Abstract
Ovarian cancer is the deadliest gynecologic cancer. Receipt of treatment from a gynecologic oncologist is an evidence-based recommendation to reduce mortality from the disease. We examined knowledge and application of this evidence-based recommendation in primary care physicians as part of CDC gynecologic cancer awareness campaign efforts and discussed results in the context of CDC National Comprehensive Cancer Control Program (NCCCP). We analyzed primary care physician responses to questions about how often they refer patients diagnosed with ovarian cancer to gynecologic oncologists, and reasons for lack of referral. We also analyzed these physicians’ knowledge of tests to help determine whether a gynecologic oncologist is needed for a planned surgery. The survey response rate was 52.2%. A total of 84% of primary care physicians (87% of family/general practitioners, 81% of internists and obstetrician/gynecologists) said they always referred patients to gynecologic oncologists for treatment. Common reasons for not always referring were patient preference or lack of gynecologic oncologists in the practice area. A total of 23% of primary care physicians had heard of the OVA1 test, which helps to determine whether gynecologic oncologist referral is needed. Although referral rates reported here are high, it is not clear whether ovarian cancer patients are actually seeing gynecologic oncologists for care. The NCCCP is undertaking several efforts to assist with this, including education of the recommendation among women and providers and assistance with treatment summaries and patient navigation toward appropriate treatment. Expansion of these efforts to all populations may help improve adherence to recommendations and reduce ovarian cancer mortality.
Introduction
Over 14,000 women die from ovarian cancer each year, and it is the fifth leading cause of cancer death among women in the United States.1 This number is expected to increase by 12% in the near future (through the year 2020), mostly due to the increases in the aging population of women in the United States.2 There are few evidence-based interventions available to reduce ovarian cancer mortality. Several organizations, including the Centers for Disease Control and Prevention (CDC), the National Institutes of Health, American College of Obstetricians and Gynecologists, the Society of Gynecologic Oncologists, and the National Comprehensive Cancer Network, support the recommendation of receiving treatment for ovarian cancer from a gynecologic oncologist due to the strong evidence associated with improved outcomes.3
Several studies have consistently demonstrated that gynecologic oncologists, subspecialists specifically trained to perform ovarian cancer surgical staging, debulking surgery, and administer chemotherapy, more often adhere to standard treatment recommendations resulting in increased survival from ovarian cancer.3–5 However, there is variable uptake of this recommendation, which may be due in part to the uneven distribution of these subspecialists across the United States and general lack of availability in rural areas where many ovarian cancer patients reside3,6 or lack of physician referral.7
OVA1, a diagnostic test that measures multiple biomarker expression, can help to determine the need for a gynecologic oncologist before a planned surgery when a woman presents with a suspicious mass. In a trial of almost 500 patients set to undergo surgery for an adnexal mass, OVA1 demonstrated higher sensitivity and a negative predictive value for ovarian malignancy compared to clinical impression and other blood marker (CA-125) measurements in a population of nongynecologic oncology practices.8 OVA1 generates a numeric result and categorizes patient risk of malignancy (high vs. low) stratified by menopausal status (pre vs. post). OVA1 has been approved for use in clinical practice since 2009 and has been validated for use by nongynecologic oncologists in several studies.8 However, the extent to which it is used by physicians to evaluate whether a patient needs to be referred to a gynecologic oncologist before surgery has not been measured.
In this study, we examine the knowledge of evidence-based recommendations for ovarian cancer mortality reduction in a population of primary care providers (family practitioners, internists, obstetrician/gynecologists). We surveyed these physicians about their referral patterns to gynecologic oncologists for ovarian cancer treatment and also knowledge of and about the OVA1 test that may be helpful for referrals to a gynecologic oncologist. This survey was undertaken as part of ongoing evaluation efforts of the CDC Inside Knowledge: Get the Facts About Gynecologic Cancer campaign. We discuss and comment on the results of this survey in the context of the CDC National Comprehensive Cancer Control Program (NCCCP). Specifically, we examine how the NCCCP activities are currently assisting with improving adherence to referral to gynecologic oncologist, eventually leading to a decrease in ovarian cancer mortality.
Methods
Porter Novelli’s 2012 DocStyles survey, an annual web-based survey of healthcare professionals conducted to gain insight into their attitudes and behaviors on a variety of health topics, was used to assess provider knowledge of evidence-based ovarian cancer mortality recommendations. Eligible participants were randomly sampled from the Epocrates Honors Panel, an opt-in, verified panel of over 275,000 physicians; this sample was drawn to match American Medical Association (AMA) master file proportions for age, gender, and region. Eligible participants included only those practicing in the United States; actively seeing patients; working in an individual, group, or hospital practice; and practicing for at least 3 years. A total of 2205 healthcare providers completed the survey. Respondents were paid between $20 and $85 for survey completion, depending on their specialty. The overall weighted response rate was 52.2% (55.2% for obstetrician/ gynecologists; 49.9% for family practitioners and internists).
Specific survey questions used were developed and commissioned as part of ongoing evaluation efforts of the CDC Inside Knowledge: Get the Facts About Gynecologic Cancer campaign. Additional information on healthcare provider demographics and practice information was also used as collected by Porter Novelli (e.g., age, gender, years in practice, group or independent practice).
Primary care providers (internists, family/general practitioner, and obstetrician/gynecologists [OB/GYNs]) were asked the following questions: (1) How often do you refer patients diagnosed with ovarian cancer to a gynecologic oncologist for staging and treatment? (Select one response option: never, rarely, some of the time, most of the time, always); (2) (asked among those who said they didn’t always refer to a gynecologic oncologist) What are the reasons you may not refer a patient diagnosed with ovarian cancer to a gynecologic oncologist? (Select all that apply: there are no gynecologic oncologists in the area in which my practice is located, I prefer to continue as the treating physician, the patient or patient’s family prefer that I continue as the treating physician, I refer the patient to another (non-gynecologic) oncology specialist, I refer the patient to a gynecologist, I refer the patient to another specialist, other; (3) Have you ever heard of the OVA1 test? (Select one response option: yes, no, not sure); (4) (asked among providers who responded they’d heard of OVA1) What is the OVA1 test used for? Select all that apply: To screen asymptomatic, average-risk patients for ovarian cancer, to determine whether a patient with an ovarian mass needs surgery, to help evaluate the malignancy of an ovarian mass before an already planned surgery, to determine if referral to a gynecologic oncologist is needed, to monitor patients previously treated for ovarian cancer, none of the above, not sure (italicized answers are the correct response).
CDC licensed the results of the 2012 DocStyles survey postcollection from Porter Novelli; institutional review board approval was not needed because CDC was not engaged in human subjects research. All analyses of data were done in SAS version 9.3 (SAS Institute, Inc., Cary, NC) and limited to those who classified themselves as primary care physicians (family/general practitioners, internists, and OB/ GYNs; n = 1251). A dichotomous variable was created for how often primary care physicians refer patients diagnosed with ovarian cancer to a gynecologic oncologist for staging and treatment (always vs. less than always).
We calculated descriptive statistics for demographic variables of interest by how often physicians refer patients diagnosed with ovarian cancer to a gynecologic oncologist, and we obtained p values from chi-square and t-tests. We examined frequency counts by provider type for reasons why patients are not routinely referred to gynecologic oncologists. Among physicians who were aware of the OVA1 test, we calculated frequency counts and percentages of correct and incorrect responses to a series of statements on the purpose of the test and we examined overall awareness of the OVA1 test by primary care physician specialty.
Results
Table 1 shows referral patterns of the primary care physicians by physician demographic and patient population information. Overall, 84% of respondents said they always referred patients diagnosed with an ovarian cancer to a gynecologic oncologist. The percentage was significantly higher for female compared to male physicians (89% vs. 82%, p = 0.001), non-Hispanic white and non-Hispanic black compared to Asian/Pacific Islander physicians (87%–88% vs. 75%, p < 0.0001), family/general practitioners compared to internists and OB/GYNs (87% vs. 81%, p = 0.01). Those physicians who said they always referred were in practice longer than those who indicated they did not always refer (16.6 years vs. 15.3 years, p = 0.05).
Table 1.
Referral to Gynecologic Oncologists by Primary Care Physician Characteristics
| Physician characteristic | How often do you refer patients diagnosed with ovarian cancer to a gynecologic oncologist for staging and treatment?
|
pa | ||
|---|---|---|---|---|
| Always, N (%) | Less than always, N (%) | Total, N (%) | ||
| Total | 1047 (84) | 204 (16) | 1251 (100) | |
| Gender | ||||
| Male | 718 (82) | 163 (18) | 881 (100) | 0.001 |
| Female | 329 (89) | 41 (11) | 370 (100) | |
| Age, years, mean | 47.4 | 45.4 | 47.1 | 0.006 |
| Race/ethnicity | ||||
| White (non-Hispanic) | 759 (87) | 117 (13) | 867 (100) | <0.0001 |
| Black (non-Hispanic) | 45 (88) | 6 (12) | 51 (100) | |
| Asian/Pacific Islander | 150 (75) | 50 (25) | 200 (100) | |
| Other race | 43 (67) | 21 (33) | 64 (100) | |
| Hispanic | 50 (83) | 10 (17) | 60 (100) | |
| Physician specialty | ||||
| Family/GP | 469 (87) | 68 (13) | 537 (100) | 0.01 |
| Internist | 375 (81) | 89 (19) | 464 (100) | |
| OB/GYN | 203 (81) | 47 (19) | 250 (100) | |
| Practice type | ||||
| Individual Outpatient | 212 (88) | 29 (12) | 241 (100) | 0.002 |
| Group outpatient | 756 (84) | 146 (16) | 902 (100) | |
| Inpatient | 79 (73) | 29 (27) | 108 (100) | |
| Patient population | ||||
| Very Poor | 47 (89) | 6 (11) | 53 (100) | 0.50 |
| Poor | 139 (85) | 24 (15) | 163 (100) | |
| Lower middle class | 406 (83) | 82 (17) | 488 (100) | |
| Middle class | 408 (84) | 78 (16) | 486 (100) | |
| Upper middle class | 47 (77) | 14 (23) | 61 (100) | |
| Years in practice, mean | 16.6 | 15.3 | 16.4 | 0.05 |
p Values comparing referral to gynecologic oncologists by demographic characteristics of providers are from chi-square tests for categorical variables, and t-tests for age and years in practice.
GP, general practitioner; OB/GYN, obstetrician/gynecologist.
Figure 1 shows reasons physicians who did not always refer to a gynecologic oncologist indicated for not doing so. The patient or patient’s family preferred that the physician continues as the treating physician (n =39), there are no gynecologic oncologist practices in my area (n =36), and referral to another (nongynecologic) oncology specialist (n =38) were all commonly cited reasons for lack of referral. Comparing physician specialty across these categories, OB/GYNs more often cited patient or family preference for treatment (n =19) as a reason, while family/general practitioners and internists more often cited referral to another oncology specialist (n =21). Relatively fewer physicians reported personally preferring to remain the treating physician as opposed to referral (n =19); however, almost half of physicians (n =9) who listed that response were OB/GYNs.
FIG. 1.
Reasons primary care physicians indicated for not referring to gynecologic oncologists. GP, general practitioner; OB/GYN, obstetrician/gynecologist; Gyn Onc, gynecologic oncologist.
Table 2 shows knowledge of the OVA1 test and its purpose. The majority (67%) of primary care physicians had not heard of the OVA1 test. Of those that heard of the test (n = 291), a little more than half (56%) correctly identified the appropriate use of the test (to help evaluate the malignancy of an ovarian mass before a planned surgery). A total of 40% of respondents also correctly identified that the test could determine if referral to a gynecologic oncologist is needed. Of note, about a third incorrectly identified the test as a screen for the asymptomatic average-risk population (29%), or a test used to determine if surgery is needed (30%). Another 12% incorrectly thought the test could be used to monitor patients who were previously treated for ovarian cancer.
Table 2.
Knowledge of OVA1 Test Among Primary Care Physicians
| What is the OVA1 test used for? Select all that applya | Selected, n (%) | Did not select, n (%) | ||
|---|---|---|---|---|
| Yes = 291 (23%) | To screen asymptomatic average-risk women | 83 (29) | 208 (71) | |
| To determine if an ovarian mass needs surgery | 86 (30) | 205 (70) | ||
| To help evaluate the malignancy of an ovarian mass before a planned surgery | 162 (56) | 129 (44) | ||
| Have you ever heard of the OVA1 test? | To determine if referral to a gyn onc is needed | 115 (40) | 176 (60) | |
| To monitor patients previously treated for ovarian cancer | 35 (12) | 256 (88) | ||
| No = 844 (67%) | N/A | |||
| Not sure = 116 (9%) | N/A | |||
Knowledge of OVA1 test use was asked only of those who indicated they heard of the test, as indicated in column 2 (n = 291). All response options to this question are listed, and the number of physicians who selected the response or did not select the response is indicated. The response options corresponding to the correct and appropriate use of OVA1 are italicized.
gyn onc, gynecologic oncologist; N/A, not applicable.
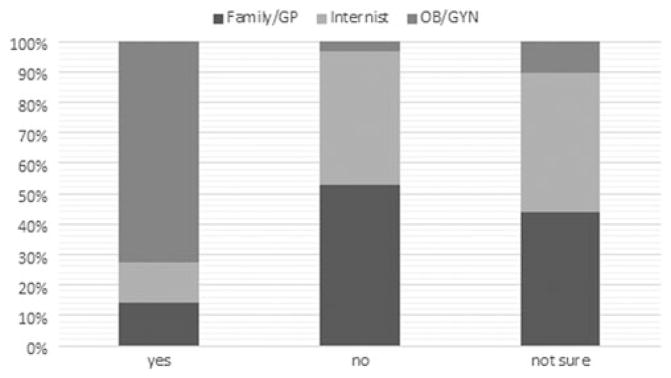
Figure 2 shows knowledge of the OVA1 test by physician specialty. The majority of physicians who had heard of the OVA1 test were OB/GYNs (72%). Almost all (97%) physicians who said they had not heard of OVA1 were family/ general practitioners or internists.
FIG. 2.
Knowledge of OVA1 test by primary care physician specialty. GP, general practitioner; OB/GYN, obstetrician/ gynecologist.
Discussion
Our findings indicate that over three-quarters of primary care physicians always refer patients diagnosed with ovarian cancer to gynecologic oncologists for staging and treatment, in line with current recommendations. This number is higher than that reported in a 2011 study, where 40%–50% of family physicians and internists and 66% of OB/GYNs reported referring to gynecologic oncologists.9 The increase could be due to wider dissemination and adoption of treatment recommendations in more recent years. We also found that there is a general lack of knowledge about the existence and purpose of the OVA1 test. This test would have the most utility among physicians who do not always refer to a gynecologic oncologist, and therefore, knowledge of it may be less important in this survey population, who largely indicated they always refer. Nevertheless, it remains an approved option for those physicians who need assistance in making the decision to refer to a gynecologic oncologist, and efforts to increase knowledge and use of OVA1 may improve appropriate referral rates to gynecologic oncologists.
While the large proportion of physicians reporting they would always refer is encouraging, actual receipt of treatment from a gynecologic oncologist is needed for ovarian cancer mortality reduction.3–5 Previous studies have reported variable and relatively lower percentages of patients receiving care from gynecologic oncologists than the referral rates reported here would suggest, ranging from 33%7 to 70% of ovarian cancer patients10; however, these percentages are from relatively older studies and more contemporary examinations may show improvement in treatment receipt, consistent with referral rates.
While this may be the case, geographic disparities in ovarian cancer care have been well documented,6,11–13 and these are likely to remain an issue for some ovarian cancer patients. A recent study in one urban National Cancer Institute-designated cancer center showed that the farther gynecologic cancer patients were required to travel to get to treatment (those traveling above 10, but less than 50 miles), the less likely they were to complete recommended care.13 Tele-medicine, which would allow gynecologic oncologists to consult on patient cases via phone- and/or videoconferencing, has been suggested to alleviate this disparity.3,14 However, this method has yet to be studied for its feasibility or utility in ovarian cancer. In addition, an inherent challenge exists in that ovarian cancer is a surgically managed disease and it is unknown whether providing remote surgical guidance would yield the same results as being the operating surgeon.14
The effect of patient or patient family preference on ovarian cancer treatment is also a factor in actual treatment receipt. While patient preference is not well studied in ovarian cancer, women have reported feeling unprepared, anxious, and confused after receiving an ovarian cancer diagnosis, and they are likely not aware of and/or may not be able to fully understand15 the survival advantage that gynecologic oncologists can offer them if it is explained at the time of diagnosis.
In general terms, several factors are thought to be considered by patients undergoing gynecologic surgery (not specifically for ovarian cancer treatment), including the preference for less invasive surgical methods if possible,16 fertility or estrogen preservation in premenopausal women,15,17 and the existence of complicating factors such as other concomitant diseases.15 For chemotherapy, women generally consider whether to enroll in a clinical trial,15,18 and the toxicity and side effects of drug regimens.15,18–20 For ovarian cancer specifically, women diagnosed with late-stage metastatic disease or those with significant comorbidities may prefer not to receive guideline-based treatment, as surgery may yield less than optimal results or may be harmful in certain circumstances. The type of treatment received is ultimately a patient or patient’s family choice; however, all physicians and healthcare providers can educate their patients on treatment options, harms, and benefits, so that informed decisions can be made.
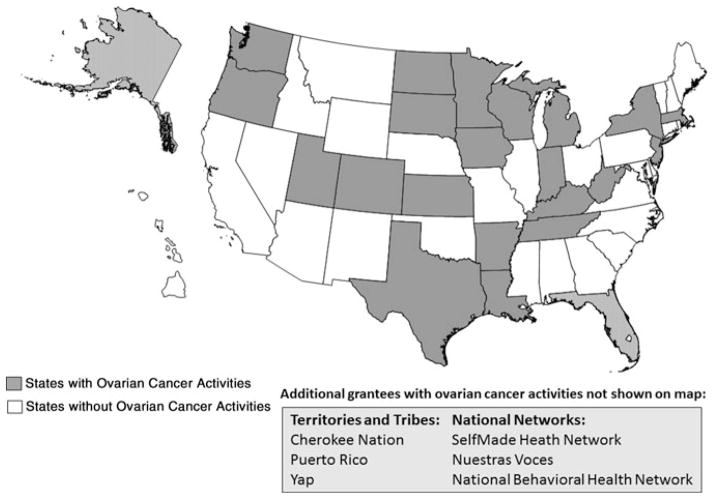
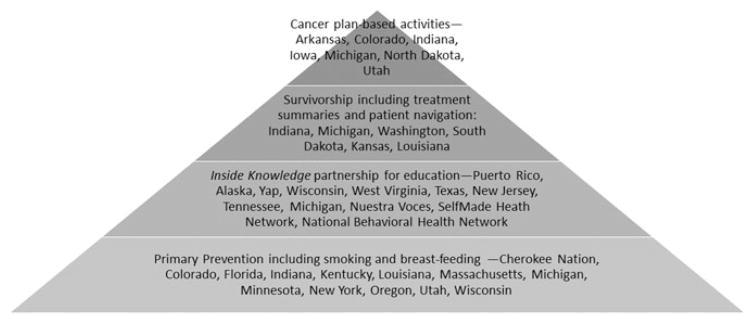
In addition to patient education by healthcare providers, public health efforts that educate and empower women to feel better able to navigate an ovarian cancer diagnosis and to make treatment decisions consistent with their preferences may assist with increased adherence to recommendations and may ultimately result in further reductions in ovarian cancer mortality. The CDC NCCCP operates in all 50 states, the District of Columbia, 7 tribal governments and organizations, and 7 territories and U.S.-associated Pacific Island jurisdictions to support the development and implementation of evidence-based initiatives to prevent and control cancer21 and is well positioned to be a leader in these public health efforts. Previous studies have documented prior ovarian cancer activities of the NCCCP, which largely centered on ovarian cancer survivor peer mentoring and provider education.10,22 Currently, 26 NCCCP-funded state, tribal, and territorial grantees, as well as three NCCCP-affiliated National Networks,23 carry out ovarian cancer activities (Fig. 3). The activities vary and range from ovarian cancer primary prevention to implementation of interventions to improve ovarian cancer survivors’ well-being (Fig. 4). Primary prevention activities include promoting smoking cessation and smoke-free environments, which may help prevent mucinous ovarian cancer and some serous ovarian tumors,24 as well as the promotion of breastfeeding among women who have the opportunity, which several studies have suggested may reduce risk for epithelial ovarian cancer.25–27
FIG. 3.
National Comprehensive Cancer Control Program grantees working in ovarian cancer.
FIG. 4.
Types of ovarian cancer activities being done by National Comprehensive Cancer Control Program grantees.
In addition, several NCCCP grantees have partnered with the CDC Inside Knowledge: Get the Facts about Gynecologic Cancer campaign to increase knowledge of other risk factors for and symptoms of ovarian cancer among the public and providers. A key message contained in Inside Knowledge materials is that if you are diagnosed with an ovarian cancer, get treatment from a gynecologic oncologist.28 Through these specific efforts, campaign materials are systematically distributed to diverse groups of women and providers across the country and knowledge changes are evaluated after facilitated educational discussions. The NCCCP has the unique ability to reach and effectively communicate with women in local communities, particularly those who do not have access to standard advertising methods (television, radio, public service announcements, and so on). Through the NCCCP/IK partnership, many women in traditionally medically under-served populations have been reached and educated directly, using methods that are culturally appropriate for them. For example, local community health workers and storytellers have participated in educational discussions to ensure better connection with participants and understanding of materials among Hispanic and American Indian/Alaska Native women, respectively. A particular strength of this NCCCP work is the enhanced outreach to disparate populations, including those that are Spanish speaking, those in the Pacific Island jurisdictions, and those that historically have experienced higher rates of cancer incidence and death.
Six NCCCP grantees are working to improve quality of life for those diagnosed with ovarian cancer. These grantees have undertaken efforts to provide survivor care plans to their populations diagnosed with cancer. Survivor care plans contain written descriptions of recommended and received treatment, and those diagnosed with cancer have reported high satisfaction with care plans and increased understanding of their treatment following care plan receipt.29 These same grantees are also developing patient navigation programs to assist cancer patients in seeking referrals and follow-up services, scheduling transportation to appointments, and improved communication with their providers among other activities.30 Studies have shown that patients who received both survivor care plans and patient navigation services were significantly more likely to attend all scheduled medical appointments, and this may translate into better quality of life and longer disease-free intervals among these patients.31
Finally, several grantees have included various initiatives in their ongoing cancer planning.32 These initiatives focus on improving public and provider knowledge of the role of family history in ovarian cancer and appropriate interventions for positive family history such as referral for genetic counseling and subsequent testing if appropriate.
While the ovarian cancer activities undertaken by NCCCP grantees are diverse, many grantees are directly addressing the evidence-based recommendation to receive care for ovarian cancer from a gynecologic oncologist. The ongoing education of the public about this recommendation before and at the time of diagnosis, and assistance of patients with communication and transportation needs following a diagnosis, could help increase the numbers of women receiving care from gynecologic oncologists following a diagnosis. To increase impact in this area, additional grantees can adopt these practices for their populations.
Conclusion
Ovarian cancer is a deadly disease, and treatment by a gynecologic oncologist is an evidence-based recommendation to decrease mortality from the disease. While many physicians indicate they always refer patients diagnosed with ovarian cancer to gynecologic oncologists, actual treatment receipt from these specialists may be dependent on a number of factors, including patient preferences for treatment, and ability of patients to travel to gynecologic oncologists practices. The CDC NCCCP is working to educate women about the benefits of and assist women with getting treatment from a gynecologic oncologist. All women, including those who have been newly diagnosed as well as those concerned about a future diagnosis, should be aware of the recommendations and options for receipt of the best and most appropriate care for them. Increased adoption of these types of awareness activities throughout the NCCCP may have substantial impact on ensuring adherence to this evidence-based recommendation.
Footnotes
Author Disclosure Statements
No competing financial interests exist.
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2012 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2015. [accessed on December 1, 2015]. Available at: www.cdc.gov/uscs. [Google Scholar]
- 2.Weir HK, Thompson TD, Soman A, Møller B, Leadbetter S, White MC. Meeting the healthy people 2020 objectives to reduce cancer mortality. Prev Chronic Dis. 2015;12:E104. doi: 10.5888/pcd12.140482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart SL, Rim SH, Richards TB. Gynecologic oncologists and ovarian cancer treatment: Avenues for improved survival. J Womens Health (Larchmt) 2011;20:1257–1260. doi: 10.1089/jwh.2011.3053. [DOI] [PubMed] [Google Scholar]
- 4.Cress RD, Bauer K, O’Malley CD, et al. Surgical staging of early stage epithelial ovarian cancer: Results from the CDC-NPCR ovarian patterns of care study. Gynecol Oncol. 2011;121:94–99. doi: 10.1016/j.ygyno.2010.12.359. [DOI] [PubMed] [Google Scholar]
- 5.Chan JK, Sherman AE, Kapp DS, et al. Influence of gynecologic oncologists on the survival of patients with endometrial cancer. J Clin Oncol. 2011;29:832–838. doi: 10.1200/JCO.2010.31.2124. [DOI] [PubMed] [Google Scholar]
- 6.Stewart SL, Cooney D, Hirsch S, et al. The effect of gynecologic oncologist availability on ovarian cancer mortality. World J Obstet Gynecol. 2014;3:71–77. doi: 10.5317/wjog.v3.i2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Earle CC, Schrag D, Neville BA, et al. Effect of surgeon specialty on processes of care and outcomes for ovarian cancer patients. J Natl Cancer Inst. 2006;98:172–180. doi: 10.1093/jnci/djj019. [DOI] [PubMed] [Google Scholar]
- 8.Bristow RE, Hodeib M, Smith A, et al. Impact of a multivariate index assay on referral patterns for surgical management of an adnexal mass. Am J Obstet Gynecol. 2013;209:581, e1–e8. doi: 10.1016/j.ajog.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Goff BA, Miller JW, Matthews B, et al. Involvement of gynecologic oncologists in the treatment of patients with a suspicious ovarian mass. Obstet Gynecol. 2011;118:854–862. doi: 10.1097/AOG.0b013e31822dabc6. [DOI] [PubMed] [Google Scholar]
- 10.Boyd LR, Novetsky AP, Curtin JP. Ovarian cancer care for the underserved: Are surgical patterns of care different in a public hospital setting? Cancer. 2011;117:777–783. doi: 10.1002/cncr.25490. [DOI] [PubMed] [Google Scholar]
- 11.Shalowitz DI, Vinograd AM, Giuntoli RL., 2nd Geographic access to gynecologic cancer care in the United States. Gynecol Oncol. 2015;138:115–120. doi: 10.1016/j.ygyno.2015.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Delva F, Soubeyran P, Rainfray M, Mathoulin-Pélissier S. Referral of elderly cancer patients to specialists: Action proposals for general practitioners. Cancer Treat Rev. 2012;38:935–941. doi: 10.1016/j.ctrv.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Temkin SM, Fleming SA, Amrane S, Schluterman N, Terplan M. Geographic disparities amongst patients with gynecologic malignancies at an urban NCI-designated cancer center. Gynecol Oncol. 2015;137:497–502. doi: 10.1016/j.ygyno.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Shalowitz DI, Smith AG, Bell MC, Gibb RK. Teleoncology for gynecologic cancers. Gynecol Oncol. 2015;139:172–177. doi: 10.1016/j.ygyno.2015.06.042. [DOI] [PubMed] [Google Scholar]
- 15.Ziebland S, Evans J, McPherson A. The choice is yours? How women with ovarian cancer make sense of treatment choices. Patient Educ Couns. 2006;62:361–367. doi: 10.1016/j.pec.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Geomini PM, Bremer GL, Kruitwagen RF, Opmeer BC, Mol BW. Patients’ preferences in mode of surgery of an adnexal mass. J Psychosom Obstet Gynaecol. 2009;30:162–167. doi: 10.1080/01674820903142259. [DOI] [PubMed] [Google Scholar]
- 17.Hershberger PE, Finnegan L, Pierce PF, Scoccia B. The decision-making process of young adult women with cancer who considered fertility cryopreservation. J Obstet Gynecol Neonatal Nurs. 2013;42:59–69. doi: 10.1111/j.1552-6909.2012.01426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minion LE, Coleman RL, Alvarez RD, Herzog TJ. Endpoints in clinical trials: What do patients consider important? A survey of the Ovarian Cancer National Alliance. Gynecol Oncol. 2016;140:193–198. doi: 10.1016/j.ygyno.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 19.Havrilesky LJ, Alvarez Secord A, Ehrisman JA, et al. Patient preferences in advanced or recurrent ovarian cancer. Cancer. 2014;120:3651–3659. doi: 10.1002/cncr.28940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun CC, Bodurka DC, Donato ML, et al. Patient preferences regarding side effects of chemotherapy for ovarian cancer: Do they change over time? Gynecol Oncol. 2002;87:118–128. doi: 10.1006/gyno.2002.6807. [DOI] [PubMed] [Google Scholar]
- 21.Major A, Stewart SL. Celebrating 10 years of the National Comprehensive Cancer Control Program, 1998 to 2008. Prev Chronic Dis. 2009;6:A133. [PMC free article] [PubMed] [Google Scholar]
- 22.Stewart SL, Lakhani N, Brown PM, Larkin OA, Moore AR, Hayes NS. Gynecologic cancer prevention and control in the National Comprehensive Cancer Control Program: Progress, current activities, and future directions. J Womens Health (Larchmt) 2013;22:651–657. doi: 10.1089/jwh.2013.4465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC. [accessed December 18, 2015];Consortium of national networks to impact populations experiencing tobacco-related and cancer health disparities. Available at http://www.cdc.gov/tobacco/about/coop-agreements/national-networks.
- 24.Faber MT, Kjær SK, Dehlendorff C, et al. Cigarette smoking and risk of ovarian cancer: A pooled analysis of 21 case-control studies. Cancer Causes Control. 2013;24:989–1004. doi: 10.1007/s10552-013-0174-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-feeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2012;23:919–927. doi: 10.1007/s10552-012-9963-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luan NN, Wu QJ, Gong TT, Vogtmann E, Wang YL, Lin B. Breastfeeding and ovarian cancer risk: A meta-analysis of epidemiologic studies. Am J Clin Nutr. 2013;98:1020–1031. doi: 10.3945/ajcn.113.062794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li DP, Du C, Zhang ZM, et al. Breastfeeding and ovarian cancer risk: A systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev. 2014;15:4829–4837. doi: 10.7314/apjcp.2014.15.12.4829. [DOI] [PubMed] [Google Scholar]
- 28.Rim SH, Polonec L, Stewart SL, Gelb CA. A national initiative for women and healthcare providers: CDC’s Inside Knowledge: Get the Facts About Gynecologic Cancer campaign. J Womens Health (Larchmt) 2011;20:1579–1585. doi: 10.1089/jwh.2011.3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brennan ME, Gormally JF, Butow P, Boyle FM, Spillane AJ. Survivorship care plans in cancer: A systematic review of care plan outcomes. Br J Cancer. 2014;111:1899–1908. doi: 10.1038/bjc.2014.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palos GR, Hare M. Patients, family caregivers, and patient navigators: A partnership approach. Cancer. 2011;117(15 Suppl):3592–3602. doi: 10.1002/cncr.26263. [DOI] [PubMed] [Google Scholar]
- 31.Jabson JM. Treatment summaries, follow-up care instructions, and patient navigation: Could they be combined to improve cancer survivor’s receipt of follow-up care? J Cancer Surviv. 2015;9:692–698. doi: 10.1007/s11764-015-0444-0. [DOI] [PubMed] [Google Scholar]
- 32.CDC. [accessed December 18, 2015];Comprehensive cancer control plans. Available at: http://www.cdc.gov/cancer/ncccp/ccc_plans.htm.