Supplemental Digital Content is available in the text
Abstract
No safe threshold level of lead exposure in children has been recognized. Also, the information on shielding effect of maternal dietary iron intake during pregnancy on the adverse effects of prenatal lead exposure on children's postnatal neurocognitive development is very limited. We examined the association of prenatal lead exposure and neurodevelopment in children at 6, 12, 24, and 36 months and the protective action of maternal dietary iron intake against the impact of lead exposure.
The study participants comprise 965 pregnant women and their subsequent offspring of the total participants enrolled in the Mothers and Children's environmental health study: a prospective birth cohort study. Generalized linear model and linear mixed model analysis were performed to analyze the effect of prenatal lead exposure and mother's dietary iron intake on children's cognitive development at 6, 12, 24, and 36 months.
Maternal late pregnancy lead was marginally associated with deficits in mental development index (MDI) of children at 6 months. Mothers having less than 75th percentile of dietary iron intake during pregnancy showed significant increase in the harmful effect of late pregnancy lead exposure on MDI at 6 months. Linear mixed model analyses showed the significant detrimental effect of prenatal lead exposure in late pregnancy on cognitive development up to 36 months in children of mothers having less dietary iron intake during pregnancy.
Thus, our findings imply importance to reduce prenatal lead exposure and have adequate iron intake for better neurodevelopment in children.
INTRODUCTION
The detrimental impact of lead on children's development still remains a major issue worldwide. The burden of neurological disorders due to lead is estimated to be 1% of the global burden of disease.1 Lead exposure causes adverse effect on children's intelligence, behavior, and memory. The developing brain is most damaged by lead exposure2 and harmful effects on children's cognitive development even with low environmental lead exposure are reported.3 Studies have shown a decrease in children's intelligence quotient whose blood lead levels were less than 10 μg/dL.4,5 Recently, the Centers for Disease Control and Prevention (CDC) recommended the reference blood lead level of 5 μg/dL to prevent harmful effects on children.6 However, no safe threshold of blood lead level in children has been identified.
Lead freely crosses through the placental membranes, thus maternal lead exposure can significantly impact the fetus.7 As fetuses and children's brain grow rapidly, even very low level of lead exposure can cause detrimental effects to a child's cognitive development. An earlier study8 showed that mean maternal blood lead levels <6.5 μg/dL are negatively associated with the cognitive development of children. Also, a report showed an inverse association between prenatal lead exposure <5 μg/dL and cognitive development in children at 24 months.7 Even though some studies have demonstrated the effect of low prenatal lead exposure on postnatal cognitive growth in children, the results remain inconsistent. More evidence is needed to make definite conclusions regarding the effect of very low prenatal lead exposure on postnatal cognitive development in early childhood.
On the other hand, the adverse effects of iron deficiency on cognitive development are known. Iron deficiency affects the mental, motor, and cognitive development of children.9,10 The demand of iron increases substantially to support the growth of fetus and due to the expansion of maternal blood volume during pregnancy.11 Thus, maternal anemia is associated with preterm birth and infant low birth weight.12 Also, iron and lead compete for same divalent metal transporter 1 (DMT1) in the gastro-intestinal tract,13 and consequently, iron deficiency increases expression of DMT1 in the duodenum, thereby increasing lead uptake.14 Hence, low dietary iron intake during pregnancy creates a positive condition for an increase in the harmful effect of lead on the fetus. The knowledge regarding the interaction between iron intake and lead exposure and its effect on children's neurodevelopment is limited.
METHODS
Study Participants
This study was conducted as a part of Mothers and Children's Environmental Health (MOCEH) study. The MOCEH study is a multicenter prospective birth cohort study designed to examine pre and postnatal environmental exposures on growth and development of children from fetus through young adulthood. There are 3 regional centers in the study located in Seoul, Cheonan, and Ulsan. Each center has a community-based network consisting of a university hospital, local clinics, and community public health centers. Women who lived in these cities and who were over the age of 18 years were enrolled before 20 weeks of pregnancy. Written informed consent was obtained at the initial visit from all of enrolled mothers on behalf of themselves and their children. All protocols were approved by the Institutional Review Board of Ewha Womans University Hospital, Dankook University Hospital, and Ulsan University Hospital.
A total of 1751 pregnant women were enrolled from May 2006 to December 2010 according to previously described study protocols.15 The study subjects were restricted to those in whom prenatal maternal blood lead level was assessed, and postnatal children's neurodevelopment measurements were performed at 6, 12, 24, and 36 months of age. Of the 1475 eligible participants, 510 subjects were excluded for the reasons of low birth weight (<2500 g, N = 41), preterm birth (gestational week <37, N = 39), missing information on gestational week (N = 36), early pregnancy lead concentration (N = 41), and mental development index (MDI)/psychomotor development index (PDI) at 6 months (N = 353). The final participants were 965 pregnant women and their babies (Figure 1). We did not find significant differences in the characteristics between the included pregnant women at recruitment and their newborns at birth and those who were excluded (Supplemental file: Table S1). Some babies were lost to follow-up from the 965 pregnant women and their babies at 6 months. Ultimately, 732, 655, and 558 children at 12, 24, and 36 months, respectively, were included in the analysis (Figure 1).
FIGURE 1.
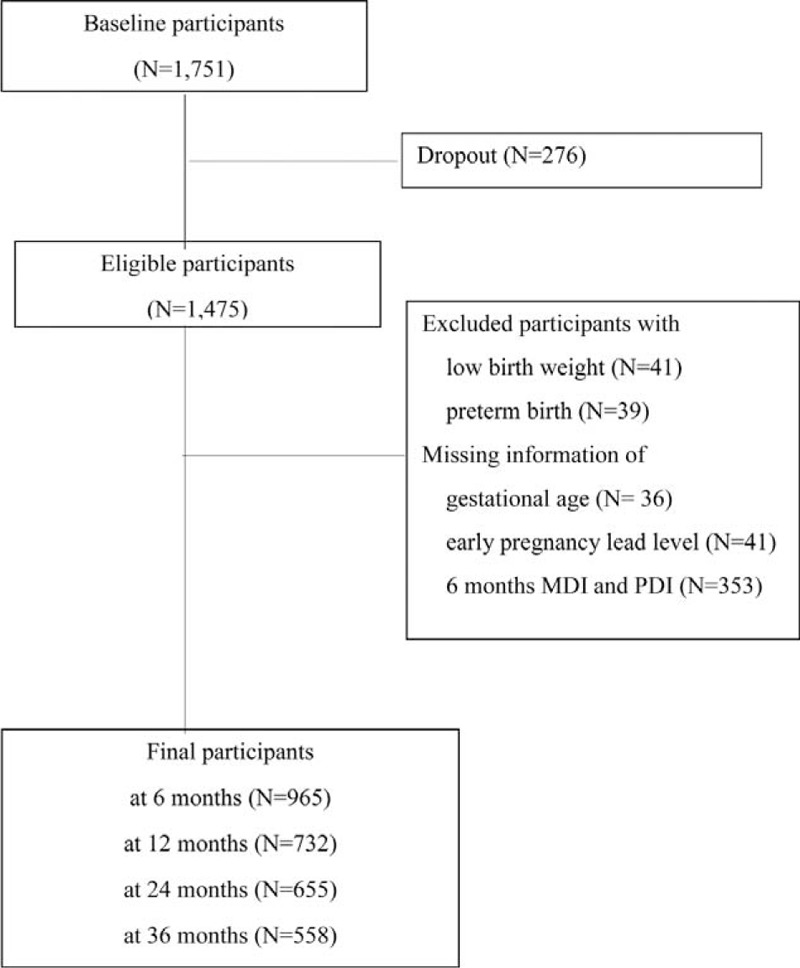
Selection process of study participants.
Data Collection on Maternal Dietary iron Intake
Information on dietary intake was collected by 24-hour recall. Experienced, well-trained dietary interviewers instructed the respondents to recall and describe all of the foods and beverages that they had consumed over the past 24 hours. Extra details were obtained regarding items like snacks, drinks, in the subjects who were not able to recall what they had eaten in the past 24 hours. All of the pregnant women were asked if their intake on the day of the 24-hour recall was representative of their typical intake. Information about portion sizes was gathered according to defined units and recorded on a form. The food items were modeled in a defined unit and illustrated to the respondents for increasing the reporting accuracy.16 Each subject's reported portions were converted to gram unit.16 The subject's dietary intakes of nutrients and food groups were quantified using a computer-aided nutritional analysis program (CAN-Pro 3.0, Korean Nutrition Society, Seoul, Korea).
Maternal and Cord Blood Lead Measurements
Whole blood samples were obtained in metal-free tubes at enrollment before gestation week 20 and at delivery, as being representative of the early and late gestational period, respectively and umbilical cord blood at birth. The blood samples were frozen and stored at −70oC. For measurement of lead levels, the samples were brought to room temperature and vortexed after thawing. In total, 0.1 mL of blood was diluted with 0.1% Triton X-100. The samples were mixed well using a vortex mixer and assayed by atomic absorption spectrometry on the Analyst 100 instrument (Perkin-Elmer, Norwalk, Connecticut) using a graphite tube atomizer (HGA 800; Perkin-Elmer GmbH, Uberlinger, Germany). Lead concentrations were quantified in the deuterium background correction mode. For internal quality assurance and control purposes, commercial reference materials were obtained from Bio-Rad (Lyphocheks Whole Blood Metals Control, Bio-Rad, Hercules, CA). An internal control was used for each series of analyses. The limit of detection (LOD) was 0.12 μg/dL and no sample had levels below the LOD.
Neurodevelopment Assessment
Children's neurodevelopment was assessed at 6, 12, 24, and 36 months using the Korean version of Bayley Scales of Infant Development II (K-BSID-II).17 The Korean version has shown test–retest stability and inter-rater agreement.18 The K-BSID-II assesses habituation, problem solving, memory, classification, vocalization, and language skills. The resulting score is called the mental development index (MDI). The psychomotor development index (PDI) is scored on the degree of body control, muscle coordination, postural control, and finer manipulatory skills. The test score was standardized as having a mean of 100 and a standard deviation of 15.19 To increase the inter-rater consistency, annual rater training sessions with video monitoring were held (inter-rater consistency; kappa value >0.8).20 The prenatal lead level of each participant was blinded to the examiners.19 The mother's intelligence levels were measured by using the short form of Korean Wechsler Adult Intelligence Scale21 during her postnatal visit to the hospital.
Information on Confounders and Covariates
Data were collected on maternal prenatal characteristics using questionnaires that addressed maternal socio-demographic factors and previous obstetric history by trained nurses. The body mass index (BMI) of the pregnant women was calculated according to the WHO method (body weight (kg) divided by height (m2) and categorized into 3 groups: underweight (<18.5 kg/m2), normal (∼23 kg/m2), and overweight (> 23 kg/m2).22 The gestational age was calculated using the information of last menstrual period. When the information of the last menstrual period was unreliable, or a significant discordance of dating (>10 days) between ultrasonographic estimation and the last menstrual period existed, the gestational age estimated by the first ultrasonography was used.22 The information of birth weight was obtained from the medical charts recorded in the delivery room.22 Information on sex, birth weight, gestational age, and birth order was collected from medical records at the time of delivery.22 Information on covariates and variables affecting neurodevelopment such as breastfeeding, mother's education, and family income was collected from the mother during their hospital visits. Information on maternal dietary calcium intake obtained by 24-hour recall was used as a covariate as well.
Statistical Analysis
The characteristics of study subjects were analyzed using t test for continuous variables and χ2 test for categorical variables. Blood lead concentrations were log transformed due to a non-normal distribution. We selected covariates based on biological (eg, maternal and gestational age, mother's intelligence quotient) and environmental (eg, maternal education) considerations. Generalized linear model (GLM) was used to estimate the effects of prenatal maternal and cord blood lead level on children's cognitive development. The dependent variables were MDI and PDI at 6, 12, 24, and 36 months, and the independent variables were maternal age, education, intelligence quotient, urinary cotinine level, dietary calcium intake and child's gestational age, birth weight, birth order, sex, breastfeeding history and center location. Due to the limited sample size, the missing data of variables of mother's age, education, intelligence quotient, urinary cotinine, birth order, and breastfeeding were converted into an unknown category and included in the analyses. The number of participants decreased during the follow-up period. However, there was no significant difference between the participants followed and those who were lost to follow-up (Supplemental file: Table S2). Generalized additive models were applied to illustrate the relationships between maternal blood lead levels and the child's neurodevelopment at 6 months.
We examined interaction between prenatal lead exposure and mother's dietary iron intake on multiplicative scale. GLM analyses stratified by mother's 75th percentile iron intake group were conducted using the same covariates as in the main analysis.
A linear mixed model (LMM) analysis was done to evaluate the relationship between prenatal lead exposure and MDI and PDI from 6 to 36 months. We used same covariates as in the GLM along with the addition of time and interaction term between lead and time. We used compound symmetry matrix as the covariance structure in LMM. Model selection was based on the value of Akaike Information Criteria (smaller the better). Stratified LMM analyses were performed after dividing the subjects into 2 groups by the mother's 75th percentile iron intake at enrollment using the same covariates as in the main analysis. We defined statistical significance as P value <0.05. Data were analyzed using SAS version 9.3 (SAS Institute Inc, Cary, North Carolina) and R version 3.0.3 (The Comprehensive R Archive Network: http://cran.r-project.org).
RESULTS
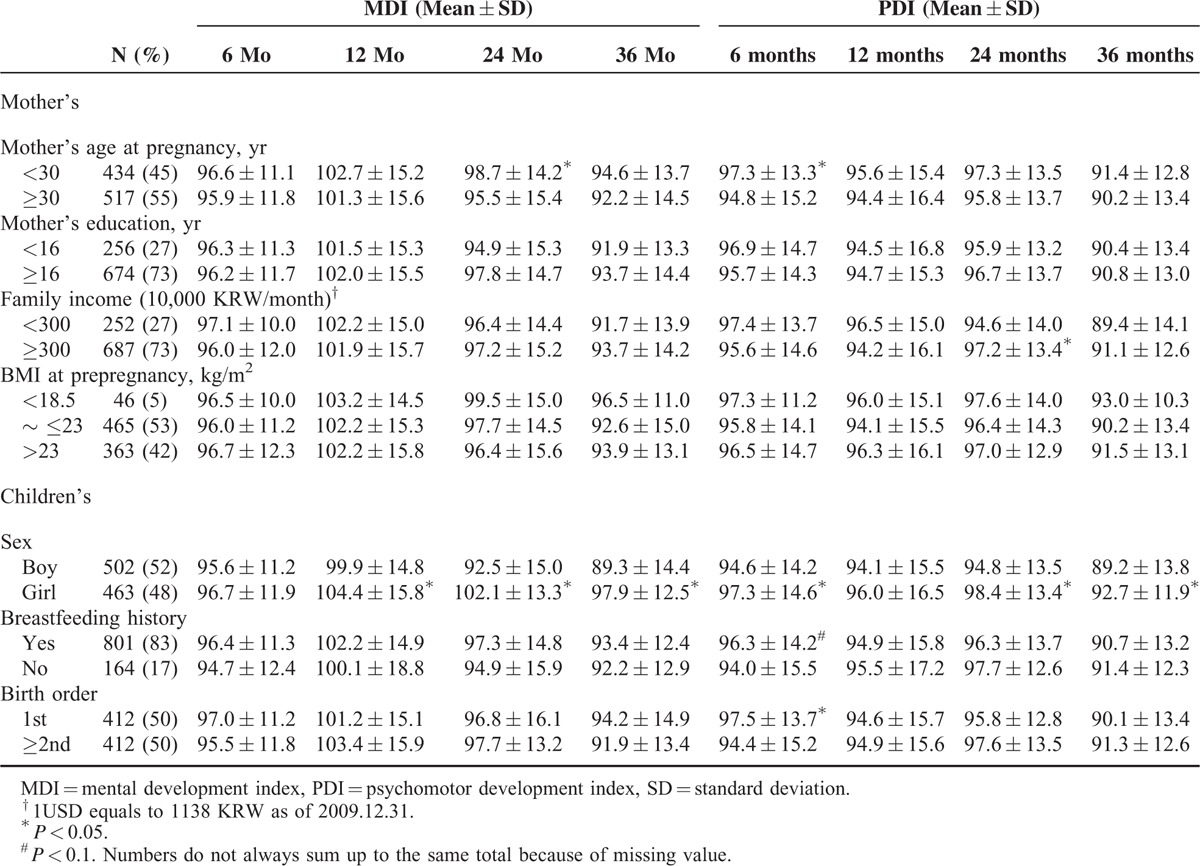
Of the study subjects, 55% of the mothers were over the age of 30 years. Almost one-third of the mothers did not have university education and had a family income which was considered to be relatively low. Girls showed significantly higher scores in MDI at 12, 24, and 36 months and in PDI at 6, 24, and 36 months than boys. MDI scores were significantly higher in children with younger mother at 24 months. PDI scores were significantly higher in those with younger mother and who were first child at 6 months but were lower at 24 months in those with less family income (Table 1).
TABLE 1.
General Characteristics of 965 Study Participants
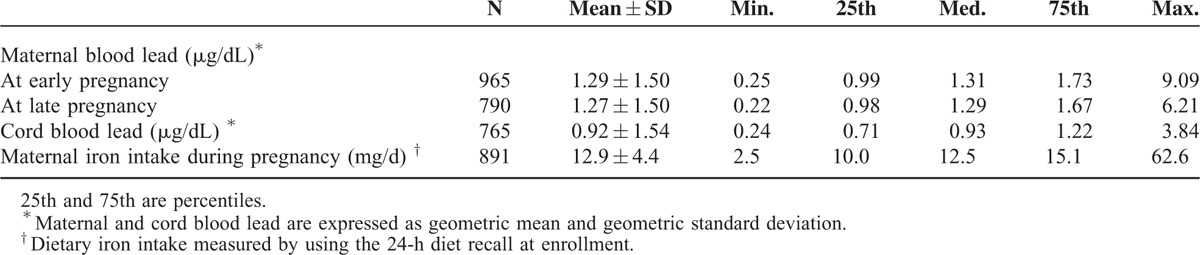
The mean blood lead levels of all participating mothers were 1.29 and 1.27 μg/dL in the early and late gestational periods, respectively, and the mean dietary iron intake of mothers at the time of enrollment was 12.9 mg/d and almost 98% of the mother's had their iron intake less than recommended dietary allowances for Koreans (Table 2).23
TABLE 2.
Distribution of Maternal and Cord Blood Lead and Maternal Dietary Iron Intake at Enrollment in Pregnant Women
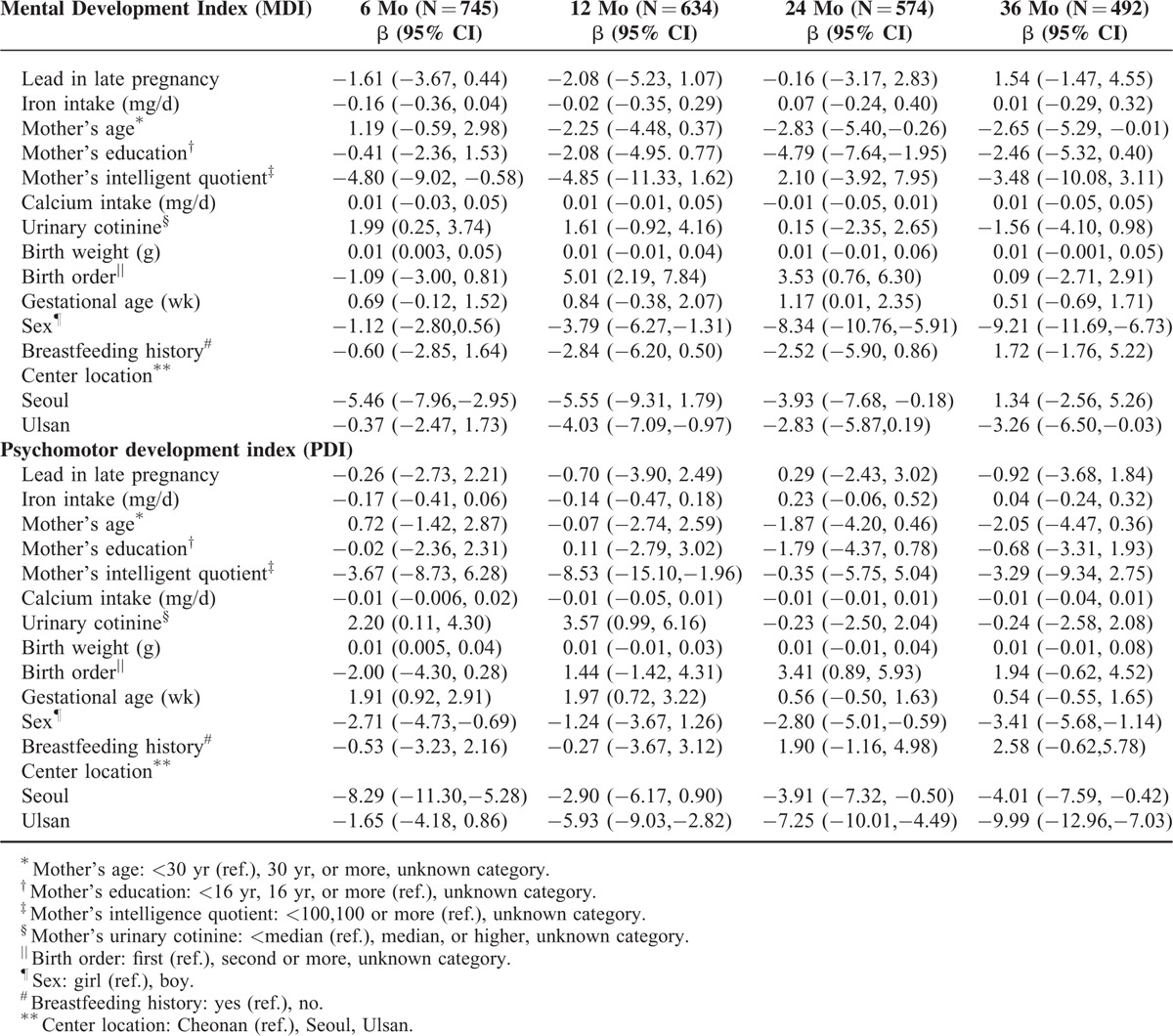
Dietary iron intake was negatively associated, but not significantly, with late maternal blood lead level (r = −0.03, P = 0.45), or with the MDI and PDI at 6 months (r = −0.02, P = 0.43 and r = −0.03, P = 0.33, respectively). The GLM analyses for maternal blood lead levels and child's MDI and PDI showed that lead levels of late pregnancy were marginally negatively associated with MDI at 6 months of age (β = −1.61, P = 0.12) after adjusting for mother's age, intelligence quotient, education, dietary calcium intake, urinary cotinine level, child's gestational age, birth weight, birth order, sex, and breastfeeding history (Table 3). There was significant multiplicative interaction between early prenatal lead and mother's iron intake in PDI at 6 months. We did not find significant associations between MDI or PDI, and maternal early pregnancy or cord blood lead (Supplementary Table S3).
TABLE 3.
Generalized Linear Model (GLM) Analyses on the Association Between Maternal Late Pregnancy Blood Lead and Children's Neurodevelopment at 6, 12, 24, and 36 Mo
As illustrated in Figure 2, the linear inverse relationship was seen between late pregnancy blood lead levels, MDI, and PDI at age 6 months in the low prenatal iron intake group. Also, no significant difference in the maternal blood lead levels across the strata by iron intake was observed.
FIGURE 2.
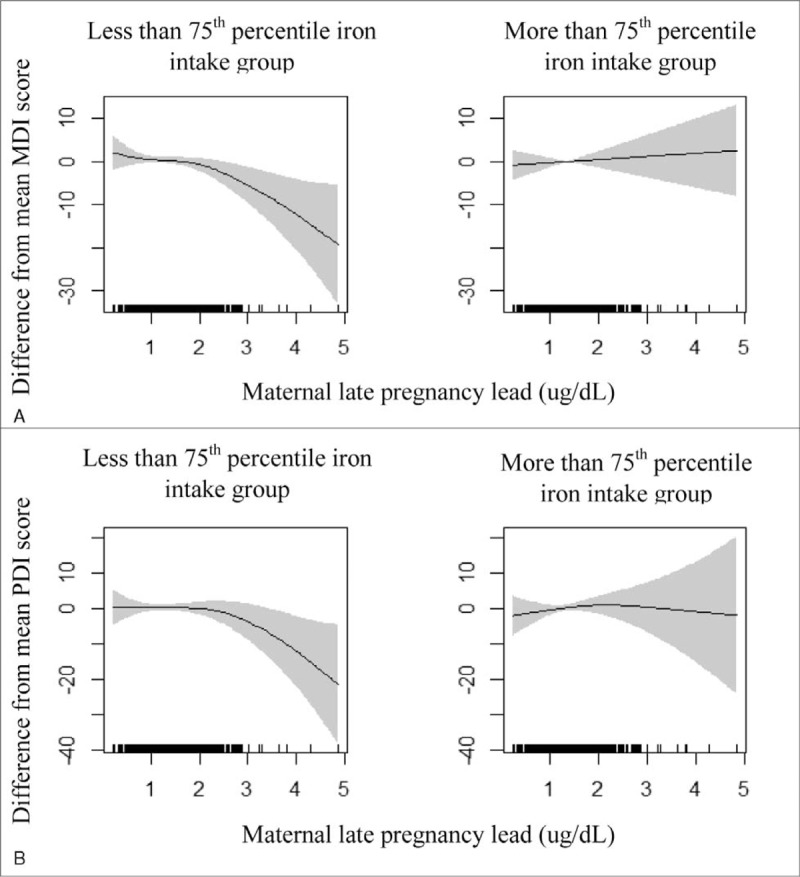
Association between late pregnancy blood lead, MDI, and PDI at 6 months by maternal dietary iron intake group. A, Mental development index (MDI). B, Psychomotor development index (PDI). The plots were generated by the generalized additive model adjusted for mother's education, age, intelligence quotient, urinary cotinine, dietary calcium intake and child's gestational age, birth weight, birth order, sex, breast feeding, history and center location.
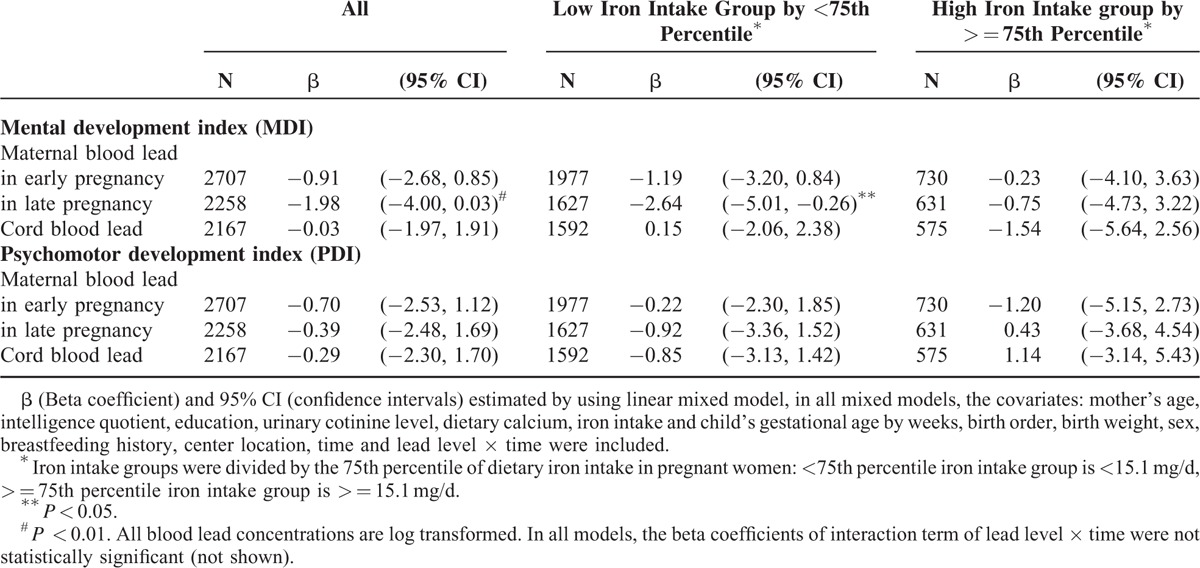
Stratification analysis by maternal iron intake significantly strengthened the association of late pregnancy blood lead and MDI at 6 months (β = −2.53, P = 0.04) in the less than 75th percentile of the prenatal iron intake group (Table 4). No significant association was seen in analysis stratified by maternal iron intake in lead level in maternal early pregnancy or cord blood and MDI or PDI (Supplementary Table S4). As shown in Table 5, with mixed model analysis, the late prenatal lead exposure had significant negative effect on children's neurodevelopment up to 36 months of age (β = −2.64, P = 0.04) in the maternal less iron intake group.
TABLE 4.
Generalized Linear Model (GLM) Analyses on the Association Between Maternal Late Pregnancy Blood Lead and Children's Neurodevelopment at 6, 12, 24, and 36 Mo According to Maternal Iron Intake
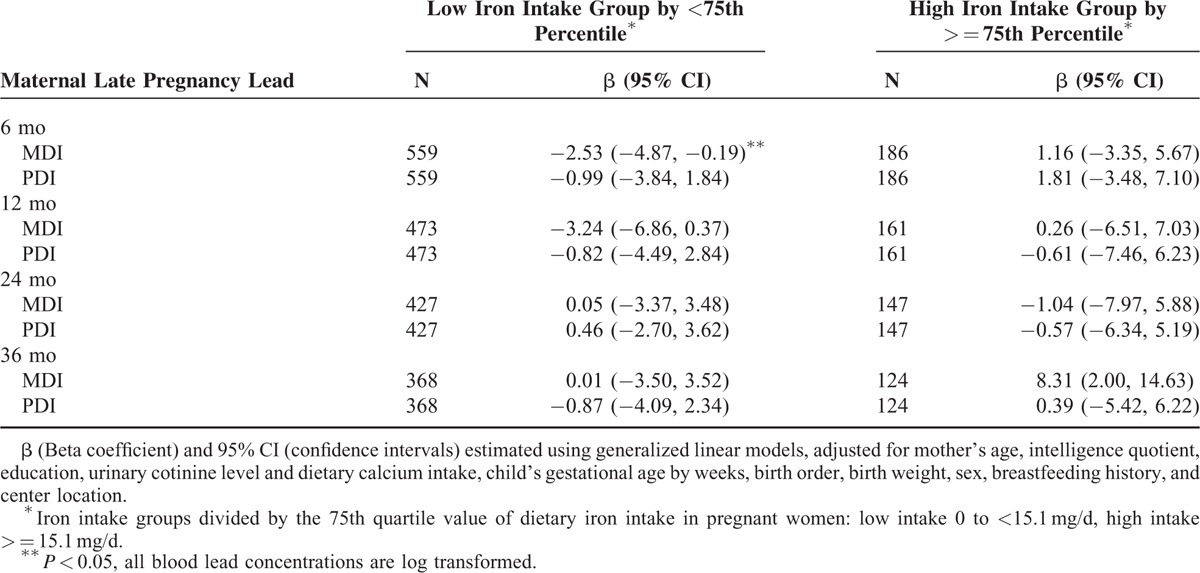
TABLE 5.
Mixed Model Analyses on the Association Between Maternal and Cord Blood Lead and Children's Neurodevelopment up to 36 Mo According to Maternal Iron Intake
DISCUSSION
Our study shows negative association for blood lead levels <5 μg/dL (geometric mean = 1.27 ug/dL) in late pregnancy with the cognitive development of children 6 months old. The less iron intake during pregnancy further aggravated the effect of prenatal lead exposure on neurodevelopment of children. The harmful effect of late pregnancy lead exposure on the neurodevelopment of children lasted up to 36 months of age. This adverse effect of maternal late pregnancy lead was amplified in the inadequate iron intake group.
Prenatal lead exposure has been negatively associated with reduced children's cognitive development.7,24 Study has reported25 that one standard deviation increase in the first trimester maternal pregnancy lead was associated with a reduction in MDI score by 3.5 points. Inverse association between maternal blood lead during last trimester of pregnancy and intellectual development of children has also been reported.24 On the other hand, cord blood lead was found to be associated with impaired cognitive development of children.7 Hence, the window of prenatal exposure affecting children's mental growth needs to be confirmed.
Maternal blood lead levels measured during the period of gestation are the most accurate biomarker of prenatal lead exposure, since toxicokinetic studies have reported robust placental transport of lead during the last trimester.2 However, it is not clear which blood measure is most suitable, that is, which specified period of gestation. In our study, we used both early and late pregnancy blood lead and cord blood lead. Lead crosses the blood brain barrier26 as well as the blood placental barrier27 and affects the developing brain. Brain development in the first trimester of pregnancy is different than in the last trimester. Proliferation and differentiation of neurons is completed by the first trimester but the aggregation and migration of neurons continues until the last trimester of pregnancy.24 Myelination of nerves begins after 25 weeks of pregnancy in the fetal brain28 and the deep cortical layers start developing after 24 weeks, becoming clearly defined by 28 weeks.29 The significant negative association between children's MDI at 6 months of age and late pregnancy blood lead but the lack of association with early pregnancy lead (≤20 weeks of gestational age) in the present study seems to be interpretable with these previous findings.
We did not find a significant association between cord blood lead and cognitive development in children, but maternal late pregnancy lead was significantly positively correlated with cord blood lead (r = 0.54, P < 0.01) suggesting that lead can diffuse from the mother's bloodstream to the growing fetus through the placenta.30 The extremely low level and narrow range of cord blood lead in the subjects of the present study may be the reason why we obtained insignificant results.
Although the mechanism underlying the harmful effects of neurotoxicity in the developing brain due to lead is not clearly understood, disruption of neural cell myelination and cell differentiation might be a possible mechanism.31 Lead disrupts the intraneural regulatory mechanism by decreasing the number of synapses32 and altering the synaptic width and curvature. This interferes with the coordination of nerve cells, resulting in poor neural connectivity.26 Lead decreases the width, granule cell density, and dendritic arborization of the molecular layer of the cerebellum. Lead interferes with neurotransmitter release, and it affects neuro-transmission by disturbing synaptic activity.33 Thus, lead disrupts the organization of the human cortex34 and the electrophysiological functioning of the central nervous system.8,35 Iron deficiency and lead exposure have adverse effect on nervous system as lead substitutes iron and alters the anatomy and physiology of nerve cells.10 Iron deficiency may increase the rate of lead uptake by astrocytes in brain by DMT1.36 Iron is very important in the maintenance of the oligodendrocyte function and participates in myelin formation. Iron uptake is increased to most during peak myelination of nerve cells.37 Iron deficiency causes a reduction in myelin components such as proteins and lipids.37 Due to a reduction in myelination, glial cells that protect the neuron from lead exposure are incapable of guarding the neurons from the deleterious injury due to lead.38 Thus lead affects oligodendrocyte development38 and disrupts myelin formation.39 Iron deficiency also affects neurotransmission by reducing the number and function of dopamine receptors, particularly D2 and transporters,40 which may increase the harmful effect of lead exposure on nervous system. Iron deficiency may induce a deficit in neurocognitive development directly and also through increased lead absorption. This advocates that lead exposure and iron deficiency are associated with alterations in neural structure and physiology.10 The detrimental effect of lead in developing brain was more pronounced in the low dietary iron intake group in the present study, a result compatible with the previous findings.
One of the study's strengths is that the effect of very low prenatal lead exposure (less than 5 ug/dL) on neurodevelopment of children up to 36 months of age was assessed. There are limited studies reporting the adverse effect of prenatal lead exposure <5 ug/dL on the postnatal cognitive development of children.7,8,25 The second strength is its longitudinal study design, which allowed us to evaluate the effect of prenatal lead exposure on children's neurodevelopment as the children's growing. In addition, the finding that low dietary iron intake magnifies the effect of lead neurotoxicity suggests the potential benefit of dietary intervention to avert the toxic influence of lead exposure during pregnancy. Recently, in one of our other studies, a similar harmful effect of prenatal blood lead and calcium intake on postnatal physical growth was reported.41 The possibility of dietary prevention of the harmful effect of prenatal lead may not be limited to physical growth but also include children's neurodevelopment.
Our study also had its limitations. We had no information regarding the biochemical parameters of the iron statuses of mothers and babies, and this could have biased our results. Although we adjusted for potential confounders, we could not consider others such as exposure to unmeasured toxic pollutants. Lastly, the results cannot be generalized beyond the race of the study population because all the participants were Koreans.
CONCLUSION
Late pregnancy maternal blood lead levels <5 μg/dL affect the neurodevelopment of children up to 36 months of age. Also, lower prenatal dietary iron intake intensifies the adverse effects of prenatal lead exposure in children's neurodevelopment. Our study suggests the necessity of protection and intervention for pregnant women with low levels of lead exposure along with iron insufficiency.
Supplementary Material
Acknowledgment
We are grateful to mothers and children of MOCEH study for their participation in this study.
Footnotes
Abbreviations: BMI = body mass index, CDC = Centers for Disease Control and Prevention, DMT1 = Divalent Metal Transporter 1, GLM = generalized linear model, K-BSID-II = Korean version of Bayley Scales of Infant Development II, LMM = linear mixed model, MDI = mental development index, MOCEH = Mothers and Children's Environmental Health, PDI = psychomotor development index.
SS-K and MH made equal contribution as first author.
This study was supported by Mothers and Children's Environmental Health (MOCEH) project of the National Institute of Environmental Research, Republic of Korea (http://www.nier.go.kr). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
REFERENCES
- 1.Fewtrell LJ, Prüss-Üstün A, Landrigan P, et al. Estimating the global burden of disease of mild mental retardation and cardiovascular diseases from environmental lead exposure. Environ Res 2004; 94:120–133. [DOI] [PubMed] [Google Scholar]
- 2.Liu JA, Chen Y, Gao D, et al. Prenatal and postnatal lead exposure and cognitive development of infants followed over the first three years of life: a prospective birth study in the Pearl River Delta region, China. Neurotoxicology 2014; 44:326–334. [DOI] [PubMed] [Google Scholar]
- 3.Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr 2008; 20:172–177. [DOI] [PubMed] [Google Scholar]
- 4.Canfield RL, Henderson CR, Jr, Cory-Slechta DA, et al. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N Engl J Med 2003; 348:1517–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children's intellectual function: an international pooled analysis. Environ Health Perspect 2005; 113:894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. Advisory Committee on Childhood Lead Poisoning Prevention. Low level lead exposure harms children: a renewed call for primary prevention. CDC. Available at: http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf Accessed May 20, 2015. [Google Scholar]
- 7.Jedrychowski W, Perera FP, Jankowski J, et al. Very low prenatal exposure to lead and mental development of children in infancy and early childhood. Neuroepidemiology 2009; 32:270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vigeh M, Yokoyama K, Matsukawa T, et al. Low level prenatal blood lead adversely affects early childhood mental development. J Child Neurol 2014; 29:1305–1311. [DOI] [PubMed] [Google Scholar]
- 9.Lozoff B. Iron deficiency and child development. Food Nutr Bull 2007; 28 Supplement 4:560S–571S. [DOI] [PubMed] [Google Scholar]
- 10.Kordas K. Iron, lead, and children's behavior and cognition. Annu Rev Nutr 2010; 30:123–148. [DOI] [PubMed] [Google Scholar]
- 11.Fernández-Ballart JD. Iron metabolism during pregnancy. Clin Drug Investig 2000; 19:9–19. [Google Scholar]
- 12.Scholl TO, Reilly T. Anemia, iron and pregnancy outcome. J Nutr 2000; 130:443S–447S. [DOI] [PubMed] [Google Scholar]
- 13.Kwong WT, Friello P, Semba RD. Interactions between iron deficiency and lead poisoning: epidemiology and pathogenesis. Sci Total Environ 2004; 330:21–37. [DOI] [PubMed] [Google Scholar]
- 14.Bannon D, Portnoy ME, Olivi L, et al. Uptake of lead and iron by divalent metal transporter 1 in yeast and mammalian cells. Biochem Biophys Res Commun 2002; 295:978–984. [DOI] [PubMed] [Google Scholar]
- 15.Kim BM, Ha M, Park HS, et al. The mothers and children's environmental health (MOCEH) study. Eur J Epidemiol 2009; 24:573–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim H, Kim G, Jang W, et al. Association between intake of B vitamins and cognitive function in elderly Koreans with cognitive impairment. Nutr J 2014; 13:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bayley N. Bayley Scales of Infant Development. 2nd ed.San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- 18.Park HW, Cho BH. Korean Bayley Scales of Infant Development. Interpretation Manual. 2nd ed.Seoul, Korea: Kidspop Publishing Corporation; 2006. [Google Scholar]
- 19.Kim Y, Ha EH, Park H, et al. Prenatal lead and cadmium co-exposure and infant neurodevelopment at 6 months of age: the Mothers and Children's Environmental Health (MOCEH) study. Neurotoxicology 2013; 35:15–22. [DOI] [PubMed] [Google Scholar]
- 20.Kim E, Park H, Hong YC, et al. Prenatal exposure to PM10 and NO2 and children's neurodevelopment from birth to 24 months of age: Mothers and Children's Environmental Health (MOCEH) study. Sci Total Environ 2014; 481:439–445. [DOI] [PubMed] [Google Scholar]
- 21.Um TH, Park YS, Oh KJ, et al. Manual for the Korean Wechsler Adult Intelligence Scale. Seoul: Guidance; 1992. [Google Scholar]
- 22.Kim BM, Lee BE, Hong YC, et al. Mercury levels in maternal and cord blood and attained weight through the 24 months of life. Sci Total Environ 2011; 410–411:26–33. [DOI] [PubMed] [Google Scholar]
- 23.Korean Nutrition Society. Dietary Reference Intakes for Koreans. 1st revision. Seoul: Korean Nutrition Society; 2010. [Google Scholar]
- 24.Schnaas L, Rothenberg SJ, Flores MF, et al. Reduced intellectual development in children with prenatal lead exposure. Environ Health Perspect 2006; 114:791–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu H, Téllez-Rojo MM, Bellinger D, et al. Fetal lead exposure at each stage of pregnancy as a predictor of infant mental development. Environ Health Perspect 2006; 114:1730–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldstein GW. Lead poisoning and brain cell function. Environ Health Perspect 1990; 89:91–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goyer RA. Transplacental transport of lead. Environ Health Perspect 1990; 89:101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herschkowitz N. Brain development in the fetus, neonate and infant. Neonatology 1988; 54:1–19. [DOI] [PubMed] [Google Scholar]
- 29.Larsen WJ. Development of the brain and cranial nerves. Human Embryology 2nd ed.New York: Churchill Livingston; 1997. 411–454. [Google Scholar]
- 30.Reddy YS.F YA, Ramalaksmi BA, Kumar BD. Lead and trace element levels in placenta, maternal and cord blood: a cross-sectional pilot study. J Obstet Gynaecol Res 2014; 40:2184–2190. [DOI] [PubMed] [Google Scholar]
- 31.Petit TL, LeBoutillier JC. Effects of lead exposure during development on neocortical dendritic and synaptic structure. Exp Neurol 1979; 64:482–492. [DOI] [PubMed] [Google Scholar]
- 32.Chen Y, Yu D, Wei Q, et al. Effect of lead exposure on synaptic structural plasticity in the hippocampus of postnatal Wistar rat [in Chinese]. Wei Sheng Yan Jiu 2012; 41:394–398. [PubMed] [Google Scholar]
- 33.Lidsky TI, Schneider JS. Lead neurotoxicity in children: basic mechanisms and clinical correlates. Brain 2003; 126 (Pt 1):5–19. [DOI] [PubMed] [Google Scholar]
- 34.Webb SJ, Monk CS, Nelson CA. Mechanisms of postnatal neurobiological development: implications for human development. Dev Neuropsychol 2001; 19:147–171. [DOI] [PubMed] [Google Scholar]
- 35.Freedman R, Olson L, Hoffer BJ. Toxic effects of lead on neuronal development and function. Environ Health Perspect 1990; 89:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheong JH, Bannon D, Olivi L, et al. Different mechanisms mediate uptake of lead in a rat astroglial cell line. Toxicol Sci 2004; 77:334–340. [DOI] [PubMed] [Google Scholar]
- 37.Todorich B, Pasquini JM, Garcia CI, et al. Oligodendrocytes and myelination: the role of iron. Glia 2009; 57:467–478. [DOI] [PubMed] [Google Scholar]
- 38.Deng W, McKinnon RD, Poretz RD. Lead exposure delays the differentiation of oligodendroglial progenitors in vitro. Toxicol Appl Pharmacol 2001; 174:235–244. [DOI] [PubMed] [Google Scholar]
- 39.Dabrowska-Bouta B, Sulkowski G, Bartosz G, et al. Chronic lead intoxication affects the myelin membrane status in the central nervous system of adult rats. J Mol Neurosci 1999; 13:127–139. [DOI] [PubMed] [Google Scholar]
- 40.Erikson KM, Jones BC, Hess EJ, et al. Iron deficiency decreases dopamine D1 and D2 receptors in rat brain. Pharmacol Biochem Behav 2001; 69:409–418. [DOI] [PubMed] [Google Scholar]
- 41.Hong YC, Kulkarni S, Lim YH, et al. Postnatal growth following prenatal lead exposure and calcium intake. Pediatrics 2014; 134:1151–1159. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


