Abstract
Background
The definition of osseous instability in radiographic borderline dysplastic hips is difficult. A reliable radiographic tool that aids decision-making—specifically, a tool that might be associated with instability—therefore would be very helpful for this group of patients.
Questions/purposes
(1) To compare a new radiographic measurement, which we call the Femoro-Epiphyseal Acetabular Roof (FEAR) index, with the lateral center-edge angle (LCEA) and acetabular index (AI), with respect to intra- and interobserver reliability; (2) to correlate AI, neck-shaft angle, LCEA, iliocapsularis volume, femoral antetorsion, and FEAR index with the surgical treatment received in stable and unstable borderline dysplastic hips; and (3) to assess whether the FEAR index is associated clinical instability in borderline dysplastic hips.
Methods
We defined and validated the FEAR index in 10 standardized radiographs of asymptomatic controls using two blinded independent observers. Interrater and intrarater coefficients were calculated, supplemented by Bland-Altman plots. We compared its reliability with LCEA and AI. We performed a case-control study using standardized radiographs of 39 surgically treated symptomatic borderline radiographically dysplastic hips and 20 age-matched controls with asymptomatic hips (a 2:1 ratio), the latter were patients attending our institution for trauma unrelated to their hips but who had standardized pelvic radiographs between January 1, 2016 and March 1, 2016. Patient demographics were assessed using univariate Wilcoxon two-sample tests. There was no difference in mean age (overall: 31.5 ± 11.8 years [95% CI, 27.7–35.4 years]; stable borderline group: mean, 32.1± 13.3 years [95% CI, 25.5–38.7 years]; unstable borderline group: mean, 31.1 ± 10.7 years [95% CI, 26.2–35.9 years]; p = 0.96) among study groups. Treatment received was either a periacetabular osteotomy (if the hip was unstable) or, for patients with femoroacetabular impingement, either an open or arthroscopic femoroacetabular impingement procedure. The association of received treatment categories with the variables AI, neck-shaft angle, LCEA, iliocapsularis volume, femoral antetorsion, and FEAR index were evaluated first using Wilcoxon two-sample tests (two-sided) followed by stepwise multiple logistic regression analysis to identify the potential associated variables in a combined setting. Sensitivity, specificity, and receiver operator curves were calculated. The primary endpoint was the association between the FEAR index and instability, which we defined as migration of the femoral head either already visible on conventional radiographs or recentering of the head on AP abduction views, a break of Shenton’s line, or the appearance of a crescent-shaped accumulation of gadolinium in the posteroinferior joint space at MR arthrography.
Results
The FEAR index showed excellent intra- and interobserver reliability, superior to the AI and LCEA. The FEAR index was lower in the stable borderline group (mean, −2.1 ± 8.4; 95% CI, −6.3 to 2.0) compared with the unstable borderline group (mean, 13.3 ± 15.2; 95% CI, 6.2–20.4) (p < 0.001) and had the highest association with treatment received. A FEAR index less than 5° had a 79% probability of correctly assigning hips as stable and unstable, respectively (sensitivity 78%; specificity 80%).
Conclusions
A painful hip with a LCEA of 25° or less and FEAR index less than 5° is likely to be stable, and in such a situation, the diagnostic focus might more productively be directed toward femoroacetabular impingement as a potential cause of a patient’s pain, rather than instability.
Level of Evidence
Level III, diagnostic study.
Introduction
The borderline dysplastic hip is currently a subject of controversy in adult hip-preservation surgery [3, 5, 15]. The debate is nurtured by the difficulty in classifying the underlying problem correctly. Although knowledge and imaging have contributed substantially to the understanding of pathobiomechanics, it often remains unclear whether the underlying problem is instability (dysplasia) or femoroacetabular impingement (FAI). However, this is of paramount importance because for an unstable hip, the preferred surgical treatment would be a periacetabular osteotomy, whereas with FAI, the treatment would be open or arthroscopic impingement surgery.
The lateral center-edge angle (LCEA) of Wiberg traditionally has been used to classify hips as normal (LCEA > 25°), dysplastic (LCEA < 20°), or borderline (LCEA 20°–25°) [1]. Often with borderline hips it is unclear whether the hip should be categorized as having impingement (stable) or as dysplastic (unstable). Thus, it is difficult to decide if the better treatment would be surgery to correct suspected cam-type FAI (in the presence of dysplasia, pincer FAI is unlikely even if the socket were to be retroverted), or a reorientation of the acetabulum to treat the unstable, dysplastic hip. Unfortunately LCEA per se cannot predict stability in the borderline hip nor direct surgical management [5, 9, 21]. A radiographic method to predict pathologic behavior in borderline hips potentially would help to guide surgical management decisions.
During development, physeal growth of the proximal femur is affected directly by the forces acting across it. Growth and the orientation of the femoral neck are under the control of the subcapital growth plate [9]. Pauwels and Maquet [18] theorized that the resultant force acts from the center of the epiphyseal cartilage and that during growth, the epiphyseal plate orients itself perpendicular to the joint reaction force in accordance with the Heuter-Volkman principle. Pauwels and Maquet’s theory later was confirmed by Carter et al. [4] who studied the influence of hip loading by bidimensional finite element analysis. The angle of the closed epiphyseal plate indicates the balance of forces across the proximal femoral physis [6].
In theory, the angle measured between the central part of the physeal scar of the femoral head growth plate and the acetabular index (AI) angle would reveal the resultant force vector, which then could be used to predict the behavior of the borderline hip. In theory, a laterally directed vector (which we defined as a more-positive value) would imply forces that potentiate hip instability, whereas a medially directed vector would not and may be associated with impingement (a more-negative value).
We theorized that this new parameter would correlate with pathologic behavior in borderline dysplastic hips. Because the consequences of hip arthroscopy in unstable hips can be severe [12, 13, 15, 17], we named this angle the Femoro-Epiphyseal Acetabular Roof (FEAR) index. This study was performed to verify a possible correlation between this new parameter and either unstable or stable borderline dysplastic hips. Specifically, we sought (1) to compare a new radiographic measurement, the FEAR index, with the LCEA and AI, with respect to intra- and interobserver reliability; (2) to correlate AI, neck-shaft angle, LCEA, iliocapsularis volume, femoral antetorsion, and FEAR index with the surgical treatment received in stable and unstable borderline dysplastic hips; and (3) to assess whether the FEAR index is associated with clinical instability in borderline dysplastic hips.
Patients and Methods
Validation of the FEAR Index
Standardized AP pelvic radiographs of 10 asymptomatic control patients treated for unrelated trauma at our institution during January 2016 were selected for the measurements. No patients had prior hip problems. Using the digital measurement tools on the Merlin picture archiving and communication system (PACS) (Phönix Merlin Software 5.0; Phönix PACS GmbH, Freiburg, Germany), two independent reviewers (MCW and JW) measured the FEAR index, LCEA, and AI, which we defined as the angle of the sourcil versus the horizontal (Fig. 1).
Fig. 1A–C.
Our measurements, using the picture archiving and communication system (PACS) measurement device, of (A) the FEAR index; (B) LCEA; and (C) AI are shown.
Measurement of the FEAR Index
The physeal scar of the femoral head normally has a slightly irregular but consistent shape. The central third radiographically is a straight line that then curves distal-medially and distal-laterally to the femoral neck. The most lateral and medial points of the straight section were identified and connected with the first inflection of this line. The second part of the angle is defined by the most medial and lateral points of the sclerosis of the sourcil. We defined a positive FEAR index as a laterally directed angle, with the apex formed by the femoral epiphysis and the AI pointing medially. A negative index was a medially directed angle, with the apex formed by the femoral epiphysis and the AI pointing laterally.
Measurement of the LCEA of Wiberg
The center of the femoral head is defined by a circle fitting the contour of the femoral head. The first branch of the angle runs perpendicular through the center of rotation. The second branch is defined by the center of the femoral head and the most lateral point of the sourcil [20]. It is important not to use the most lateral point of the acetabulum, because this does not follow the definition of Wiberg, and will give false high values [16]. Statistical reliability testing was performed with intraclass correlation values interpreted as: greater than 0.75 = excellent, 0.40–0.75 = fair to good, and less than 0.40 = poor.
Case-control Study of Borderline Hips
The radiographs of all 266 hips (266 patients) from our institution who underwent joint-preserving surgery of the hip between August 1, 2008, and August 1, 2012, were analyzed and their hips were categorized as normal (LCEA > 25°) or abnormal (LCEA of 25° or less). Only hips with a LCEA less than 25° were included and we considered those with a LCEA greater than 25° normal. Because the radiographic classification of “borderline dysplastic” (LCEA > 20° and < 25°) and “dysplastic” (LCEA < 20°) is unreliable with respect to stability, all hips with a LCEA less than 25°, including the dysplastic hips, were included. All patients had at least 2 years of followup. Exclusion criteria were those with femoral head deformities that prevented measurement of the LCEA, Tönnis osteoarthritis grade greater than 1, hips with previous surgery, concomitant subtrochanteric osteotomy for treatment of high femoral antetorsion, and a clinical result with a Merle d’Aubigné score less than 16. Of the 266 hips, 45 met the inclusion criteria with a LCEA of 25° or less. Two hips, both in the FAI group, were excluded because they had a Merle d’Aubigné score less than 16. Four hips had a concomitant femoral derotation osteotomy and also were excluded. Therefore, 39 symptomatic borderline hips were included in the study, of which 21 were identified as unstable and underwent a periacetabular osteotomy. Nineteen patients were considered to have stable hips and had FAI correction. The 20 asymptomatic controls with a LCEA greater than 25° were those who were treated at our institution for trauma unrelated to their hips but who had standardized pelvic radiographs between January 1, 2016 to March 1, 2016. We recorded age and sex on all patients. All patient data were anonymous. The study population consisted of 61% women and the women were older than the men (35 years ±10.3 versus 25 years ±12.1; p = 0.05) (Table 1).
Table 1.
Age of patients at surgery versus the control group
| Treatment | Number of patients | Mean (years) | SD (years) | 25% percentile | 75% percentile | Lower confidence limit | Upper confidence limit | Minimum (years) | Maximum (years) |
|---|---|---|---|---|---|---|---|---|---|
| Impingement (31%) | 18 | 32 | 13 | 20 | 44 | 25 | 38 | 14 | 55 |
| Dysplasia (36%) | 21 | 31 | 10 | 22 | 41 | 26 | 35 | 15 | 46 |
| Control (34%) | 20 | 37 | 11 | 29 | 48 | 31 | 42 | 15 | 52 |
| Total (100%) | 59 | 33 | 11 | 22 | 43 | 30 | 36 | 14 | 55 |
Kruskal-Wallis test (df = 2): p = 0.241; F-test (df = 2): p = 0.229.
As we believe that the terms “dysplastic” and “borderline dysplastic” are obsolete (are only radiographic parameters) and should be replaced or supplemented by a functional analysis that evaluates the stability of the hip, all hips with a LCEA of 25° or less were analyzed for signs of instability. Therefore hips were classified as unstable or stable and received either a periacetabular osteotomy to treat the instability or open or arthroscopic FAI surgery. A hip was considered unstable when radiographic signs of instability were present, namely migration of the femoral head either already visible on conventional radiographs as an increased distance from the ilioischial line or recentering of the head on AP abduction views, a break of Shenton’s line, or the appearance of a crescent-shaped accumulation of gadolinium in the posteroinferior joint space at MR arthrography. A positive crescent sign was present if gadolinium was visible on two of three planes (axial, sagittal, and radial) between the posterior horn and the posterior femoral head. To be able to differentiate and analyze the new FEAR index, all hips with a LCEA of 25° or less, and all potentially unstable hips have to be included. We aimed to define a reliable cutoff between those two groups. Therefore clearly dysplastic hips also have to be included. In addition, we added a control group of normal hips (LCEA > 25°).
We then measured the following radiographic parameters in each group: AI, LCEA, neck-shaft angle, femoral antetorsion, iliocapsularis volume as described previously [1], and the FEAR index. In addition, the FEAR index, LCEA, and AI were measured in 20 asymptomatic hips and compared with the two other groups. The two assessors (MCW and JW) of the FEAR index were blinded to the treatment received to prevent assessor bias. Each parameter was examined for statistical differentiation between groups and for correlation with other parameters. One patient had a missing assessment for the FEAR index and was not included in the statistical analyses, thus reducing the set of patients with dysplasia from 21 to 20.
Corroborative Analysis
The primary endpoint was the association between the FEAR index and instability. Instability was defined as lateral and/or anterior migration or subluxation of the femoral head and depends primarily on the osseous geometry of the acetabulum. There may be instability attributable to soft tissue insufficiency, but this is more likely to be seen in normal osseous anatomy of the hip and therefore is not part of our investigation. We also sought to correlate the other angles with instability, to see which was most sensitive and most specific. Finally, we sought to evaluate the association between the various measurements of interest (FEAR index, AI, neck-shaft angle, LCEA, iliocapsularis volume, and femoral antetorsion), and whether a patient had surgery for FAI, for dysplasia, or no surgery.
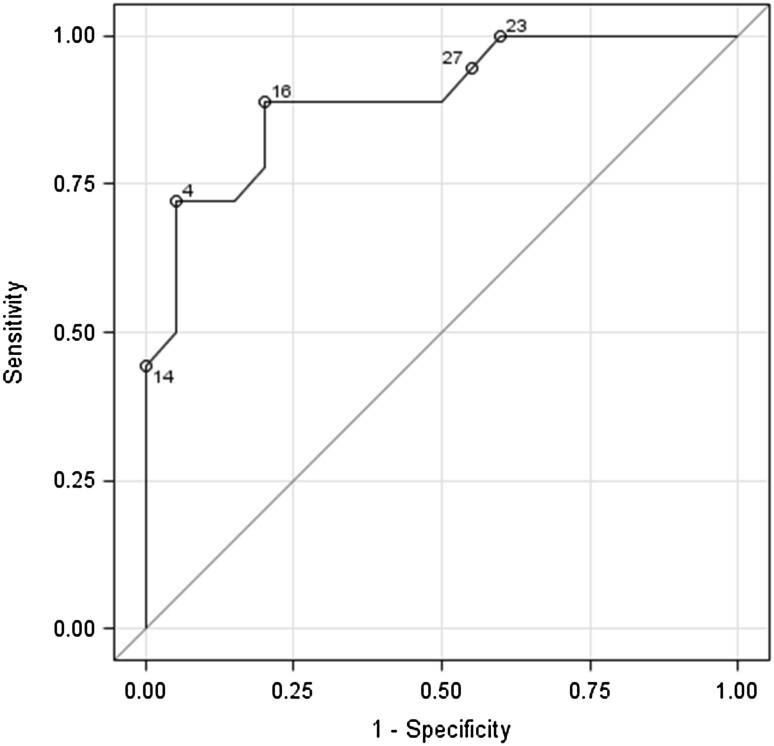
A multivariate prediction analysis model was created using stepwise logistic regression. This permitted construction of a receiver operator curve (ROC). Cutoff values were identified and sensitivity and specificity calculated. This model then was tested using discriminant analysis.
Statistical Methodology
All statistical analyses were performed using SAS® software, Version 9.3 (SAS Institute, Cary, NC, USA).
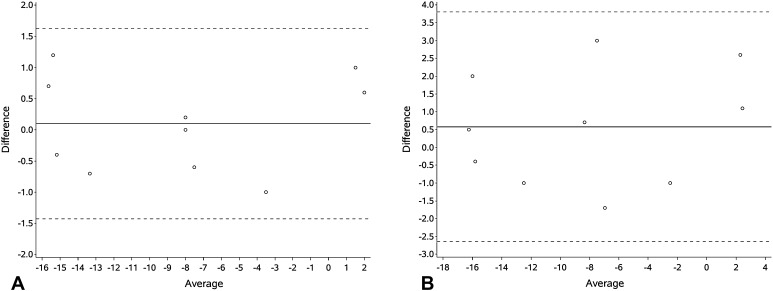
Validity testing of the FEAR index, center-edge angle, and AI was done using the intraclass correlation coefficient (ICC) [19]. ICC values were interpreted as follows: > 0.75 was excellent, 0.40–0.75 was fair to good, and < 0.40 was considered poor [7]. Bland-Altman graphs were constructed to display interobserver agreement [2].
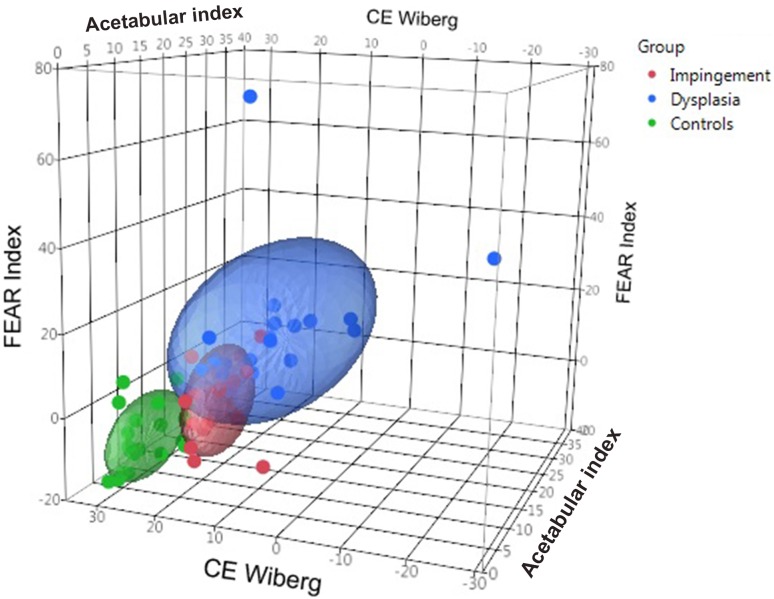
Comparisons of age and gender demographics were performed using Kruskal-Wallis tests (2 degrees of freedom) and Wilcoxon two-sample tests (1 degree of freedom), the latter also was used to examine stable and unstable hips to identify potential predictors as a means of univariate analyses. Correlation of radiographic parameters was explored using Spearman correlation coefficients and graphically with a three-dimensional scatterplot.
To examine potential predictor variables, an analysis using multiple logistic regression was done applying stepwise selection to retain only significant variables in the model. Cutoff probabilities and sensitivity and specificity values were calculated guided by a ROC to fine-tune selecting optimal cutoff values. As a means of sensitivity analysis, the records with lowest and highest values of the predictor variable were discarded and the identified prediction model was repeated.
Results
The FEAR index showed excellent inter- and intraobserver agreement. The reliability of the FEAR index was then compared with the LCEA and AI (Table 2). The inter- and intraobserver reliability was fair to good for the LCEA, whereas the AI was excellent for both yet inferior to the FEAR index. The FEAR index did not vary substantially between assessors for each replication (Fig. 2).
Table 2.
Intraclass correlation coefficients (ICC)
| Measure | ICC First measurement |
ICC Second measurement |
Agreement |
|---|---|---|---|
| Intraobserver reliability | |||
| AI | 0.93 | 0.91 | Excellent |
| LCEA | 0.74 | 0.55 | Fair to good |
| FEAR index | 0.99 | 0.99 | Excellent |
| Rater = JW | Rater = MW | ||
| Intraobserver reliability | |||
| AI | 0.95 | 0.95 | Excellent |
| LCEA | 0.73 | 0.68 | Fair to good |
| FEAR Index | 0.99 | 0.99 | Excellent |
AI = acetabular index; LCEA = lateral center-edge angle; FEAR = Femoro-Epiphyseal Acetabular Roof; JW = Jan Weidner; MW = Michael Wyatt.
Fig. 2A–B.
Bland-Altman plots are shown for the FEAR index for the (A) first and (B) second measurements.
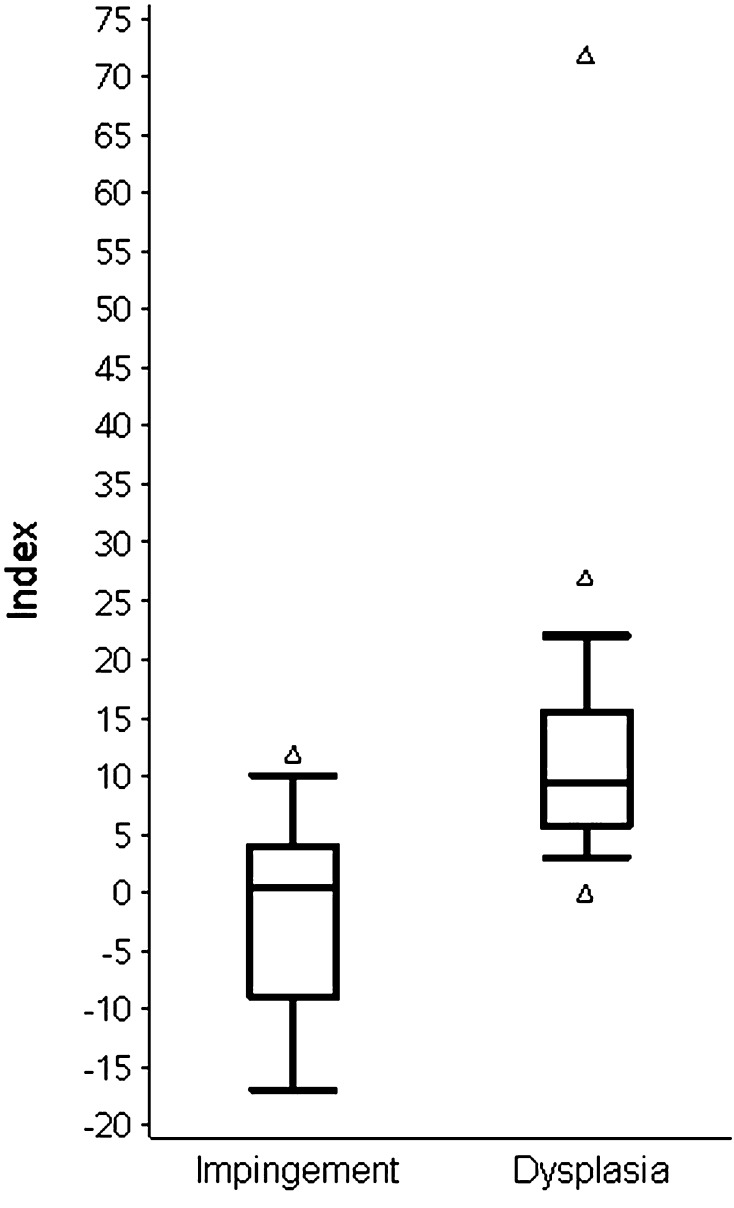
There was no difference in mean age (overall: 31.5 ± 11.8 years [95% CI, 27.7–35.4 years]; stable borderline group: mean, 32.1 ± 13.3 years [95% CI, 25.5–38.7 years]; unstable borderline group: mean, 31.1 ± 10.7 years [95% CI, 26.2–35.9 years]) between study groups.. The FEAR index was higher among the groups with FAI and unstable treatment compared with the asymptomatic control group (mean −2.1 ± 8.4 and 13.3 ± 15.2 respectively versus −7.7 ± 7.1 for controls; p < 0.001) (Fig. 3). In addition, the FEAR index yielded the greatest distinction with respect to treatment status (impingement borderline group mean −2.1 ± 8.4 versus unstable borderline group mean 13.3 ± 15.2; p < 0.001) compared with the LCEA (impingement borderline group 20 ± 3.1 versus unstable borderline group mean 13.7 ± 8.3; p < 0.001) and AI (impingement borderline group 13.6 ± 3.6 versus unstable borderline group mean 19.2 ± 6.8; p = 0.006), respectively (Fig. 4). Iliocapsularis volume, neck-shaft angle, and femoral antetorsion did not discriminate between treatment groups. However, in our study, iliocapsularis volume had a positive association with femoral antetorsion, that is, a larger iliocapsularis volume was associated with greater antetorsion.
Fig. 3.
A box plot of the FEAR index versus treatment group is shown.
Fig. 4.
A three-dimensional scattergraph shows the LCEA, AI, and FEAR index.
After controlling for age and gender, the FEAR index was lower in the stable borderline group (mean, −2.1± 8.4; 95% CI, −6.3 to 2.0) compared with the unstable borderline group (mean, 13.3 ± 15.2; 95% CI, 6.2–20.4; p < 0.001) and had the highest association with treatment received. Stepwise logistic regression identified the FEAR index as the only parameter associated with instability in the model (p = 0.004). We found that a FEAR index less than 5° yielded the best distinction between the symptomatic borderline dysplastic hip pathologic behavior being instability or FAI using a fine-tuned cutoff probability of 0.45 (Table 3). Thus, using the respective angle of less than 5° as a cutoff, 79% of patients were correctly identified as either having an unstable or stable hip using the FEAR index (Table 4). This is shown graphically (Fig. 5). The value of area under the curve in this ROC curve being close to the upper left corner indicates that the FEAR index has a very high association with instability.
Table 3.
Classification of FEAR index angle versus sensitivity and specificity in prediction of behavior
| Probability level | Correct nonevent | Correct event | Incorrect nonevent | Incorrect event | Sensitivity (%) | Specificity (%) | False negative (%) | False positive (%) |
|---|---|---|---|---|---|---|---|---|
| 0.35 | 16 | 13 | 7 | 2 | 76 | 89 | 30 | 13 |
| 0.4 | 16 | 14 | 6 | 2 | 79 | 89 | 27 | 12 |
| 0.45 | 14 | 16 | 4 | 4 | 79 | 78 | 22 | 20 |
| 0.5 | 13 | 16 | 4 | 5 | 76 | 72 | 23 | 23 |
| 0.55 | 13 | 16 | 4 | 5 | 76 | 72 | 23 | 23 |
| 0.6 | 13 | 17 | 3 | 5 | 79 | 72 | 18 | 22 |
| 0.65 | 13 | 19 | 1 | 5 | 84 | 72 | 7 | 20 |
FEAR = Femoro-Epiphyseal Acetabular Roof.
Table 4.
Summary of radiographic parameters by group
| Parameter | Number of observations | Mean (degrees) | SD (degrees) | Median (degrees) | 25% Percentile | 75% Percentile |
|---|---|---|---|---|---|---|
| Acetabular roof angle | ||||||
| Impingement | 18 | 13 | 4 | 13 | 11 | 16 |
| Dysplasia | 21 | 19 | 7 | 17 | 15 | 23 |
| Neck-shaft angle | ||||||
| Impingement | 18 | 135 | 6 | 134 | 132 | 140 |
| Dysplasia | 21 | 141 | 9 | 141 | 133 | 147 |
| LCEA | ||||||
| Impingement | 18 | 20 | 3 | 21 | 19 | 22 |
| Dysplasia | 21 | 14 | 8 | 17 | 10 | 19 |
| Iliocapsularis volume | ||||||
| Impingement | 16 | 144 | 62 | 136 | 94 | 183 |
| Dysplasia | 15 | 145 | 29 | 144 | 125 | 162 |
| FEAR index | ||||||
| Impingement | 18 | −2 | 8 | 0.5 | −9.0 | 4 |
| Dysplasia | 20 | 13 | 15 | 10 | 6 | 16 |
LCEA = lateral center-edge angle; FEAR = Femoro-Epiphyseal Acetabular Roof.
Fig. 5.
The ROC for FEAR index model is shown (area under the curve = 0.8944).
Discussion
Borderline dysplastic is a radiographic definition that is quantified by the LCEA [19]. Unfortunately this radiographic finding does not give any indication regarding the clinical stability of the hip. Additional factors contribute to instability; these include antetorsion, acetabular roof inclination, and neck shaft angle. Although the categorization of borderline hips as stable or unstable is necessary for successful treatment of these hips, this can be difficult to do in practice and may lead to incorrect treatment. In particular, if one mistakenly surmises the problem is FAI rather than instability and performs hip arthroscopy to treat it, this likely will result in persistent symptoms from instability. The question that has to be addressed is not whether a hip is dysplastic or borderline dysplastic, but whether the hip is stable or unstable. The key therefore is to classify the hip accurately as one or the other and then treat it accordingly. Traditionally, the LCEA was used to categorize hips as normal, borderline, or dysplastic. However, the LCEA does not always predict stability of the hip. To aid decision-making, we have proposed a new radiographic parameter that can be measured reliably on standardized AP pelvic radiographs. The purpose of this study was to evaluate this FEAR index to see whether it is associated with pathologic behavior in the borderline-unstable hip.
The study is limited because with the small number of patients included, precise patient matching could not be performed. More-exhaustive matching for parameters like signs of generalized ligamentous laxity, BMI, and muscular conditioning would be advantageous. Furthermore, a retrospective study allows us to show associations but not to make predictions. Therefore future prospective studies to show whether the FEAR index predicts progressive instability are warranted. We also defined instability by various parameters, including pooling of gadolinium posteroinferiorly on MR arthrography, recentering of the femoral head or a break in Shenton’s line and rather than on a purely radiographic basis; this results in a functional definition of instability. We attempted to address the issue of assessor bias by having two individuals blinded to the treatments patients received perform the measurements.
The findings from our study show that our new index shows excellent inter- and intraobserver reliability and was superior to the LCEA and AI. This superiority may be because of difficulty in defining the edge of the acetabular sourcil as has been alluded to [16].
A couple of studies have been published looking specifically at the results of surgical treatment of borderline dysplastic hips, with one study showing higher rates of failure in the borderline hips than in those with adequate acetabular cover [10], and the other study showing comparable outcomes [15]. Currently stability of the hip is assessed with the LCEA. Realizing the limitations of the LCEA, there have been attempts to use other parameters in borderline hips as surrogate markers for hip instability, such as the size of the labrum or the volume of the iliocapsularis, both structures known often to be hypertrophic in hip dysplasia [1, 8, 11]. Introducing the FEAR index is a new attempt to assess functional stability of the hip, based on the biomechanical concept that the growth plate orients itself perpendicularly to the joint reacting forces during growth [5, 6, 8, 9]. In the control group and the stable borderline group, the FEAR index had a medially open angle, that is, a medially directed vector, indicating medial-directed joint-reaction forces and stability. In the dysplastic group (13°), the angle opened laterally, indicating joint-reaction forces favoring lateral migration and instability of the joint.
Our study did not support the iliocapsularis volume as a discriminator in borderline dysplastic hips. This is contrary to the study by Babst et al. [1]. This probably is attributable to patient selection. Babst et al. [1] compared dysplastic hips with hips with pincer FAI and we compared unstable with stable borderline hips, the anatomic difference being only minimal. We recommend further research to examine this, because our study showed a correlation between iliocapsularis volume with femoral antetorsion.
Statistical modeling of the FEAR index suggests that this could become a useful tool in identifying borderline hips that likely will behave as stable. This could prove advantageous in identifying hips that would be appropriate for hip arthroscopy. With 79% correctly identified as stable borderline hips with a sensitivity of 80% and specificity of 78%, the FEAR index seems suitable to identify stable hips. The ability of the FEAR index to identify instability was less encouraging and this may reflect other factors such as ligamentous laxity being pertinent in the decision-making process. Interestingly, hypermobility has been noted to be more prevalent in symptomatic patients with FAI [10, 14].
We believe the FEAR index might be applied in the context of a thorough clinical and radiographic workup including standard radiographs, and preferably MR arthrography remains the standard first step. MR arthrography is superior to MRI for detection of hip instability because the crescent sign can be observed. Signs of instability, like migration of the femoral head on standard radiographs and the crescent sign on MR arthrography, have to be looked for. If present, the hip has to be stabilized with a periacetabular osteotomy. If one is still undecided whether the hip is stable, the FEAR index can be used to assess the likelihood of stability.
We found that if a patient presents with hip pain and borderline dysplasia (defined as a LCEA 20° to 25°), a FEAR index less than 5° indicates an 80% probability that the hip is stable, and if the FEAR index increases by 1°, the odds of having impingement decreases by 24%. In that situation, FAI seems more likely than dysplasia; however, other causes should be considered and excluded before determining a diagnosis of FAI. Surgical treatment, if indicated, should be selected accordingly. Further studies are needed to validate the FEAR index prospectively.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
A comment to this article is available at http://dx.doi.org/10.1007/s11999-016-5207-3.
References
- 1.Babst D, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. The iliocapsularis muscle: an important stabilizer in the dysplastic hip. Clin Orthop Relat Res. 2011;469:1728–1734. doi: 10.1007/s11999-010-1705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055–1060. doi: 10.1016/j.arthro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Carter DR, Orr TE, Fyrie DP, Schurman DJ. Influences of mechanical stress on prenatal and postnatal skeletal development. Clin Orthop Relat Res. 1987;219:237–250. [PubMed] [Google Scholar]
- 5.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 6.Fabeck L, Tolley M, Rooze M, Burny F. Theoretical study of the decrease in the femoral neck anteversion during growth. Cells Tissues Organs. 2002;171:269–275. doi: 10.1159/000063127. [DOI] [PubMed] [Google Scholar]
- 7.Fleiss J. The Design and Analysis of Clinical Experiments. New York, NY: John Wiley & Sons; 1986. [Google Scholar]
- 8.Garabekyan T, Ashwell Z, Chadayammuri V, Jesse MK, Pascual-Garrido C, Petersen B, Mei-Dan O. Lateral acetabular coverage predicts the size of the hip labrum. Am J Sports Med. 2016;44:1582–1589. doi: 10.1177/0363546516634058. [DOI] [PubMed] [Google Scholar]
- 9.Hunziker EB. Mechanism of longitudinal bone growth and its regulation by growth plate chondrocytes. Microsc Res Tech. 1994;28:505–519. doi: 10.1002/jemt.1070280606. [DOI] [PubMed] [Google Scholar]
- 10.Kalore NV, Jiranek WA. Save the torn labrum in hips with borderline acetabular coverage. Clin Orthop Relat Res. 2012;470:3406–3413. doi: 10.1007/s11999-012-2499-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74–80. doi: 10.1097/00003086-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Matsuda DK, Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy. 2012;28:1738–1743. doi: 10.1016/j.arthro.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic Instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Naal FD, Hatzung G, Müller A, Impellizzeri F, Leunig M. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. Int Orthop. 2014;38:2245–2250. doi: 10.1007/s00264-014-2424-9. [DOI] [PubMed] [Google Scholar]
- 15.Nawabi DH, Degen RM, Fields KG, McLawhorn A, Ranawat AS, Sink EL, Kelly BT. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44:1017–1023. doi: 10.1177/0363546515624682. [DOI] [PubMed] [Google Scholar]
- 16.Omeroglu H, Biçimoglu A, Aguş H, Tümer Y. Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol. 2002;31:25–29. doi: 10.1007/s002560100402. [DOI] [PubMed] [Google Scholar]
- 17.Parvizi J, Bican O, Bender B, Mortazavi SM, Purtill JJ, Erickson J, Peters C. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24(6 suppl):110–113. doi: 10.1016/j.arth.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 18.Pauwels F, Maquet P. Biomechanics of the Locomotor Apparatus: Contributions on the Functional Anatomy of the Locomotor Apparatus. In: Maquet P, Furlong R, trans. Berlin, Germany: Springer-Verlag; 1980.
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 20.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. JAMA. 1940;115:81. [Google Scholar]
- 21.Zaltz I, Kelly BT, Larson CM, Leunig M, Bedi A. Surgical treatment of femoroacetabular impingement: what are the limits of hip arthroscopy? Arthroscopy. 2014;30:99–110. doi: 10.1016/j.arthro.2013.10.005. [DOI] [PubMed] [Google Scholar]