Abstract
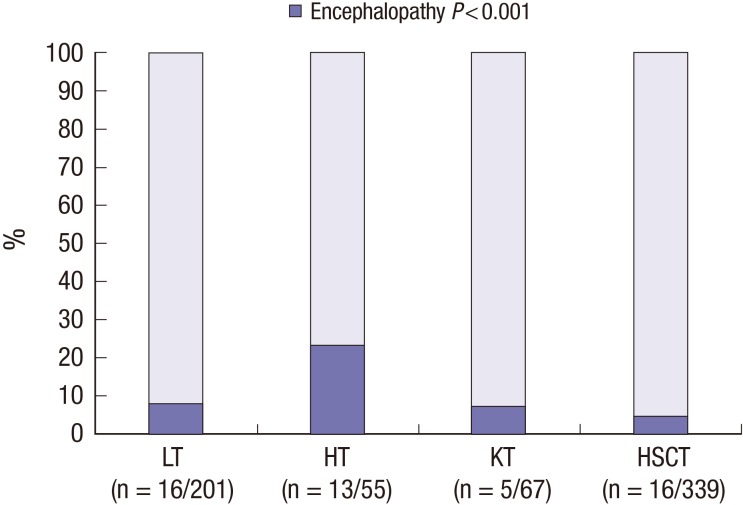
We aimed to analyze characteristics of encephalopathy after both hematopoietic stem cell and solid organ pediatric transplantation. We retrospectively reviewed medical records of 662 pediatric transplant recipients (201 with liver transplantation [LT], 55 with heart transplantation [HT], and 67 with kidney transplantation [KT], 339 with allogeneic hematopoietic stem cell transplantation [HSCT]) who received their graft organs at Asan Medical Center between January 2000 and July 2014. Of the 662 patients, 50 (7.6%) experienced encephalopathy after transplantation. The incidence of encephalopathy was significantly different according to the type of organ transplant: LT, 16/201 (8.0%), HT, 13/55 (23.6%), KT, 5/67 (7.5%), and HSCT, 16/339 (4.7%) (P < 0.001). Drug-induced encephalopathy (n = 14) was the most common encephalopathy for all transplant types, but particularly after HSCT. Hypertensive encephalopathy was the most common after KT and HT, whereas metabolic encephalopathy was the most common after LT. The median time to encephalopathy onset also differed according to the transplant type: 5 days after KT (range 0–491 days), 10 days after HT (1–296 days), 49.5 days after HSCT (9–1,405 days), and 39 days after LT (1–1,092 days) (P = 0.018). The mortality rate among patients with encephalopathy was 42.0% (n = 21/50). Only 5 patients died of neurologic complications. Transplant-associated encephalopathy presented different characteristics according to the type of transplant. Specialized diagnostic approach for neurologic complications specific to the type of transplant may improve survival and quality of life in children after transplantation.
Keywords: Encephalopathy, Transplantation, Liver, Kidney, Heart, Hematopoietic Stem Cells
Graphical Abstract
INTRODUCTION
Solid organ and hematopoietic stem cell transplantation (HSCT) have been performed increasingly as a therapeutic modality for end-stage organ failure, a variety of hematologic disorders, and non-malignancy disease. Solid organ transplants performed in the United States in 2015 exceeded 30,000 and continued to increase (1). Although remarkable advances in transplantation medicine improved the outcomes of allogeneic graft recipients, neurologic complications are still common with variety incidence ranging from 7% to 77% of allograft recipients after HSCT and solid or gan transplantation (2,3,4,5,6,7,8,9,10,11,12). One of the most deleterious neurologic complications is transplant-associated encephalopathy, which has various etiologies, including the underlying disorder motivating the transplant, immunosuppressant neurotoxicity, metabolic derangement, central nervous system (CNS) infection, and stroke (9,12,13,14,15). As the surgical procedure, intensity of immunosuppression, infection prophylaxis regimen, underlying neurologic symptoms, and recipient's age vary according to the type of transplant, the presentation of the encephalopathy may differ according to the specific type of organs transplanted.
To help shape neurological care in pediatric transplantation, we investigated the overall incidence, etiologies and clinical course of encephalopathy after allogeneic HSCT and solid organ transplantation in pediatric patients from a single tertiary center in Korea. In addition, we dissected the differences among the transplant types to identify the best peritransplant care approach after transplantation from a neurological perspective.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of all patients younger than 18 years at the time of transplantation who received a transplant, including allogeneic hematopoietic stem cell, kidney, heart, and liver transplantation (LT), between January 2000 and July 2014 at Asan Medical Center Children's Hospital, a single tertiary center in Korea. Before identifying patients with encephalopathy after transplantation, we excluded patients who underwent autologous HSCT or 2 or more organ transplants at the same time. Encephalopathy was defined as any altered level of consciousness or newly developed brain dysfunction, such as seizures, tremors, visual problems, or personality changes, after transplantation that was not caused by sedative medication. We intended to exclude neurologic deterioration not directly associated with transplantation procedures, preexisting CNS manifestations associated with CNS involvement of underlying disease, such as leukemic or lymphohistiocytosis infiltration into the CNS and hepatic encephalopathy persistent after transplantation, was excluded from the study. The following data were collected from the medical records: patient characteristics, underlying disease, preoperative neurologic symptoms, the etiologies of encephalopathy, encephalopathy onset time, clinical course, and survival after transplantation. Neurological examinations, neuroimaging, laboratory studies (blood count, coagulation profile, electrolyte, chemistry, serum trough level of immunosuppressants, cerebrospinal fluid analysis, microbiological studies), and electroencephalography findings at the time of events were also reviewed by 2 pediatric neurologists (LYJ, YMS). The etiology of the encephalopathy was determined by reviewing clinical history and symptoms and microbiological, electrophysiological, and radiological characteristics. Encephalopathies were categorized into 6 groups: drug-induced, hypertensive, anoxic, metabolic, CNS infection-associated, and unknown etiology. Drug-induced encephalopathy was defined as an acute encephalopathy temporally related to the administration of any drugs, such as immunosuppressant, chemotherapeutic, and antibiologic agents, that resolved after withdrawal of the drug and based on exclusion of other causes. Identification of immunosuppressant related encephalopathy was supported in case of high serum trough level of immunosuppressant (e.g., tacrolimus > 15 ng/mL or cyclosporine > 400 ng/mL) at that time of neurologic complications without any other causes. Hypertensive encephalopathy was defined as encephalopathy in the presence of pronounced hypertension. When encephalopathy is caused by hypertension secondary to immunosuppressant, the patient is defined as drug-induced encephalopathy. Anoxic encephalopathy was defined as acute symptoms of cerebral perfusion reduction, including ischemic stroke or intracranial hemorrhage (ICH). Metabolic encephalopathy was defined as encephalopathy that developed with the occurrence of renal failure, liver failure, or electrolyte and glucose imbalance. CNS infection-associated encephalopathy was diagnosed by positive identification of a pathogen from the cerebrospinal fluid, blood, or tissue pathology and/or a cerebrospinal fluid finding compatible with infection. Posterior reversible encephalopathy syndrome (PRES) was defined as an independent clinicoradiological entity involving a posterior lesion in the cerebral hemisphere and characterized by altered consciousness, cortical blindness, and/or convulsion (16).
Statistical analysis
Group differences according to the transplanted organ were assessed by the χ2 test or Fisher's exact test for categorical variables and the Kruskal-Wallis test for continuous variables, followed by post hoc testing. All tests of significance were 2-sided, with a significance level of P < 0.05. For multiple comparisons, the significance level was corrected for the number of comparisons by the Bonferroni method (Bonferroni-adjusted P < 0.008). All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Asan Medical Center (Registry No. 20150724). Informed consent was waived by the board.
RESULTS
Patient characteristics and incidence of encephalopathy
From January 2000 through July 2014, 662 pediatric patients underwent organ transplantation at Asan Medical Center Children's Hospital: LT in 201 patients, kidney transplantation (KT) in 67, heart transplantation (HT) in 55, and allogeneic HSCT in 339. Of the 662 patients, 50 (7.6%) developed encephalopathy after transplantation at a mean ± standard deviation follow-up of 53.1 ± 46.6 months: 16 of 201 LT recipients (8.0%), 13 of 55 HT recipients (23.6%), 5 of 67 KT recipients (7.5%), and 16 of 339 allogeneic HSCT recipients (4.7%) (Fig. 1). The incidence of encephalopathy was significantly different according to the type of organ transplant (P < 0.001). We compared the characteristics of the patients with encephalopathy according to the type of transplant (Table 1). The median age at the time of transplantation (P < 0.001) and presence of preoperative neurologic symptoms (P = 0.002) differed according to the encephalopathy group. LT patients (n = 8, 50.0%) were the most likely to show preoperative neurologic symptoms, followed by HT patients (n = 4, 28.6%). The median encephalopathy onset time was significantly different according to the transplanted organ (P = 0.018). Encephalopathy tended to occur in the early postoperative period after KT and HT, whereas it occurred in the late postoperative period after allogeneic HSCT and LT. The encephalopathy onset time was significantly different between HSCT and HT patients (P = 0.002).
Fig. 1.
The incidence of encephalopathy according to the type of organ transplant.
LT = liver transplantation, HT = heart transplantation, KT = kidney transplantation, HSCT = hematopoietic stem cell transplantation.
Table 1. Characteristics of the patients with encephalopathy.
| Characteristics | LT (n = 16) | HT (n = 13) | KT (n = 5) | HSCT (n = 16) | P value |
|---|---|---|---|---|---|
| Age, yr | 1.4 (0.5–11.0)*,†,‡ | 8.4 (0.7–17.2)† | 14.4 (10.3–15.1)‡ | 6.3 (1.2–15.8)* | < 0.001§ |
| Male sex | 8 (50.0) | 7 (53.8) | 4 (80.0) | 9 (56.3) | 0.558 |
| Follow-up duration, mon | 36.4 (1.0–116.0) | 52.7 (1.0–137.0) | 119.8 (19.0–143.0) | 37.1 (0.3–129.1) | 0.178 |
| Preoperative neurologic symptom | 8 (50.0)* | 4 (28.6) | 0 (0.0) | 0 (0.0)* | 0.002§ |
| Onset time of encephalopathy, day | 39 (1–1,092) | 10 (1–296)∥ | 5 (0–491) | 49.5 (9–1,405)∥ | 0.018§ |
Values are presented as number (%) or median (range).
LT = liver transplantation, HT = heart transplantation, KT = kidney transplantation, HSCT = hematopoietic stem cell transplantation.
*P = 0.002, comparison of the HSCT group with the LT group; †P = 0.001, comparison of the LT group with the HT group; ‡P = 0.002, comparison of the LT group with the KT group; §P < 0.05; ‖P = 0.002, comparison of the HSCT group with the HT group.
Etiology of encephalopathy
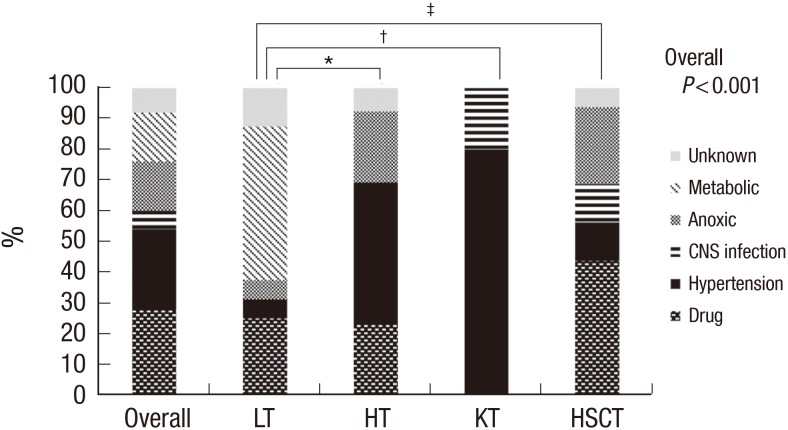
In all 50 patients with encephalopathy, the most common etiology was drug-induced encephalopathy (n = 14, 28.0%) (Fig. 2). The distribution of etiologies was significantly different according to the type of transplant (P < 0.001). Post hoc analysis indicated that the distribution of etiologies was significantly different in HSCT, HT, and KT from LT. The most prevalent etiology of encephalopathy differed according to the type of transplant: metabolic encephalopathy in LT (n = 8), hypertensive encephalopathy in KT (n = 4) and HT (n = 6), and drug-induced encephalopathy in allogeneic HSCT (n = 7).
Fig. 2.
The etiology of encephalopathy according to the type of organ transplant.
LT = liver transplantation, HT = heart transplantation, KT = kidney transplantation, HSCT = hematopoietic stem cell transplantation, CNS = central nervous system.
*P = 0.006; †P = 0.004; ‡P = 0.002.
Organ-specific encephalopathy
Liver transplantation
Sixteen patients developed encephalopathy after LT at a median follow-up of 36.4 months (range 1–116 months) after the transplantation (Table 2). The most common etiology was metabolic encephalopathy (n = 8), followed by drug-induced encephalopathy (n = 4). Of the 8 patients with metabolic encephalopathy, 7 had hepatic encephalopathy, 5 of whom died because of graft failure. All 4 patients with drug-induced encephalopathy presented with a toxic serum concentration of immunosuppressant and elevated blood pressure. One patient (patient 10), who had citrullinemia, Epstein-Barr virus (EBV)-associated post-transplant lymphoproliferative disorder (PTLD) and coagulopathy developed ICH around 3 years after transplantation and died of brain herniation.
Table 2. Patients with encephalopathy after LT (n = 16/201).
| Pt. No. | Sex/Age, yr | Diagnosis | Neurologic symptom | NC onset, day | Etiology | MRI/CT | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1 | M/0.8 | BA | Seizure | 422 | Metabolic | Hypoglycemia (glucose 9 mg/dL) | N | Alive |
| 2 | F/0.6 | BA | Mental change | 20 | Metabolic | HE | - | Death (liver failure) |
| 3 | F/1.8 | BA | Mental change | 184 | Metabolic | HE | - | Death (liver failure) |
| 4 | F/8.0 | BA | Mental change | 124 | Metabolic | HE | - | Death (liver failure) |
| 5 | M/0.9 | BA | Mental change | 1 | Metabolic | HE | Diffuse brain edema | Alive, epilepsy |
| 6 | M/0.8 | ALF | Mental change, seizure | 79 | Metabolic | HE | - | Death (liver failure) |
| 7 | F/1.4 | ALF | Mental change, seizure | 14 | Metabolic | HE | Diffuse brain edema | Death (liver failure) |
| 8 | M/0.5 | ALF | Mental change | 27 | Metabolic | HE | Diffuse T2 HSI WM | Alive, epilepsy |
| 9 | F/11.0 | Budd-Chiari syndrome | Seizure | 51 | HTN | BP 160/110 mmHg | Frontal hypodensity | Alive |
| 10 | F/2.8 | Citrullinemia | Mental change | 1,092 | Anoxic | ICH | ICH, brainherniation | Death (ICH) |
| 11 | M/5.0 | BA | Mental change, tremor | 59 | Drug | FK506 16.9 ng/mL | N | Alive |
| BP 155/80 mmHg | ||||||||
| 12 | F/4.0 | Alagille syndrome | Seizure | 16 | Drug | FK506 32.2 ng/mL | Multifocal calcification | Death (GI bleeding) |
| BP 160/100 mmHg | ||||||||
| 13 | M/2.0 | PFIC type 1 | Mental change | 5 | Drug | FK506 23 ng/mL | Mild ventriculomegaly | Alive |
| BP 133/53 mmHg | ||||||||
| 14 | F/1.4 | Factor X deficiency | Seizure | 3 | Drug | FK506 30.3 ng/mL | Encephalomalacia | Alive |
| BP 118/80 mmHg | ||||||||
| 15 | M/0.8 | ALF | Seizure | 100 | Unknown | - | Alive | |
| 16 | F/0.8 | BA | Seizure | 22 | Unknown | - | Alive | |
LT = liver transplantation, NC = neurologic complication, MRI = magnetic resonance imaging, CT = computed tomography, BA = biliary atresia, N = no abnormality, HE = hepatic encephalopathy, ALF = acute liver failure, HSI = high signal intensity, BP = blood pressure, WM = white matter, HTN = hypertensive, ICH = intracranial hemorrhage, FK506 = tacrolimus, GI = gastrointestinal, PFIC = progressive familial intrahepatic cholestasis.
Heart transplantation
Thirteen patients (7 males) were identified as having encephalopathy at a median follow-up of 52.7 months (range 1–137 months) after transplantation (Table 3). The most common encephalopathy in HT patients was hypertensive encephalopathy (n = 6), followed by anoxic encephalopathy (n = 3) and drug-induced encephalopathy (n = 3). Cardiopulmonary resuscitation events occurred in 4 patients (3 in hypertension encephalopathy, 1 in anoxic encephalopathy) and extracorporeal membrane oxygenation (ECMO) insertion in 1 patient with anoxic encephalopathy before neurologic symptom onset. Except for 1 patient with ICH, the 12 other encephalopathic events developed within 2 months after transplantation. In particular, 5 cases of hypertensive encephalopathy and 2 cases of ischemic encephalopathy occurred within 2 weeks after transplantation. Three patients with hypertension (patient 2, 7, and 9) were diagnosed with PRES and 2 of them (patient 7 and 9) also had calcineurin inhibitor neurotoxicity. One patient, who was taking anticoagulant medication after surgical repair of an aortic aneurysm, developed abnormal coagulation function resulting in ICH and died of ICH.
Table 3. Patients with encephalopathy after HT (n = 13/55).
| Pt. No. | Sex/Age, yr | Diagnosis | Neurologic symptom | NC onset, day | CPR/ECMO | Etiology | MRI/CT | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/3.1 | DCMP | Seizure, mental change | 30 | −/− | HTN | BP 147/97 mmHg | Small SDH | Death (HF) |
| 2 | F/0.7 | DCMP | seizure, mental change | 1 | +/− | HTN | BP 150/78 mmHg | PRES | Alive, epilepsy |
| 3 | F/7.8 | DCMP | Mental change, seizure | 7 | −/− | HTN | BP 149/99 mmHg | Mild diffuse brain atrophy | Alive |
| 4 | M/3.5 | HF | Mental change, seizure | 10 | +/− | HTN | BP 170/90 mmHg | Multiple calcification | Alive, mental retardation |
| 5 | F/3.1 | DCMP | Mental change | 11 | +/− | HTN | BP 170/85 mmHg | N | Alive |
| 6 | M/11.0 | DCMP | Seizure | 5 | −/− | HTN | BP 150/96 mmHg | - | Alive |
| 7 | M/8.4 | RCMP | Seizure, mental change, visual impairment | 28 | −/− | Drug | FK506 13.6 ng/mL BP 135/85 mmHg |
PRES | Alive |
| 8 | M/7.5 | RCMP | Seizure, mental change | 11 | −/− | Drug | FK506 5.6 ng/mL BP 105/69 mmHg |
Small SDH | Alive |
| 9 | M/12.9 | HCMP | Seizure, mental change, psychosis | 59 | −/− | Drug | CsA 1,699 ng/mL BP 136/82 mmHg |
PRES | Alive |
| 10 | F/11.2 | HF | Seizure, mental change, delirium | 1 | −/− | Anoxic | - | Diffuse hypodensity | Alive |
| 11 | F/14.1 | RCMP | Mental change | 4 | −/+ | Anoxic | - | Bilateral putaminal T2 HSI | Death |
| 12 | M/12.6 | DCMP | Mental change | 296 | +/− | Anoxic | ICH | ICH, herniation | Death (ICH) |
| 13 | M/17.2 | HCMP | Mental change | 6 | −/− | Unknown | - | Small SDH | Death (HF) |
HT = heart transplantation, NC = neurologic complication, CPR = cardiopulmonary resuscitation, ECMO = extracorporeal membrane oxygenation, MRI = magnetic resonance imaging, CT = computed tomography, DCMP = dilated cardiomyopathy, HTN = hypertensive, BP = blood pressure, SDH = subdural hemorrhage, HF = heart failure, HCMP = hypertrophic cardiomyopathy, CsA = cyclosporine, PRES = posterior reversible encephalopathy syndrome, N = no abnormality, FK506 = tacrolimus, RCMP = restrictive cardiomyopathy, HSI = high signal intensity, ICH = intracranial hemorrhage.
Kidney transplantation
Five patients developed encephalopathy after KT (Table 4). Hypertensive encephalopathy developed in 4 patients within 7 days after transplantation. Neuroimaging revealed typical white matter lesionson the occipital lobe that were consistent with PRES in 2 patients with hypertensive encephalopathy (patient 2 and 4). One patient (patient 5) presented with mental change, seizure, headache, and fever and was diagnosed with EBV encephalitis 1 year after transplantation and finally with CNS PTLD.
Table 4. Patients with encephalopathy after KT (n = 5/67).
| Pt. No. | Sex/Age, yr | Diagnosis | Neurologic symptom | NC onset, day | Etiology | MRI/CT | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1 | M/10.3 | Reflux nephropathy | Mental change | 38 | HTN | BP 150/90 mmHg | N | Alive |
| 2 | M/14.4 | Reflux nephropathy | Seizure | 0 | HTN | BP 180/90 mmHg | PRES | Alive |
| 3 | F/15.1 | Henoch-Schönlein nephritis | Seizure | 1 | HTN | BP 180/110 mmHg | - | Alive |
| 4 | M/15.0 | Chronic renal failure, unknown etiology | Seizure | 5 | HTN | BP 179/110 mmHg | PRES | Alive |
| 5 | M/10.6 | Bilateral dysplastic kidney | Fever, mental change | 491 | CNS infection | EBV encephalitis → PTLD | Multifocal enhancing T2 HSI | Alive |
KT = kidney transplantation, NC = neurologic complication, MRI = magnetic resonance imaging, CT = computed tomography, HTN = hypertensive, BP = blood pressure, N = no abnormality, PRES = posterior reversible encephalopathy syndrome, CNS = central nervous system, EBV = Epstein-Barr virus, PTLD = post-transplant lymphoproliferative disorder, HSI = high signal intensity.
Hematopoietic stem cell transplantation
Encephalopathy occurred in 16 patients (9 males) at a median follow-up of 37.1 months (range 0.3–129.1 months) after allogeneic HSCT (Table 5). Except for 1 patient with a full-matched related donor transplant, 15 patients underwent HSCT from anunrelated donor. The most common etiology was drug-induced encephalopathy (n = 7), followed by anoxic encephalopathy (n = 4). Three patients with calcineurin inhibitor neurotoxicity (patient 2, 5, and 6) presented coexisting hypertension during neurologic symptoms and 2 of them (patient 2 and 6) were diagnosed with PRES and recovered without any residual neurologic deficit. One patient who had chronic lung graft versus host disease (GVHD) (patient 8) presented with anoxic encephalopathy after cardiopulmonary resuscitation and application of ECMO due to respiratory failure. Two patients were diagnosed with CNS infection and one of them was confirmed as having aspergillosis. Two patients with ICH had thrombocytopenia, and in one of them, CNS infection developed before hemorrhage. Two with ICH and one with meningoencephalitis died because of their neurologic symptom.
Table 5. Patients with encephalopathy after allogeneic HSCT (n = 16/339).
| Pt. No. | Sex/Age, yr | Diagnosis | Donor type | Neurologic symptom | NC onset, day | Etiology | MRI/CT | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/14.6 | AML | URD | Mental change | 523 | Drug | FK506 - | Multifocal WM T2 HSI | Death (MOF) |
| BP 138/86 mmHg | |||||||||
| 2 | M/4.6 | FA | URD | Mental change, seizure | 91 | Drug | FK506 26 ng/mL | PRES | Alive |
| BP 150/90 mmHg | |||||||||
| 3 | F/12.2 | FA | URD | Seizure | 34 | Drug | CsA 439 ng/mL | Multifocal WM T2 HSI | Alive |
| BP 137/86 mmHg | |||||||||
| 4 | F/2.2 | AML | URD | Mental change, seizure | 22 | Drug | CsA 302 ng/mL | - | Death (septic shock) |
| BP 140/90 mmHg | |||||||||
| 5 | M/1.2 | ALL | URD | Mental change, seizure | 29 | Drug | CsA 249 ng/mL | N | Death (asphyxia) |
| BP 160/100 mmHg | |||||||||
| 6 | M/5.7 | CML | MRD | Blurred vision, seizure,mental change | 677 | Drug | CsA 312 ng/mL | PRES | Alive |
| BP 160/110 mmHg | |||||||||
| 7 | M/15.5 | AML | URD | Visual disturbance, memory loss | 690 | Drug | Chemotherapy/RT | Multifocal T2 HSI | Death (asphyxia) |
| BP 92/61 mmHg | |||||||||
| 8 | F/6.9 | ALL | URD | Seizure | 1405 | Anoxic | cGVHD related | - | Death (septic shock) |
| 9 | F/4.4 | AML | URD | Mental change, seizure | 23 | Anoxic | - | Multifocal T2 HSI | Alive, quadriparesis |
| 10 | F/9.0 | AA | URD | Mental change | 154 | Anoxic | ICH | ICH, SDH | Death (ICH) |
| 11 | F/1.2 | ALL | URD | Mental change | 9 | Anoxic | - | Diffuse atrophy | Death (septic shock) |
| 12 | M/15.8 | ALL | URD | Mental change | 258 | CNS infection | Meningoencephalitis | Multifocal FLAIR HSI, gyral swelling | Death (CNS infection) |
| 13 | M/13.8 | MDS | URD | Mental change | 42 | CNS infection | Fungal abscess | Multiple abscess | Death (ICH) |
| 14 | M/4.6 | AA | URD | Mental change, seizure | 18 | HTN | BP 150/90 mmHg | N | Alive, epilepsy |
| 15 | M/7.2 | AML | URD | Mental change | 57 | HTN | BP 138/83 mmHg | N | Alive, epilepsy |
| 16 | M/2.1 | TLL | URD | Mental change, seizure | 12 | Unknown | - | N | Death (MOF) |
HSCT = hematopoietic stem cell transplantation, NC = neurologic complication, MRI = magnetic resonance imaging, CT = computed tomography, URD = unrelated donor, FK506 = tacrolimus, BP = blood pressure, WM = white matter, HSI = high signal intensity, MOF = multi-organ failure, FA = Fanconi anemia, PRES = posterior reversible encephalopathy syndrome, AML = acute myeloid leukemia, CsA = cyclosporine, ALL = acute lymphoblastic leukemia, CML = chronic myeloid leukemia, cGVHD = chronic graft versus host disease, ICH = intracranial hemorrhage, AA = aplastic anemia , SDH = subdural hemorrhage, CNS = central nervous system, FLAIR = fluid-attenuated inversion recovery, N = no abnormality, TLL = T-cell acute lymphoblastic leukemia.
Outcome of encephalopathy
Of the 50 patients with encephalopathy, 21 (42.0%) died. The mortality rate was 62.5% in allogeneic HSCT patients (n = 10), 43.8% in LT patients (n = 7), 30.8% in HT patients (n = 4) and 0.0% in KT patients (P = 0.070, between 4 groups). Five patients died of neurologic complications, including ICH (2 in the allogeneic HSCT group, 1 in the HT, 1 in the LT) and meningoencephalitis (1 in the allogeneic HSCT group). All patients with ICH presented coagulopathy, or thrombocytopenia and one had coexisting CNS infection at that time of neurologic symptom. The remaining 16 patients died of other transplant-related causes; graft failure, multi-organ failure, septic shock, pulmonary hemorrhage, and gastrointestinal bleeding. Of the 29 surviving patients, there were residual neurologic symptoms in 7 patients (24.1%) after transplantation. Residual neurologic deficits included epilepsy, quadriparesis, dysphagia, and cognitive impairment. All 7 patients with PRES completely recovered from their neurologic symptoms, except for 1 who hadepilepsy before HT.
DISCUSSION
This is the first study to compare the characteristics of encephalopathy according to the type of organ transplant from a neurological perspective. In this study, transplant-associated encephalopathy was common after pediatric solid organ transplantations and allogeneic HSCTs. Previous studies (2,3,4,5,6,7,8,9,10,11,12) reported an estimated incidence of transplant-related neurologic complications that ranged from 7% to 77% according to the type of organ studied and the population. As we disregarded other neurological problems, we cannot directly compare the incidence of encephalopathy with previous studies reporting the overall incidence of neurologic complications.
We also showed that the incidence, etiologies and characteristics of encephalopathy differ according to the type of organ transplant. In our study population, the incidence of transplant-related encephalopathy was highest for HT (13/55, 23.6%), followed by LT (16/201, 8.0%), KT (5/67, 7.5%), and allogeneic HSCT (16/339, 4.7%). Highest incidence of encephalopathy in HT is probably due to multi-factorial risk factors during pre- and post-transplant period. As previous reports, cardiac arrest, prolonged cardiopulmonary bypass, use of anticoagulants, complications of cardiac catheterization, microemboli during intraoperative period, and hemodynamic instability during peritransplant period may lead the HT recipients to be vulnerable to neurologic complications (11,17,18). Furthermore, long-standing cerebral hypoperfusion caused by underlying heart disease can increase an intrinsic risk for neurologic complications such as anoxic and hypertensive encephalopathy (19,20,21,22,23). In other organ transplantations, previous reports suggested that patients with preexisting neurologic impairment caused by chronic organ failure have predisposing factors that lead to neurologic complications after transplantation (5,24,25,26). In an analysis of 101 LT recipients, preoperative hepatic encephalopathy was suggested to be the strongest predictive factor associated with neurologic complications (25). In another analysis of brain magnetic resonance imaging of KT and LT recipients, various neuroradiological findings, including brain atrophy, venous thrombosis, white matter change, and ICH, were seen to be secondary to chronic liver disease and end stage renal disease (24). Preexisting neurologic impairment due to chemotherapy and radiation induced neurotoxicity, opportunistic infections, or ICH before transplantation were also prevalent in HSCT candidates (27,28). In our study, the prevalence of pre-transplantation neurologic symptoms was significantly different according to the type of organ transplant, with symptoms most commonly seen in LT recipients (3 hepatic encephalopathy, 5 epilepsy, 1 ICH), followed by HT recipients (2 ischemic stroke, 1 delirium, 1 epilepsy). This high prevalence of preexisting neurological problems in HT and LT can be the another cause of the higher incidence of post-transplant neurological complications.
Our results showed that the attributable etiologies of encephalopathy were significantly different according to the type of organ transplant. The incidence of hypertensive encephalopathy was particularly high in KT (4/5, 80.0%) and HT (6/13, 46.2%) recipients, similar to previous studies (3,11,15). Both calcineurin inhibitor and hemodynamic instability have been reported to be decisive factors for hypertensive encephalopathy in KT and HT (3,11). We defined the patients with hypertensive encephalopathy secondary to immunosuppressant neurotoxicity as drug related encephalopathy and most cases of calcineurin inhibitor neurotoxicity were related to hypertension (4 in LT, 2 in HT, 6 in HSCT) showing the close relation between the calcineurin inhibitor usage and hypertension. In HT, the restoration of perfusion pressure in previously hypoperfused brain after increasing cardiac output with impaired cerebral autoregulation are reported to be the cause of the hypertensive encephalopathy after HT (20,21,22,29). In KT, post-transplant hypertension within 1 months after transplantation was reported with high incidence of 70%–86% in recipients (30,31) and caused by more complicated factors including immunosuppressant usage, graft renal artery stenosis, sequalae of antibody-mediated rejection, allograft dysfunction, and genetic factors (32). Thus, we suggest that early control of hemodynamic instability, particularly in KT and HT, and careful use of calcineurin inhibitor in all types of organ transplant to prevent hypertensive encephalopathy.
The high incidence of the metabolic encephalopathy in LT can be explained by the frequent hepatic encephalopathy of primary liver failure caused by delayed stabilization of graft function or graft rejection. In the LT patients of our study, 7 of the 8 patients with metabolic encephalopathy developed hepatic encephalopathy due to graft failure.
In allogenic HSCT recipients with encephalopathy, the most common etiology was drug-related encephalopathy, which included calcineurin inhibitor neurotoxicity in 6 patients. Similarly, calcineurin inhibitor neurotoxicity has been reported as the most common etiology of neurologic complications after HSCT (4,6,33). In allogenic HSCT, severe GHVD and an unrelated or mismatched donor type have been suggested to be risk factors for neurologic complications of HSCT (6,33,34). These factors may be in part attributable to aggressive immunotherapeutic treatment of GVHD, which may lead to a higher risk of drug-induced neurotoxicity (14). Moreover, opportunistic CNS infection occurred more frequently in patients with severe GVHD, which was related to chronic immunosuppression (35). Although we could not analyze the risk of encephalopathy in patients with GVHD, 10 of the 16 allogenic HSCT patients with encephalopathy suffered from grade III or higher GVHD in our study.
Interestingly, we also found that the encephalopathy onset time was significantly different according to the type of transplanted organ (P = 0.018). Encephalopathy occurred earlier in HT recipients than in HSCT recipients (median 10 days vs. 49.5 days, P = 0.002). The different etiological distribution of encephalopathy in patients with different transplant types could explain this result. Hypertensive encephalopathy, the most common etiology of HT, mainly occurred in the acute period because of hemodynamic instability. In contrast, encephalopathy in HSCT recipients tended to develop in the later period of transplantation due to engraftment failure, chronic GHVD, and other treatment related morbidities.
The mortality rate of patients with encephalopathy was not significantly different according to the type of transplant. However, it is notable that all the patients with KT associated encephalopathy survived. The high prevalence of hypertensive encephalopathy without devastating neurologic complications such as ICH may be the major factor for this high survival rate in KT. The relatively higher mortality rate in HSCT and LT were associated with other transplant-related morbidity including multiorgan failure, graft failure, and septic shock. Further study with larger cohort to compare the predisposing factors of mortality in each type of transplant will be needed.
In our study, the major neurological cause of death was ICH. ICH is a well-known cause of morbidity and mortality in all types of transplant recipients. It is seen in 1.0% to 7.0% of LT recipients and 0.6% to 5.0% of HSCTs due to coagulopathy, thrombocytopenia, and coexisting CNS infection (14,36). Disseminated intravascular coagulopathy, anticoagulation therapy, prolonged extracorporeal circulation, and hyperperfusion due to improved cardiac output have been implicated in intracranial bleeding in HT recipients (11,37). One study reported that ICH was comparatively rare and responsible for only 1.0% of the deaths after KT (38). This study can explain the higher survival in KT recipients.
The present study had a number of limitations, including a retrospective study carried out in single-center setting and possibility of underestimation of minor neurologic complications in the immediate postoperative period. Yet, this study can be an important guidance on the consultation about the transplantation-related CNS morbidity for the pediatric neurologists.
Transplant-associated encephalopathy in pediatric patients had different characteristics in incidence, etiology, and clinical course according to the type of transplant. Hypertensive encephalopathy was prevalent in acute post-transplant period of HT and KT, and metabolic encephalopathy in LT. All transplant recipients including HSCT recipients must be carefully monitored to prevent drug associated encephalopathy. To the best of our knowledge, the present study is the first to assess the clinical features of encephalopathy according to the type of transplant. Although little evidence is available to correlate perioperative parameters with the definite etiology of encephalopathy, our results indicate that diagnostic approach of neurologic complications should be optimized for each type of transplant.
ACKNOWLEDGMENT
The authors would like to thank Sun-Ok Kim (Asan Medical Center) for statistical analysis.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Lee YJ, Yum MS, Kim EH, Kim MJ, Kim KM, Im HJ, Kim YH, Park YS. Data curation: Lee YJ. Investigation: Lee YJ, Yum MS, Kim EH, Kim MJ, Kim KM, Im HJ, Kim YH, Park YS, Ko TS. Supervision: Ko TS. Writing - original draft: Lee YJ. Writing - review & editing: Yum MS, Ko TS.
References
- 1.U.S. Department of Health and Human Services, Health Resources and Services Administration. OPTN/SRTR 2012 annual data report [Internet] [accessed on 28 January 2016]. Available at http://srtr.transplant.hrsa.gov/annual_reports/2012/Default.aspx.
- 2.Kang JM, Kim YJ, Kim JY, Cho EJ, Lee JH, Lee MH, Lee SH, Sung KW, Koo HH, Yoo KH. Neurologic complications after allogeneic hematopoietic stem cell transplantation in children: analysis of prognostic factors. Biol Blood Marrow Transplant. 2015;21:1091–1098. doi: 10.1016/j.bbmt.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh PS, Kwon C, Klein M, Corder J, Ghosh D. Neurologic complications following pediatric renal transplantation. J Child Neurol. 2014;29:793–798. doi: 10.1177/0883073813490074. [DOI] [PubMed] [Google Scholar]
- 4.Faraci M, Lanino E, Dini G, Fondelli MP, Morreale G, Dallorso S, Manzitti C, Calevo MG, Gaggero R, Castagnola E, et al. Severe neurologic complications after hematopoietic stem cell transplantation in children. Neurology. 2002;59:1895–1904. doi: 10.1212/01.wnl.0000036608.42104.b9. [DOI] [PubMed] [Google Scholar]
- 5.Lee YJ, Yum MS, Kim EH, Choi HW, Oh SH, Kim DY, Kim KM, Ko TS. Risk factors for neurological complications and their correlation with survival following pediatric liver transplantation. Pediatr Transplant. 2014;18:177–184. doi: 10.1111/petr.12218. [DOI] [PubMed] [Google Scholar]
- 6.Koh KN, Park M, Kim BE, Im HJ, Seo JJ. Early central nervous system complications after allogeneic hematopoietic stem cell transplantation in children. Korean J Hematol. 2010;45:164–170. doi: 10.5045/kjh.2010.45.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghaus N, Bohlega S, Rezeig M. Neurological complications in liver transplantation. J Neurol. 2001;248:1042–1048. doi: 10.1007/s004150170023. [DOI] [PubMed] [Google Scholar]
- 8.Pless M, Zivkovic SA. Neurologic complications of transplantation. Neurologist. 2002;8:107–120. doi: 10.1097/00127893-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Senzolo M, Ferronato C, Burra P. Neurologic complications after solid organ transplantation. Transpl Int. 2009;22:269–278. doi: 10.1111/j.1432-2277.2008.00780.x. [DOI] [PubMed] [Google Scholar]
- 10.Iguchi A, Kobayashi R, Yoshida M, Kaneda M, Watanabe N, Cho Y, Arioka H, Naito H, Shikano T, Ishikawa Y. Neurological complications after stem cell transplantation in childhood. Bone Marrow Transplant. 1999;24:647–652. doi: 10.1038/sj.bmt.1701969. [DOI] [PubMed] [Google Scholar]
- 11.Andrews BT, Hershon JJ, Calanchini P, Avery GJ, 2nd, Hill JD. Neurologic complications of cardiac transplantation. West J Med. 1990;153:146–148. [PMC free article] [PubMed] [Google Scholar]
- 12.Jeong MY, Cho YK, Kim SY, Kim YO, Kim CJ, Kook H, Woo YJ, Hwang TJ. Neurologic complications after hematopoietic stem cell transplantation in children. Korean J Pediatr. 2004;47:978–985. [Google Scholar]
- 13.Zivković S. Neuroimaging and neurologic complications after organ transplantation. J Neuroimaging. 2007;17:110–123. doi: 10.1111/j.1552-6569.2007.00097.x. [DOI] [PubMed] [Google Scholar]
- 14.Pruitt AA, Graus F, Rosenfeld MR. Neurological complications of transplantation: part I: hematopoietic cell transplantation. Neurohospitalist. 2013;3:24–38. doi: 10.1177/1941874412455338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pruitt AA, Graus F, Rosenfeld MR. Neurological complications of solid organ transplantation. Neurohospitalist. 2013;3:152–166. doi: 10.1177/1941874412466090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500. doi: 10.1056/NEJM199602223340803. [DOI] [PubMed] [Google Scholar]
- 17.Belvís R, Martí-Fàbregas J, Cocho D, García-Bargo MD, Franquet E, Agudo R, Brosa V, Campreciós M, Puig M, Martí-Vilalta JL. Cerebrovascular disease as a complication of cardiac transplantation. Cerebrovasc Dis. 2005;19:267–271. doi: 10.1159/000084091. [DOI] [PubMed] [Google Scholar]
- 18.Jarquin-Valdivia AA, Wijdicks EF, McGregor C. Neurologic complications following heart transplantation in the modern era: decreased incidence, but postoperative stroke remains prevalent. Transplant Proc. 1999;31:2161–2162. doi: 10.1016/s0041-1345(99)00294-8. [DOI] [PubMed] [Google Scholar]
- 19.Burra P, Senzolo M, Pizzolato G, Tursi V, Livi U, Chierichetti F, Dam M. Frontal cerebral blood flow is impaired in patients with heart transplantation. Transpl Int. 2002;15:459–462. doi: 10.1007/s00147-002-0448-3. [DOI] [PubMed] [Google Scholar]
- 20.Massaro AR, Dutra AP, Almeida DR, Diniz RV, Malheiros SM. Transcranial Doppler assessment of cerebral blood flow: effect of cardiac transplantation. Neurology. 2006;66:124–126. doi: 10.1212/01.wnl.0000191397.57244.91. [DOI] [PubMed] [Google Scholar]
- 21.van Mook WN, Rennenberg RJ, Schurink GW, van Oostenbrugge RJ, Mess WH, Hofman PA, de Leeuw PW. Cerebral hyperperfusion syndrome. Lancet Neurol. 2005;4:877–888. doi: 10.1016/S1474-4422(05)70251-9. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz RB. Hyperperfusion encephalopathies: hypertensive encephalopathy and related conditions. Neurologist. 2002;8:22–34. doi: 10.1097/00127893-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Yu S, Liebeskind DS, Dua S, Wilhalme H, Elashoff D, Qiao XJ, Alger JR, Sanossian N, Starkman S, Ali LK, et al. Postischemic hyperperfusion on arterial spin labeled perfusion MRI is linked to hemorrhagic transformation in stroke. J Cereb Blood Flow Metab. 2015;35:630–637. doi: 10.1038/jcbfm.2014.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agildere AM, Başaran C, Cakir B, Ozgül E, Kural F, Haberal M. Evaluation of neurologic complications by brain MRI in kidney and liver transplant recipients. Transplant Proc. 2006;38:611–618. doi: 10.1016/j.transproceed.2005.12.113. [DOI] [PubMed] [Google Scholar]
- 25.Dhar R, Young GB, Marotta P. Perioperative neurological complications after liver transplantation are best predicted by pre-transplant hepatic encephalopathy. Neurocrit Care. 2008;8:253–258. doi: 10.1007/s12028-007-9020-4. [DOI] [PubMed] [Google Scholar]
- 26.Sotil EU, Gottstein J, Ayala E, Randolph C, Blei AT. Impact of preoperative overt hepatic encephalopathy on neurocognitive function after liver transplantation. Liver Transpl. 2009;15:184–192. doi: 10.1002/lt.21593. [DOI] [PubMed] [Google Scholar]
- 27.Parasole R, Petruzziello F, Menna G, Mangione A, Cianciulli E, Buffardi S, Marchese L, Nastro A, Misuraca A, Poggi V. Central nervous system complications during treatment of acute lymphoblastic leukemia in a single pediatric institution. Leuk Lymphoma. 2010;51:1063–1071. doi: 10.3109/10428191003754608. [DOI] [PubMed] [Google Scholar]
- 28.Baytan B, Evim MS, Güler S, Güneş AM, Okan M. Acute central nervous system complications in pediatric acute lymphoblastic leukemia. Pediatr Neurol. 2015;53:312–318. doi: 10.1016/j.pediatrneurol.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Gruhn N, Larsen FS, Boesgaard S, Knudsen GM, Mortensen SA, Thomsen G, Aldershvile J. Cerebral blood flow in patients with chronic heart failure before and after heart transplantation. Stroke. 2001;32:2530–2533. doi: 10.1161/hs1101.098360. [DOI] [PubMed] [Google Scholar]
- 30.Baluarte HJ, Gruskin AB, Ingelfinger JR, Stablein D, Tejani A. Analysis of hypertension in children post renal transplantation--a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) Pediatr Nephrol. 1994;8:570–573. doi: 10.1007/BF00858130. [DOI] [PubMed] [Google Scholar]
- 31.Tejani A. Post-transplant hypertension and hypertensive encephalopathy in renal allograft recipients. Nephron. 1983;34:73–78. doi: 10.1159/000182985. [DOI] [PubMed] [Google Scholar]
- 32.Büscher R, Vester U, Wingen AM, Hoyer PF. Pathomechanisms and the diagnosis of arterial hypertension in pediatric renal allograft recipients. Pediatr Nephrol. 2004;19:1202–1211. doi: 10.1007/s00467-004-1601-2. [DOI] [PubMed] [Google Scholar]
- 33.Uckan D, Cetin M, Yigitkanli I, Tezcan I, Tuncer M, Karasimav D, Oguz KK, Topçu M. Life-threatening neurological complications after bone marrow transplantation in children. Bone Marrow Transplant. 2005;35:71–76. doi: 10.1038/sj.bmt.1704749. [DOI] [PubMed] [Google Scholar]
- 34.Weber C, Schaper J, Tibussek D, Adams O, Mackenzie CR, Dilloo D, Meisel R, Göbel U, Laws HJ. Diagnostic and therapeutic implications of neurological complications following paediatric haematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41:253–259. doi: 10.1038/sj.bmt.1705905. [DOI] [PubMed] [Google Scholar]
- 35.Maschke M, Dietrich U, Prumbaum M, Kastrup O, Turowski B, Schaefer UW, Diener HC. Opportunistic CNS infection after bone marrow transplantation. Bone Marrow Transplant. 1999;23:1167–1176. doi: 10.1038/sj.bmt.1701782. [DOI] [PubMed] [Google Scholar]
- 36.Zivković SA. Neurologic complications after liver transplantation. World J Hepatol. 2013;5:409–416. doi: 10.4254/wjh.v5.i8.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alejaldre A, Delgado-Mederos R, Santos MÁ, Martí-Fàbregas J. Cerebrovascular complications after heart transplantation. Curr Cardiol Rev. 2010;6:214–217. doi: 10.2174/157340310791658811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wijdicks EF, Torres VE, Schievink WI, Sterioff S. Cerebral hemorrhage in recipients of renal transplantation. Mayo Clin Proc. 1999;74:1111–1112. doi: 10.4065/74.11.1111. [DOI] [PubMed] [Google Scholar]