotension has thus been identified as an important factor in reducing blood loss during surgery. In this study, however, although we found a relationship between CVSBP and blood loss, no such relationship was observed with SBP-mean, suggesting that in orthognathic surgery, it may be more important to suppress variations in systolic blood pressure rather than to lower the value of mean systolic blood pressure itself.
The results of this study also showed that the odds ratio for the use of remifentanil was greater than that for the CVSBP. This suggests that the use of remifentanil contributes more importantly to reducing blood loss. The absence of a significant relationship between the type of opioid and CVSBP (P = .4084) suggests that multicollinearity was unlikely and that remifentanil contributes to reducing blood loss via factors other than stabilizing blood pressure fluctuation. Hence, it is possible that remifentanil decreased blood flow in oral tissues and reduced blood loss in humans in a manner similar to that seen in rabbit studies.10,11 Further studies are needed to examine which factor, decreased blood flow in oral tissues due to remifentanil or suppression of variations in systolic blood pressure, contributes more to the reduction in blood loss and to what degree.
In this study, we also found that blood loss tended to be decreased for a greater mean infusion rate of remifentanil, although this difference only approached significance (P < .076). A greater number of subjects may be needed to determine if this is a significant factor. This suggests that the decrease in blood flow in oral tissues in an infusion rate–dependent manner reported by Koshika et al11 may possibly apply to humans. This suggestion should be validated clinically by a randomized controlled trial or other means.
With respect to the maintenance anesthetic, a comparison of the use of sevoflurane and propofol in maxillary sinus surgery found that blood loss was lower in patients who were given propofol.19,20 According to Koshika et al,11 however, neither sevoflurane nor propofol had any differential effect on blood flow in oral tissues. No significant difference in blood loss was observed between sevoflurane and propofol, suggesting that the type of maintenance anesthetic used may not have a major effect on blood loss in orthognathic surgery. Significant differences in heart rate between 2 groups (total blood loss ≥5 mL/kg or <5 mL/kg) were not observed in this study, and thus, heart rate, 1 of 2 components of cardiac output, did not appear to be a major contributor to reduction of blood loss.
Although deliberate hypotension has been reported to be available to reduce bleeding during surgery, there are many reports of critical complications.5–8 Since remifentanil can stabilize blood pressure and reduce blood loss without excessive hypotension,11 remifentanil may be a good candidate to reduce blood loss for orthognathic surgery. However, large-dose remifentanil may induce significant cardiovascular depression and hyperalgesia after surgery.21–23 Therefore, further study will be needed to determine the appropriate dose of remifentanil to obtain maximal effect to reduce blood loss while minimizing adverse effects.
In conclusion, we retrospectively investigated whether the use of remifentanil decreased intraoperative blood loss in patients undergoing orthognathic surgery and found that the use of remifentanil and smaller variations in SBP (CVSBP) were associated with the reduction of blood loss. Logistic regression analysis revealed that the use of remifentanil (odds ratio 3.112) was more strongly associated with blood loss reduction than CVSBP.
Acknowledgments
Funding: Departmental sources.
Conflict of interest: None.
Institutional review board: Tokyo Dental College Ethics Committee approved this study (approval No. 464). The requirement for written informed consent was waived by the Tokyo Dental College Ethics Committee.
REFERENCES
- 1. Fukunaga AF, Flacke WE, Bloor BC. . Hypotensive effects of adenosine and adenosine triphosphate compared with sodium nitroprusside. Anesth Analg. 1982; 61: 273– 278. [PubMed] [Google Scholar]
- 2. Bloor BC, Fukunaga AF, Ma C, et al. Myocardial hemodynamics during induced hypotension: a comparison between sodium nitroprusside and adenosine triphosphate. Anesthesiology. 1985; 63: 517– 525. [DOI] [PubMed] [Google Scholar]
- 3. Kaneko Y. . Clinical experiences and physiological response to induced hypotensive anesthesia during oral and maxillofacial surgery: especially on ATP (In Japanese). Shikwa Gakuho. 1987; 87: 1159– 1170. [PubMed] [Google Scholar]
- 4. Choi WS, Samman N. . Risks and benefits of deliberate hypotension in anaesthesia: a systematic review. Int J Oral Maxillofac Surg. 2008; 37: 687– 703. [DOI] [PubMed] [Google Scholar]
- 5. Davies DW, Greiss L, Kadar D, Steward DJ. . Sodium nitroprusside in children: observations on metabolism during normal and abnormal responses. Can Anaesth Soc J. 1975; 22: 553– 560. [DOI] [PubMed] [Google Scholar]
- 6. Pasch T, Huk W. . Cerebral complications following induced hypotension. Eur J Anaesthesiol. 1986; 3: 299– 312. [PubMed] [Google Scholar]
- 7. Enlund M, Ahlstedt B, Revenas B, Krekmanov L, Ronquist G. . Adverse effects on the brain in connection with isoflurane-induced hypotensive anaesthesia. Acta Anaesthesiol Scand. 1989; 33: 413– 415. [DOI] [PubMed] [Google Scholar]
- 8. Dong Y, Teoh HL, Chan BP, et al. Changes in cerebral hemodynamic and cognitive parameters after external carotid-internal carotid bypass surgery in patients with severe steno-occlusive disease: a pilot study. J Neurol Sci. 2012; 322: 112– 116. [DOI] [PubMed] [Google Scholar]
- 9. Tassoudis V, Vretzakis G, Petsiti A, et al. Impact of intraoperative hypotension on hospital stay in major abdominal surgery. J Anesth. 2011; 25: 492– 499. [DOI] [PubMed] [Google Scholar]
- 10. Kemmochi M, Ichinohe T, Kaneko Y. . Remifentanil decreases mandibular bone marrow blood flow during propofol or sevoflurane anesthesia in rabbits. J Oral Maxillofac Surg. 2009; 67: 1245– 1250. [DOI] [PubMed] [Google Scholar]
- 11. Koshika K, Ichinohe T, Kaneko Y. . Dose-dependent remifentanil decreases oral tissue blood flow during sevoflurane and propofol anesthesia in rabbits. J Oral Maxillofac Surg. 2011; 69: 2128– 2134. [DOI] [PubMed] [Google Scholar]
- 12. Patel SS, Spencer CM. . Remifentanil. Drugs. 1996; 52: 417– 427. [DOI] [PubMed] [Google Scholar]
- 13. Manyam SC, Gupta DK, Tohnson KB, et al. Opioid-Volatile anesthetic synergy: a response surface model with remifentanil and sevoflurane as prototypes. Anesthesiology. 2006; 105: 267– 278. [DOI] [PubMed] [Google Scholar]
- 14. Koitabashi T. . Remifentanil anesthesia: efficacy and the prevention of adverse effects [in Japanese]. J Japan Soc Clin Anesth. 2009; 29: 455– 466. [Google Scholar]
- 15. Nooh N, Abdelhalim AA, Abdullah WA, Sheta SA. . Effect of remifentanil on the hemodynamic responses and recovery profile of patients undergoing single jaw orthognathic surgery. Int J Oral Maxillofac Surg. 2013; 42: 988– 993. [DOI] [PubMed] [Google Scholar]
- 16. Wakasugi Y, Matsuura N, Ichinohe T. . Intraoperative blood loss during orthognathic surgery: a comparison of remifentanil-based anesthesia with sevoflurane or isoflurane. J Oral Maxillofac Surg. 2015; 73: 2294– 2299. [DOI] [PubMed] [Google Scholar]
- 17. Kawano H, Manabe S, Matsumoto T, et al. Comparison of intraoperative blood loss during spinal surgery using either remifentanil or fentanyl as an adjuvant to general anesthesia. BMC Anesthesiol. 2013; 13: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dolman RM, Bentley KC, Head TW, English M. . The effect of hypotensive anesthesia on blood loss operative time during Le Fort 1 Osteotomies. J Oral Maxillofac Surg. 2000; 58: 834– 839. [DOI] [PubMed] [Google Scholar]
- 19. Sivaci R, Yilmaz MD, Balci C, Erincler T, Unlu H. . Comparison of propofol and sevoflurane anesthesia by means of blood loss during endoscopic sinus surgery. Saudi Med J. 2004; 25: 1995– 1998. [PubMed] [Google Scholar]
- 20. Miłoński J, Zielińska-Bliźniewska H, Golusiński W, Urbaniak J, Sobański R, Olszewski J. . Effect of three different type of anesthesia on perioperative bleeding control in functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2013; 270: 2045– 2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reid JE, Mirakhur RK. . Bradycardia after administration of remifentanil. Br J Anaesth. 2000; 84: 422– 423. [DOI] [PubMed] [Google Scholar]
- 22. Guignard B, Bossard AE, Coste C, et al. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000; 93: 409– 417. [DOI] [PubMed] [Google Scholar]
- 23. Kurdi O, Deleuze A, Marret E, Bonnet F. . Asystole during anaesthetic induction with remifentanil and sevoflurane. Br J Anaesth. 2001; 87: 943. [PubMed] [Google Scholar]


