Abstract
A single incisional laparoscopic surgery (SILS) approach is increasingly being used, taking advantage of the minimally invasive technique. The aim of this study was to evaluate the feasibility and the validation of SILS procedure for small bowel obstruction (SBO).
Sixteen consecutive patients with SBO who underwent SILS release of ileus between April 2010 and March 2015 were compared with the conventional multiport laparoscopic treatment group of 16 patients matched for age, gender, and surgical procedure.
Laparoscopic treatment was completed in a total of 14 patients in SILS group and 13 in multiport laparoscopic group. Two cases and 3 cases were converted to multiport laparoscopic surgery or open surgery. Eight patients with nonscar and nonadhesive ileus, such as internal hernia, obturator hernia, gallstone ileus, and intestinal invagination, were treated successfully in the laparoscopic procedure. There was no mortality in either of the groups. The mean procedural time was 105 minutes in the SILS group and 116 minutes in the multiport laparoscopic group. The mean amount of blood loss was not statistically different in either of groups (15 ml vs. 23 ml). Patients resumed oral intake after a mean of 2 days in the SILS and 3 days in the multiport groups with the statistically difference. The length of hospital stay was shorter in the SILS group (5 days vs. 7 days) with no statistically difference. Perioperative morbidity was seen in 2 patients in the SILS group and 3 patients in the multiport group.
SILS approach has superior and/or similar perioperative outcomes to multiport approach for SBO. SILS release of ileus as an ultra-minimal invasion technique is feasible, effective, and offers benefits with cosmesis in simple adhesive or scar-less nonadhesive ileus patients.
INTRODUCTION
Laparoscopy has been regarded as contraindicated in patients with previous abdominal surgery because adhesions make dissection more difficult and because there is a higher risk of accidental bowel perforation. However, the case of 1 patient in whom a single band responsible for small bowel obstruction (SBO) was lysed via a laparoscopic approach was reported in 1991 by Bastug et al.1 Since then, the surgical management of SBO has been notable for the increasing familiarity of general surgeons with laparoscopy.
Abdominal exploration in any type of surgery may potentially form fibrous adhesions or bands, leading to obstructive structures, and has been observed in approximately 95% of patients.2 Subsequently, the most frequent causes of SBO result from such structures.3,4 Some investigators have reported that adhesive SBO occurs in 3% of laparotomies, with 1% occurring in the first postoperative year.5,6 After operating on postoperative adhesive SBO, a risk of recurrence remains, and the literature reports a rate of overall recurrence ranging widely from 3 years to longer.3,7–10
At present, laparoscopic surgery is known to have many advantages, including minimalized invasiveness due to the need of smaller incisions, less influence on body temperature, reduced formation of adhesions, and lower risk of intraabdominal contamination. Laparoscopic treatment of ileus for SBO is being performed more often with the hope of reducing morbidity and shortening the hospital stay.11–16 Our previous study was consistent with other reports.17 Furthermore, use of single incision laparoscopic surgery (SILS) has recently emerged as an attempt to further improve the cosmetic advantages and decrease the morbidity of minimally invasive surgery.18,19 This approach ultimately might lead to scar-less operation, such as NOTES (natural orifice transluminal endoscopic surgery), and led us to attempt SILS approach.
In the present study, we evaluated the feasibility and validation of SILS ileus releasing of SBO and compared the SILS and multiport laparoscopic approaches for the treatment of this common entity.
PATIENTS AND METHODS
Forty-five consecutive patients with postoperative SBO were treated by laparoscopic operation at the Department of Surgery of Tsuru Municipal Hospital between January 2004 and March 2015. Data from 45 consecutive patients treated by laparoscopic ileus operations was collected and analyzed. Sixteen patients with SBO who underwent SILS ileus releasing between April 2010 and March 2015 were compared with the conventional multiport laparoscopic treatment group of 16 patients matched for age, gender, and surgical procedure. This study was conducted and approved in accordance with the ethical principles outlined in the Declaration of Helsinki.20 All the patients provided written informed consent before the initiation of the study. The authors include 2 surgeons who operated consecutively during the study period.
SBO was clinically diagnosed by patient history, physical examination, blood tests, and X-ray examinations. Preoperative abdominal contrast-enhanced computed tomography (CT) scans were performed in transverse, coronal and sagittal views. In 30 of the 45 patients, a long decompression tube was inserted nasally, and a small bowel contrast series was obtained after achieving small intestine decompression. The location of the obstructed or stenotic region was predicted for the subsequent laparoscopic procedure from these images.
The decision to use a laparoscopic approach for mechanical SBO was made based on each surgeon's experience with laparoscopy and on the availability of equipment.
After the patient was placed in the supine position under general anesthesia, pneumoperitoneum at 10 mm Hg was established following placement of an initial 12 mm trocar through a 1.5 cm longitudinal incision in an area without former surgical incisions. The incision was often made in the left upper quadrant or in the umbilicus. The SILS port or EZ access (Hakko Medical Co., Nagano, Japan) was placed in the left or right side of the abdomen through a 2.5 cm skin incision, in which the fibrous adhesion was located at the midline of the incision. When the adhesion was located at the left or right side of the abdomen and/or nonscar nonadhesive ileus, SILS, or EZ access port was placed in the umbilicus. When the operator decided that it was impossible to complete the releasing of the ileus, a 5 mm trocar was added. In the multiport laparoscopic approach, two additional trocars (5 or 10 mm) were then placed by intraabdominal findings and the location of adhesions in such a way as to provide good triangulation between the instruments and to allow for optimal placement of the camera. A flexible steerable laparoscope and forceps were used to overcome possible technical difficulties of the laparoscopic procedure.
The small bowel was examined proximally starting from the ileocecal valve, whenever possible. If an adhesive band was found to be possibly responsible for the obstruction or stenosis, it was cut and dissected with scissors, sometimes after bipolar coagulation or use of a Harmonics scalpel (Johnson & Johnson, Cincinnati, OH, USA). If multiple adhesions were identified, they were released as best as possible. The entire small bowel was then investigated to confirm relief of ileus by the surgeon.
Conversion to open laparotomy was performed if accidental bowel perforation with possible peritoneal contamination occurred, when bowel necrosis was found, or when release of ileus was deemed too difficult due to the presence of diffuse adhesions. Intestinal injuries with only minor leakage of contents or sero-muscular tears were sutured laparoscopically.
Multiple factors were assessed, including age, gender, previous operation, adhesion site, and cause of obstruction. Operation time, amount of blood loss, initial day of liquid or solid food intake, length of postoperative hospital stay, morbidity, and mortality were evaluated and compared between the SILS and multiport laparoscopic surgery groups. Recorded complications were also evaluated, including prolonged ileus (no oral intake for more than 7 days), pneumonia, ventral incisional hernia, and surgical site infection presenting as local pain, redness, and drainage of cloudy fluid from the incision wound.
Data are expressed as the means and ranges for each variable. The t test (2-tailed) and χ2 test were used to assess the significance of differences between the 2 groups, with P < 0.05 considered as a significant difference.
RESULTS
Demographic data of laparoscopic treatment are summarized in Table 1. The multiport group matched the SILS group for age, gender, and surgical procedure in the case–control analysis. In the SILS cases, previous operations were gastrectomy in 5 patients, cholecystectomy in 4 patients, sigmoidectomy in 1 patient, anterior resection of the rectum in 1 patient, gynecologic procedure in 1 patient, and no abdominal operations in 4 patients. In the multiport surgery, previous operations were as follows: appendectomy in 2 patients, gastrectomy in 8 patients, cholecystectomy in 1 patient, gynecologic procedure in 1 patient, no abdominal operations in 4 patients. Diseases necessitating the original laparotomy in the SILS cases were for gastric cancer and gastric ulcer in the gastrectomies, acute cholecystitis in the cholecystectomies, sigmoid colon cancer in the sigmoidectomy, rectal cancer in the low anterior resection, and uterine fibroids in the histerectomy. The original laparotomies in the multiport surgery cases were for acute appendicitis in the case of appendectomy, gastric cancer in the gastrectomies, acute cholecystitis in the cholecystectomies, uterine fibroids in the gynecological operation.
TABLE 1.
Demographic Data of Laparoscopic Treatment
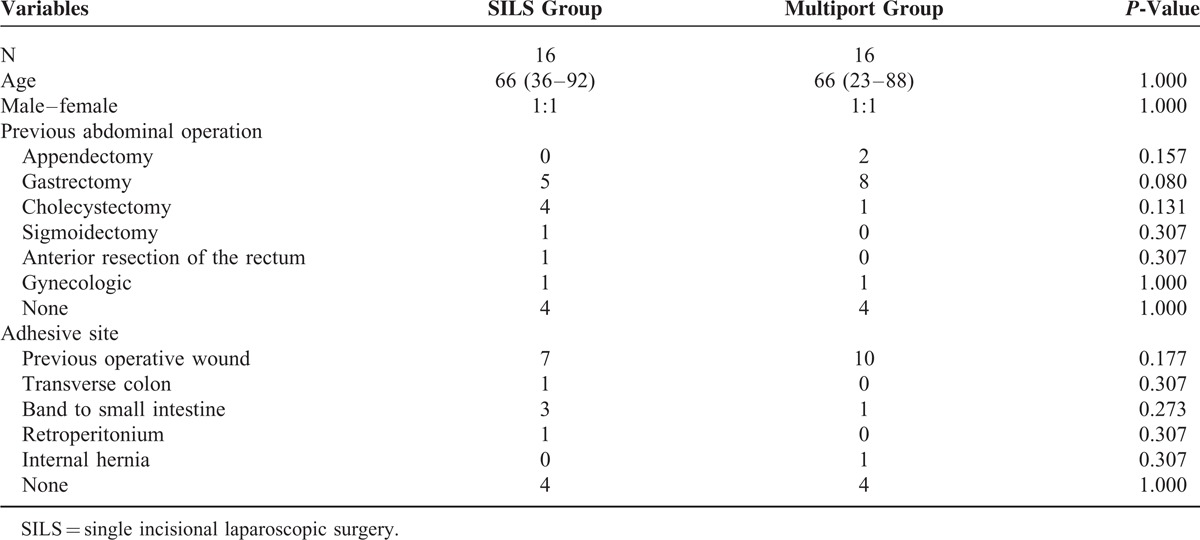
Possible causes of obstruction are as follows. In the SILS group, 7 patients had small intestinal adhesions to a previously incised abdominal wall. One patient had small intestinal adhesions between the transverse colon and omentum. Three patients had adhesion bands to the small bowel, and 1 was stick adhesions to the small bowel. One patient had small intestine adhesions to the retroperitoneum. Four patients had never undergone operation. In the multiport laparoscopic group, 10 patients had adhesions to a previously incised abdominal wall. One patient had fibrous bands involving the small intestine. One patient had an internal hernia due to the fibrous band. Four patients had never undergone operation.
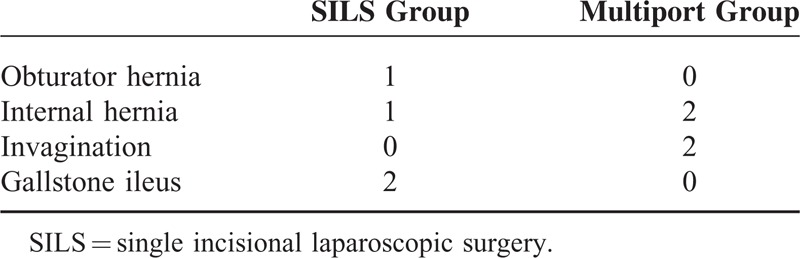
Contents of nonadhesive ileus without previous operation are indicated in Table 2. In the SILS group, 1 patient had SBO by obturator hernia and 1 patient had the obstruction by internal hernia by appendix epiploica of the sigmoid colon. Other 2 patients had gall stone ileus. In the multiport group, 2 patients had internal hernia without previous operation such as trans-mesosigmoid hernia, volvulus of the sigmoid colon. Other 2 patients had intestinal invaginations.
TABLE 2.
Contents of Nonadhesive and Nonscar Ileus
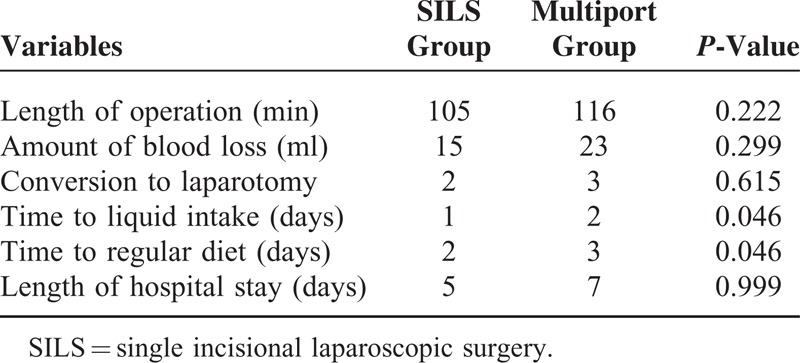
The results after surgery are presented in Table 3. The mean surgical times were 105 minutes in the SILS group and 116 minutes in the multiport laparoscopic group; the difference was not statistically significant. The amount of blood loss was 15 and 23 ml, respectively, with no significantly difference. Fourteen patients of the SILS group were completed entirely single incisional laparoscopically for the relief of ileus. Time to liquid intake and time to resumption of a regular diet, return of bowel function, in the SILS group were significant shorter than in the multiport group with statistically difference. The mean length of hospital stay of SILS group was 5 days whereas that of the multiport laparoscopic group was 7 days without statistical differences.
TABLE 3.
Surgical Outcomes
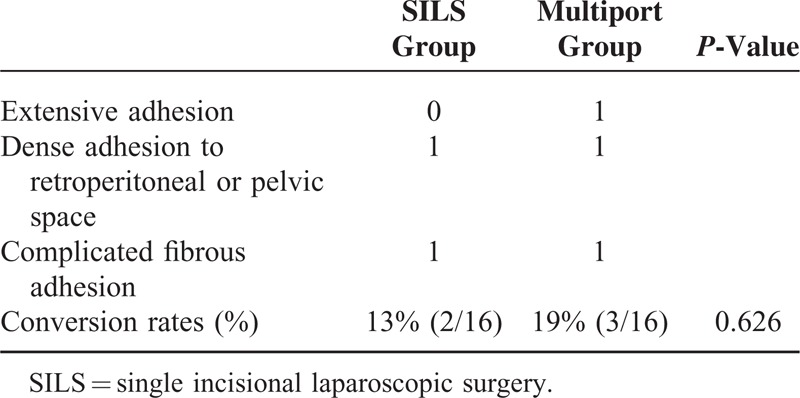
Details of conversion cases are shown in Table 4. One case was converted to open laparotomy and another 1 was done to multiport surgery in the SILS group. The reasons for conversion in the 2 SILS group cases were as follows: dense adhesions to a retroperitoneal space, and complicated fibrous adhesions. Three patients were converted to open laparotomy in the multiport group. Those for the 3 cases in the multiport group were extensive adhesions to the previous incision site, dense adhesions to a previous pelvic wound, and complicated fibrous adhesions. All cases were required for intestinal partial resection. We could not find the significant differences in conversion rate of the each group.
TABLE 4.
Conversion Cases
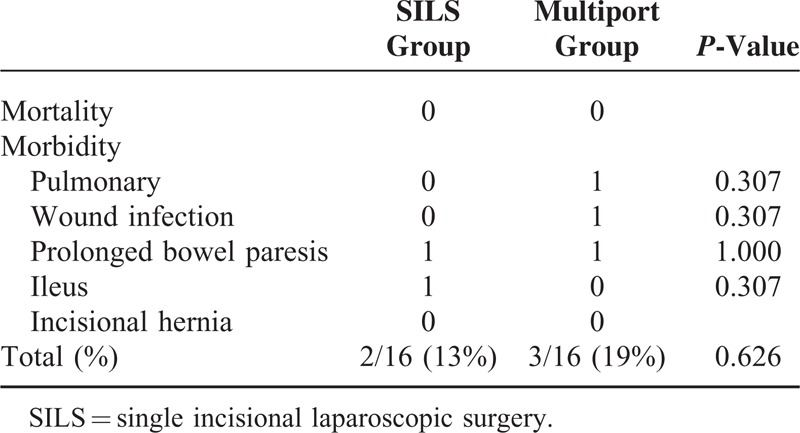
Perioperative mortality and morbidity are shown in Table 5. There was no perioperative mortality in either group. Postoperative pulmonary complications were not observed in the SILS group whereas one pulmonary complication was done in the multiport laparoscopic surgery group. This patient had chronic obstructive pulmonary disease. Surgical site infections were seen only in the multiport laparoscopic surgery group. Prolonged bowel paralysis was observed in the both SILS and multiport laparoscopic surgery groups. Postoperative ileus was found in one case in the SILS group, caused by a newly formed complicated adhesive site at the dissected lesion from the previous adhesiolysis. This case was converted to multiport surgery with intestinal resection. There are no incisional hernias in the both groups. The overall rates of complications contributing to morbidity were not significantly different in patients who underwent laparoscopic surgery by SILS or by multiport laparoscopic surgery.
TABLE 5.
Mortality and Morbidity
DISCUSSION
Since the introduction and adoption of minimally invasive surgery, the role of laparoscopy in the management of SBO has gradually received more attention.1,11–16 Our previous study demonstrated that multiport laparoscopic adhesiolysis is effective and useful in selected patients.17 The present study showed that surgical outcomes in the SILS group, such as time to liquid intake and/or regular diet were superior to those in conventional multiport laparoscopy, although the outcomes of surgical time, blood loss, and length of stay in the SILS group were similar to those in the multiport group. This result indicates that SILS approach is also feasible and brings the benefit of improved patient outcomes. Furthermore, we have reported for the first time that SILS release of the ileus was useful and effective for not only adhesive ileus but also scar-less nonadhesive ileus, such as internal hernia, intestinal invagination. Especially, SILS release of the ileus brought the cosmetic benefits in scar-less nonadhesive ileus cases.
It has been reported that postoperative intraabdominal adhesions account for 60% to 80% of ileus cases,2,8,21 emphasizing the importance of resolving this disorder. Conventional open surgery, which is both the cause of obstructions and the definitive procedure for adhesiolysis or resection, has been the standard therapy for this disease. However, disadvantages of a large abdominal incision include growing postoperative pain, prolonged intestinal paresis, wound infection, ventral incisional hernia, and poor cosmesis. Furthermore, operation in patients with adhesions carries the risk of causing more adhesions. Accordingly, it becomes more difficult and more dangerous to perform successive operations. On the other hand, it has been reported that laparoscopic surgery may result in fewer postoperative adhesions than open surgery.22,23
Laparoscopic release of multiple dense adhesions or adhesiolysis may be difficult in some cases, and conversion to open surgery may be necessary due to the limitation of retroposterior view or a smaller pelvic cavity.16 In the present series, multiple fibrous adhesions, dense adhesions, and extensive broad adhesions were difficult to release laparoscopically, and conversion to open surgery was required in some cases. In our SILS cases, dense adhesion to the retroperitoneal space and complicated fibrous adhesions were converted to multiport surgery and open surgery, respectively. In such cases, surgeons should not hesitate to convert to multiport procedure and/or the conventional open surgery. Accordingly, the conversion rate has been reported to be from 6.2% to 52%.8,15,24–27 Our conversion rates were 13% in the SILS group and 19% in the multiport group. Although forceps movement is restricted by a single-port, the conversion rate of the either group was not significant different. In particular, SILS is a possible technique when a single adhesive band or scar-less nonadhesive ileus is responsible for SBO.
There are few studies indicating complications between laparoscopic and conventional surgeries. However, more frequent complications have been shown to occur after converted surgeries than after completed laparoscopic procedures for treatment of ileus.15,25 It has been shown in a previous study that patients in whom a laparoscopic procedure was intended had fewer postoperative complications. Furthermore, laparoscopic treatments carry some advantages, including quicker bowel function recovery and a shorter hospital stay, than conventional approach. The present study indicated the SILS approach has similar advantages, quicker bowel function recovery, and also showed that operative complications in the SILS group, such as postoperative pneumonia, wound infection, postoperative bowel paresis, and ventral incisional hernia were similar to those in the multiport laparoscopic group.
In conclusion, SILS release of the ileus as well as laparoscopic multiport surgery is feasible, effective, and safety for the management of mechanical SBO in selected patients, especially with simple adhesive or nonadhesive ileus. We had only a small number of our SILS cases so far; further accumulation studies are required. Ideally, a randomized control trial should be set out for comparison.
Footnotes
Abbreviations: CT = computed tomography, NOTES = natural orifice transluminal endoscopic surgery, SBO = small bowel obstruction, SILS = single incisional laparoscopic surgery.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Bastug DF, Trammel SW, Boland JP, et al. Laparoscopic adhesiolysis for small bowel obstruction. Surg Laparosc Endosc 1991; 1:259–262. [PubMed] [Google Scholar]
- 2.Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 1999; 353:1476–1480. [DOI] [PubMed] [Google Scholar]
- 3.Mucha P., Jr Small intestinal obstruction. Surg Clin North Am 1987; 67:597–620. [DOI] [PubMed] [Google Scholar]
- 4.Miller G, Boman J, Shrier I, et al. Etiology of small bowel obstruction. Am J Surg 2000; 180:33–36. [DOI] [PubMed] [Google Scholar]
- 5.Menzies D, Ellis H. Intestinal obstruction from adhesions: how big is the problem? Ann R Coll Surg Engl 1990; 72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 6.Menzies D. Peritoneal adhesions: incidence, cause, and prevention. Surg Annu 1992; 24:27–45. [PubMed] [Google Scholar]
- 7.Landercasper J, Cogbill TH, Merry WH, et al. Long-term outcome after hospitalization for small-bowel obstruction. Arch Surg 1993; 128:765–770. [DOI] [PubMed] [Google Scholar]
- 8.Miller G, Boman J, Shriner I, et al. Natural history of patients with adhesive small bowel obstruction. Br J Surg 2000; 87:1240–1247. [DOI] [PubMed] [Google Scholar]
- 9.Fevang BT, Fevang J, Lie SA, et al. Long-term prognosis after operation for adhesive small bowel obstruction. Ann Surg 2004; 240:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barkan H, Webster J, Ozeran S. Factors predicting the recurrence of adhesive small-bowel obstruction. Am J Surg 1995; 170:361–365. [DOI] [PubMed] [Google Scholar]
- 11.León EL, Metzger A, Tsiotos GC, et al. Laparoscopic management of small bowel obstruction: indications and outcome. J Gastrointest Surg 1998; 2:132–140. [DOI] [PubMed] [Google Scholar]
- 12.Navez B, Arimont JM, Guiot P. Laparoscopic approach in acute small bowel obstruction. A review of 68 patients. Hepatogastroenterology 1998; 45:2146–2150. [PubMed] [Google Scholar]
- 13.Suter M, Zermatten P, Halkic N, et al. Laparoscopic management of mechanical small bowel obstruction: are there predictors of success or failure? Surg Endosc 2000; 14:478–483. [DOI] [PubMed] [Google Scholar]
- 14.Kirshtein B, Roy-Shapira A, Lantsberg L, et al. Laparoscopic management of acute small bowel obstruction. Surg Endosc 2005; 19:464–467. [DOI] [PubMed] [Google Scholar]
- 15.Borzellino G, Tasselli S, Zerman G, et al. Laparoscopic approach to postoperative adhesive obstruction. Surg Endosc 2004; 18:686–690. [DOI] [PubMed] [Google Scholar]
- 16.Chopra R, McVay C, Phillips E, et al. Laparoscopic lysis of adhesions. Am Surg 2003; 69:966–968. [PubMed] [Google Scholar]
- 17.Okamoto H, Wakana H, Kawashima K, et al. Clinical outcomes of laparoscopic adhesiolysis for mechanical small bowel obstruction. Asian J Endosc Surg 2012; 5:53–58. [DOI] [PubMed] [Google Scholar]
- 18.Bessler M, Stevens PD, Milone L, et al. Transvaginal laparoscopically assisted endoscopic cholecystectomy: a hybrid approach to natural orifice surgery. Gastrointest Endosc 2007; 66:1243–1245. [DOI] [PubMed] [Google Scholar]
- 19.Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis 2008; 23:1013–1016. [DOI] [PubMed] [Google Scholar]
- 20.American society of Clinical Oncology. Good clinical practice research guidelines reviewed, emphasis given to responsibilities of investigators: second article in a series. J Oncol Pract 2008; 4:233–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellis H. The clinical significance of adhesions: focus on intestinal obstruction. Eur J Surg Suppl 1997; 577:5–9. [PubMed] [Google Scholar]
- 22.Garrard CL, Clements RH, Nanncy L, et al. Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 1999; 13:10–13. [DOI] [PubMed] [Google Scholar]
- 23.Wullstein C, Gross E. Laparoscopic compared with conventional treatment of acute adhesive small bowel obstruction. Br J Surg 2003; 90:1147–1151. [DOI] [PubMed] [Google Scholar]
- 24.Berzellino G, Manzoni GD, Ricci F. Detection of abdominal adhesions in laparoscopic surgery. A controlled study of 130 cases. Surg Laparosc Endosc 1998; 8:273–276. [PubMed] [Google Scholar]
- 25.Levard H, Boudet MJ, Msika S, et al. Laparoscopic treatment of acute small bowel obstruction: a multicentre retrospective study. Aust N Z J Surg 2001; 71:641–646. [DOI] [PubMed] [Google Scholar]
- 26.Sato Y, Ido K, Kumagai M, et al. Laparoscopic adhesiolysis for recurrent small bowel obstruction: long-term follow-up. Gastrointest Endosc 2001; 54:476–479. [DOI] [PubMed] [Google Scholar]
- 27.Franklin ME, Jr, Dorman JP, Pharand D. Laparoscopic surgery in acute small bowel obstruction. Surg Laparosc Endosc 1994; 4:289–296. [PubMed] [Google Scholar]


