Abstract
While risky sexual behaviours related to illicit drug use among street youth have been explored, the impacts of alcohol use have received less attention. This longitudinal study examined hazardous alcohol use among a population of street-involved youth, with particular attention to sexual and drug-related risk behaviours. Data were derived from the At-Risk Youth Study, a prospective cohort of street-involved youth in Vancouver, Canada. The outcome of interest was hazardous alcohol use defined by the US National Institute on Alcohol Abuse and Alcoholism. We used generalized estimating equations (GEEs) analyses to identify factors associated with hazardous alcohol use. Between 2005 and 2014, 1149 drug-using youth were recruited and 629 (55%) reported hazardous alcohol use in the previous 6 months during study follow-up. In multivariable GEE analyses, unprotected sex (adjusted odds ratio [AOR] = 1.28, 95% confidence interval [95% CI] = 1.12–1.46) and homelessness (AOR = 1.35, 95% CI = 1.19–1.54) were independently associated with hazardous alcohol use (all p < .001). Older age (AOR = 0.95, 95% CI = 0.92–0.99), Caucasian ethnicity (AOR = 0.74, 95% CI = 0.61–0.90), daily heroin use (AOR = 0.53, 95% CI = 0.42– 0.67), daily crack cocaine smoking (AOR = 0.73, 95% CI = 0.59–0.91), and daily crystal methamphetamine use (AOR = 0.52, 95% CI = 0.42–0.64) were negatively associated with hazardous alcohol use (all p < .05). In sub-analysis, consistent dose–response patterns were observed between levels of alcohol use and unprotected sex, homelessness, and daily heroin injection. In sum, hazardous alcohol use was positively associated with unsafe sexual behaviour and negatively associated with high-intensity drug use. Interventions to address hazardous alcohol use should be central to HIV prevention efforts for street-involved youth.
Keywords: Hazardous drinking, injection drug use, HIV, youth, homelessness
INTRODUCTION
Alcohol use is a major cause of morbidity and mortality worldwide. Health consequences secondary to chronic hazardous alcohol use include liver cirrhosis, cardiovascular disease, and cancers (Baan et al., 2007; Rehm et al., 2010; Singh et al., 2013). Harms related to acute intoxication include accidents, interpersonal violence and sexual risk behaviour, often occurring in youth (Cherpitel, 2013; Taylor et al., 2010). Alcohol use disorders are most prevalent in young adulthood (18–29 years) (Grant et al., 2015). Alcohol is the main risk factor contributing to the global burden of disease and outweighs the impacts of tobacco smoking and illicit drug use among young adults (Gore et al., 2011).
In North America, alcohol is the most commonly used psychoactive substance among youth based on nationwide surveys (Health Canada, Office of Research and Surveillance, Controlled Substances and Tobacco Directorate, 2015; Substance Abuse and Mental Health Services Administration, 2014). Past year alcohol consumption was reported by 70% of Canadian youth, who were more likely than adults to exceed safer drinking recommendations (Health Canada, Office of Research and Surveillance, Controlled Substances and Tobacco Directorate, 2015). However, survey-based research often fails to capture socially and economically disadvantaged populations including street-involved youth – that is, young adults who spend all or part of their time working or living on the street (Farrow, Deisher, Brown, Kulig, & Kipke, 1992).
Street-involved youth are an important population to capture, as they are known to be at risk of numerous health harms. High rates of HIV-risk behaviour related to drug use behaviours have been documented in street-involved youth, including high-intensity drug-use patterns and syringe sharing (Lloyd-Smith, Kerr, Zhang, Montaner, & Wood, 2008; Roy et al., 2003). Further, sexual risk behaviours such as reporting multiple sex partners and inconsistent condom use, as well as higher documented rates of sexually transmitted infections (STIs) have been identified among street- involved youth (Halcon & Lifson, 2004; Milburn, Rotheram-Borus, Rice, Mallet, & Rosenthal, 2006).
While sexual and drug-related risk behaviours have been commonly studied among street-involved youth (Ehrenstein, Horton, & Samet, 2004; Tucker et al., 2012; Tyler & Melander, 2010), the associations between alcohol and sexual and drug-related HIV-risk behaviours have received substantially less attention (Cheng, Johnston, et al., 2016; Mackesy-Amiti, Donenberg, & Ouellet, 2012). This is surprising given that the prevalence of alcohol use and alcohol use disorders is highest during young adulthood (Gore et al., 2011; Grant et al., 2015). Furthermore, in one study involving a cohort of street- involved youth in Montreal, daily alcohol use was a predictor of premature mortality (Roy et al., 2004), underscoring the need to understand the role of hazardous alcohol use in this population.
Thus, the purpose of this longitudinal study was to examine hazardous alcohol use among a cohort of street-involved youth in Vancouver, Canada. We hypothesized that hazardous alcohol use would be associated with increased sexual risk behaviours, but not drug-related, HIV-related risk among street- involved youth. Therefore, particular attention was paid to associations with sexual risk behaviours and drug-use practices in order to identify potentially modifiable HIV risk behaviours among street-involved youth.
METHODS
Participants and recruitment
Data for this study were collected from the At-Risk Youth Study (ARYS), a prospective cohort of street-involved youth in Vancouver, Canada. The study has previously been described in detail (Wood, Stoltz, Montaner, & Kerr, 2006). In brief, participants were recruited through extensive street-based outreach and snowball sampling. Eligibility criteria included (1) youth between the ages of 14 and 26 at enrolment, (2) use of an illicit drug other than marijuana in the past 30 days, (3) provision of written informed consent, and (4) street-involved, defined as being absolutely or temporarily without stable housing, or having accessed street-based youth services in past 6 months. Similar conditions have previously been used to define street-involvement among youth (Boivin, Roy, Haley, & Galbaud du Fort, 2005; DeMatteo et al., 1999).
Procedure
At baseline and every six months thereafter, participants completed an interviewer-administered questionnaire pertaining to socio-demographic information, sex- and drug-related risk behaviours including specific drugs used and modes of use. At every visit, participants also provided blood samples in order to ascertain HIV and hepatitis C infection status and received $30 CAD as remuneration. Data for this analysis were collected from September 2005 to May 2014.
Survey measures
The primary outcome in our analysis was “hazardous alcohol use” defined as National Institute on Alcohol Abuse and Alcoholism (NIAAA) risky alcohol use, specifically, >14 drinks/week or >4 drinks on one occasion for men and >7 drinks/week or >3 drinks on one occasion for women (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2007). A standard drink is defined as one 12-ounce bottle of beer, one 5-ounce glass of wine, or 1.5 ounces of distilled spirits (NIAAA, 2007).
Socio-demographic explanatory variables of interest included age at baseline (treated as a continuous variable per additional year older), gender (female vs. male), Caucasian ethnicity (yes vs. other), and homelessness in the previous six months (yes vs. no). Drug use variables of interest referring to behaviours in the previous six months included non-fatal overdose, daily crystal methamphetamine use (injection or non-injection), daily crack cocaine smoking, daily cocaine use (injection or non-injection), daily heroin use (injection or non-injection), and syringe sharing, defined as using a syringe that has already been used by someone else or lending a used syringe to someone else. Other variables of interest included unprotected sex, defined as vaginal or anal sex without use of a condom in the past 6 months, self-reported history of any diagnosed STIs in the last six months, same sex oral or anal sexual activity among men (one or more encounters vs. none), engagement in sex work, defined as the provision of sexual services in exchange for needed items such as money, food, or shelter (yes vs. no), and incarceration, defined as being in detention, prison, drunk tank, or jail in the previous six months (yes vs. no). These time-updated variables referred to exposures occurring in the six-month period prior to each study interview. “Female” gender and all “yes” responses were coded as 1 and “male” gender and all “no” responses were coded as 0 in the analyses. All drug use and sexual risk behaviours were coded as dichotomous (yes vs. no).
Statistical analysis
First, we examined baseline characteristics from participants’ first study visit, stratified by hazardous alcohol use, using Pearson’s χ2 test and Wilcoxon rank sum test. Second, we examined hazardous alcohol use in the past six months during study follow-up using generalized estimating equations (GEEs) with a logit link function and an exchangeable correlation structure for the analysis of correlated data (Johnston, Callon, Li, Wood, & Kerr, 2010). In order to adjust for potential confounding in the multivariable GEE analysis, variables significant at the p < .10 threshold in bivariable analyses were used in the backwards model selection process. The model with the best overall fit was determined by the lowest quasi-likelihood under the independence model criterion value (Cui, 2007).
In sub-analysis to assess whether varying intensities of alcohol use were associated with sexual and drug-related risk behaviours, we created four categories of alcohol use. The reference category “light drinking” included all individuals who did not fulfil criteria for hazardous alcohol use and reported a daily drinking average during the last week of ≤2 drinks for women or ≤3 drinks for men. We defined “moderate drinking”, “heavy drinking”, and “very heavy drinking” exposure groups based on the median number of drinks per day during the past week (8 for women and 10 for men) reported among hazardous drinkers: (1) “moderate drinking” included individuals who did not fulfil criteria for hazardous alcohol use and reported a daily drinking average during the last week of >2 drinks for women and >3 drinks for men; (2) “heavy drinking” included individuals who did fulfil criteria for hazardous alcohol use and reported a daily drinking average during the last week <8 for women or <10 for men; and (3) “very heavy drinking” included individuals who reported hazardous alcohol use and reported a daily drinking average during the last week ≥8 for women OR ≥10 for men. We constructed three GEE models, comparing each exposure group with the reference group. Individuals who contributed multiple observations during the study period contributed observations to more than one category when intensity of alcohol use changed over time. The same explanatory variables of interest were included in bivariable analyses and those significant at the p < .10 threshold for each exposure group were included in the fixed multivariable models.
All statistical analyses were performed using the SAS software version 9.4 (SAS Institute, Cary, NC), and all p-values are two-sided.
RESULTS
Sample characteristics
A total of 1149 youth were recruited into the ARYS cohort from September 2005 to May 2014. At study entry, among this sample, the median age was 21 years (interquartile range [IQR] 19–23 years), 359 (31%) were female, 780 (68%) were Caucasian, and 852 (74%) had been homeless during last 6 months (Table 1). The median number of study visits per participant was 3 (IQR = 1–5). For the 796 participants who had more than one study visit, the median follow-up time per participant was 24.5 months (IQR = 13.3–52.9). This sample contributed 4343 observations, of which 1493 (34%) included a report of hazardous alcohol use.
Table 1.
Baseline characteristics of street-involved youth stratified by hazardous alcohol use (n = 1149).
| Hazardous alcohol use | ||||
|---|---|---|---|---|
| Characteristic | Yes n = 423 (36.8%) |
No n = 726 (63.2%) |
OR (95% CI) | p-Value |
| Median age (IQR) | 21 (19–23) | 21 (20–23) | 0.95 (0.91–0.99) | .025 |
| Gender | ||||
| Female | 131 (31.0) | 228 (31.4) | 0.98 (0.76–1.27) | .878 |
| Male | 292 (69.0) | 498 (68.6) | ||
| Caucasian ethnicity | ||||
| Yes | 272 (64.3) | 508 (70.0) | 0.77 (0.60–1.00) | .047 |
| Other | 151 (35.7) | 218 (30.0) | ||
| Homelessnessb | ||||
| Yes | 301 (71.2) | 551 (75.9) | 0.79 (0.60–1.03) | .085 |
| No | 120 (28.4) | 173 (23.8) | ||
| Daily heroin useb,c | ||||
| Yes | 14 (3.3) | 105 (14.5) | 0.21 (0.12–0.36) | <.001 |
| No | 402 (95.0) | 617 (85.0) | ||
| Daily cocaine useb,c | ||||
| Yes | 7 (1.7) | 29 (4.0) | 0.41 (0.18–0.93) | .029 |
| No | 413 (97.6) | 694 (95.6) | ||
| Daily crack cocaine smokingb | ||||
| Yes | 48 (11.4) | 133 (18.3) | 0.58 (0.40–0.82) | .002 |
| No | 372 (87.9) | 592 (81.5) | ||
| Daily crystal methamphetamine useb,c | ||||
| Yes | 28 (6.6) | 115 (15.8) | 0.38 (0.24–0.58) | <.001 |
| No | 392 (92.7) | 606 (83.5) | ||
| Syringe sharingb | ||||
| Yes | 28 (6.6) | 110 (15.2) | 0.40 (0.26–0.62) | <.001 |
| No | 393 (92.9) | 615 (84.7) | ||
| Non-fatal overdoseb | ||||
| Yes | 48 (11.4) | 106 (14.6) | 0.75 (0.52–1.08) | .116 |
| No | 374 (88.4) | 617 (85.0) | ||
| STIsb | ||||
| Yes | 33 (7.8) | 51 (7.0) | 1.12 (0.71–1.77) | .626 |
| No | 390 (92.2) | 675 (93.0) | ||
| Unprotected sexb | ||||
| Yes | 256 (60.5) | 370 (51.0) | 1.46 (1.14–1.87) | .002 |
| No | 163 (38.5) | 344 (47.4) | ||
| Male same sexb,d | ||||
| ≥1 | 21 (7.2) | 40 (8.0) | 0.87 (0.50–1.50) | .611 |
| 0 | 267 (91.4) | 441 (88.6) | ||
| Sex worka | ||||
| Yes | 32 (7.6) | 90 (12.4) | 0.58 (0.38–0.88) | .010 |
| No | 391 (92.4) | 636 (87.6) | ||
| Incarcerationa | ||||
| Yes | 78 (18.4) | 125 (17.2) | 1.09 (0.80–1.49) | .586 |
| No | 341 (80.6) | 596 (82.1) | ||
CI, confidence interval.
All activities refer to the previous six months.
Any route of consumption (i.e., sniffing, snorting, smoking, or injecting).
This variable was restricted to male participants.
At baseline, 423 (37%) youth reported hazardous alcohol use in the last 6 months, and over the study period, a total of 629 (55%) reported hazardous alcohol use. Among participants who reported hazardous alcohol use, the median number of drinks per day during the past week was 10 (IQR = 6–17) overall, 8 (IQR = 5– 15) for women, and 10 (IQR = 8–18) for men. Among 1493 observations which involved a report of hazardous alcohol use, 524 (35%) reported ≤6 drinks per day, 294 (20%) reported 7–11 drinks per day, 309 (20%) reported 12–17 drinks per day, and 366 (25%) reported >17 drinks per day.
Baseline characteristics of the study sample stratified by hazardous alcohol use are presented in Table 1. Individuals who reported hazardous alcohol use had a significantly increased odds of reporting unprotected sex (OR = 1.46, 95% CI = 1.14–1.87) and significantly decreased odds of: being older (OR=0.95, 95% CI= 0.91–0.99); daily heroin use (OR = 0.21, 95% CI = 0.12– 0.36); daily cocaine use (OR=0.41, 95% CI=0.18– 0.93); daily crack cocaine smoking (OR = 0.58, 95% CI = 0.40–0.82); daily crystal methamphetamine use (OR = 0.38, 95% CI = 0.24–0.58); syringe sharing (OR = 0.40, 95% CI = 0.26–0.62); and engagement in sex work (OR = 0.58, 95% CI = 0.38–0.88).
Factors associated with hazardous alcohol use
Bivariable and multivariable GEE analyses of factors associated with hazardous alcohol use are presented in Table 2. In bivariable GEE analysis, individuals who reported hazardous alcohol use had increased odds of being homeless (OR = 1.27, 95% CI = 1.12–1.44) and engaging in unprotected sex (OR = 1.28, 95% CI = 1.13–1.45). Older age (OR = 0.95, 95% CI = 0.92–0.98), Caucasian ethnicity (OR = 0.80, 95% CI = 0.66–0.97), daily heroin use (OR = 0.50, 95% CI = 0.40–0.62), daily crack cocaine smoking (OR = 0.79, 95% CI = 0.64–0.97), daily crystal methamphetamine use (OR = 0.52, 95% CI = 0.43–0.64), and engagement in sex work (OR = 0.73, 95% CI = 0.58–0.91) were negatively associated with hazardous alcohol use in bivariable analyses.
Table 2.
Bivariable and multivariable GEEa analysis of factors associated with hazardous alcohol useb among street-involved youth in Vancouver, Canada (n = 1149).
| Characteristic | Unadjusted odds ratio (95% CIc) |
p-Value | Adjusted odds ratio (95% CIc) |
p-Value |
|---|---|---|---|---|
| Age | ||||
| Per year older | 0.95 (0.92–0.98) | .004 | 0.95 (0.92–0.99) | .008 |
| Caucasian ethnicity | ||||
| (yes vs. other) | 0.80 (0.66–0.97) | .026 | 0.74 (0.61–0.90) | .002 |
| Gender | ||||
| (female vs. male) | 0.85 (0.69–1.04) | .119 | ||
| Homelessnessd | ||||
| (yes vs. no) | 1.27 (1.12–1.44) | <.001 | 1.35 (1.19–1.54) | <.001 |
| Daily heroin used,e | ||||
| (yes vs. no) | 0.50 (0.40–0.62) | <.001 | 0.53 (0.42–0.67) | <.001 |
| Daily cocaine used,e | ||||
| (yes vs. no) | 0.99 (0.64–1.54) | .980 | ||
| Daily crack cocaine smokingd | ||||
| (yes vs. no) | 0.79 (0.64–0.97) | .025 | 0.73 (0.59–0.91) | .005 |
| Daily crystal methamphetamine used,e | ||||
| (yes vs. no) | 0.52 (0.43–0.64) | <.001 | 0.52 (0.42–0.64) | <.001 |
| Non-fatal overdosed | ||||
| (yes vs. no) | 1.11 (0.92–1.35) | .277 | ||
| Syringe sharingd | ||||
| (yes vs. no) | 0.81 (0.65–1.01) | .059 | ||
| STIsd | ||||
| (yes vs. no) | 1.14 (0.89–1.46) | .315 | ||
| Unprotected sexd | ||||
| (yes vs. no) | 1.28 (1.13–1.45) | <.001 | 1.28 (1.12–1.46) | <.001 |
| Male same sexd,f | ||||
| (≥1 vs. 0) | 1.09 (0.79–1.51) | .610 | ||
| Sex workd | ||||
| (yes vs. no) | 0.73 (0.58–0.91) | .006 | 0.78 (0.61–1.00) | .052 |
| Incarcerationd | ||||
| (yes vs. no) | 1.14 (0.97–1.34) | .119 |
GEE, generalized estimating equation.
Hazardous alcohol use >14 drinks per week or >4 drinks on one occasion for men, and >7 drinks per week or >3 drinks on one occasion for women.
CI, confidence interval.
All activities refer to the previous six months.
Any route of consumption (i.e., sniffing, snorting, smoking, or injecting).
Variable restricted to male participants.
In multivariable GEE analysis, unprotected sex (adjusted odds ratio [AOR = 1.28, 95% CI = 1.12–1.46) and homelessness (AOR = 1.35, 95% CI = 1.19–1.54) were independently associated with hazardous alcohol use. Older age (AOR = 0.95, 95% CI = 0.92–0.99), Caucasian ethnicity (AOR = 0.74, 95% CI = 0.61–0.90), daily heroin use (AOR = 0.53, 95% CI = 0.42–0.67), daily crack cocaine smoking (AOR = 0.73, 95% CI = 0.59– 0.91), and daily crystal methamphetamine use (AOR = 0.52, 95% CI = 0.42–0.64) were negatively associated with hazardous alcohol use.
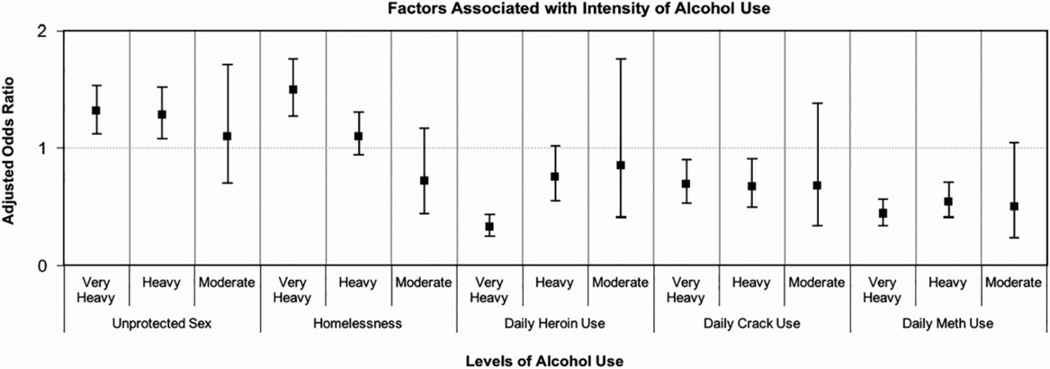
Sub-analysis: dose–response relationship
There were 2765 (64%) observations in the “light drinking” category, 85 (2%) observations in the “moderate drinking” category, 668 (15%) observations in the “heavy drinking” category, and 825 (19%) in the “very heavy drinking” category. Multivariable GEE analyses comparing “moderate drinking”, “heavy drinking”, and “very heavy drinking” with “light drinking” are presented in Table 3 and displayed in Figure 1. A dose– response pattern was observed between unprotected sex and intensity of alcohol use whereby “moderate drinking” was not significantly associated with unprotected sex (AOR = 1.10, 95% CI = 0.70–1.71), but “heavy drinking” (AOR = 1.28, 95% CI = 1.08–1.52) and “very heavy drinking” (AOR = 1.31, 95% CI = 1.12–1.53) were increasingly significantly associated. Similar patterns emerged with homelessness and heroin use. Specifically, the AOR for homelessness increased from 0.72 for “moderate drinking”, to 1.10 for “heavy drinking”, and 1.49 for “very heavy drinking”, while the AOR for daily heroin use decreased from 0.85 for “moderate drinking”, to 0.75 for “heavy drinking”, and 0.33 for “very heavy drinking”. The associations between level of alcohol use and age, crack smoking, and crystal methamphetamine use did not follow a consistent dose–response pattern.
Table 3.
Multivariable GEEa analyses of factors associated with intensity of alcohol useb among street-involved youth in Vancouver, Canada (n = 1149).c
| Characteristicd | Moderatef vs. light drinkinge |
Heavyg vs. light drinkinge | Veryh vs. light drinkinge | |||
|---|---|---|---|---|---|---|
| Adjusted odds ratio (95% CIi) |
p- Value |
Adjusted odds ratio (95% CI) |
p- Value |
Adjusted odds ratio (95% CI) |
p- Value |
|
| Age | ||||||
| Per year older | 0.96 (0.88–1.05) | .344 | 0.95 (0.91–0.99) | .012 | 0.96 (0.92–1.00) | .061 |
| Caucasian ethnicity | ||||||
| (yes vs. other) | 0.79 (0.48–1.31) | .360 | 0.89 (0.71–1.13) | .344 | 0.68 (0.54–0.85) | <.001 |
| Homelessnessj | ||||||
| (yes vs. no) | 0.72 (0.44–1.17) | .186 | 1.10 (0.94–1.30) | .248 | 1.49 (1.27–1.76) | <.001 |
| Incarcerationj | ||||||
| (yes vs. no) | – | – | – | – | 1.33 (1.09–1.62) | .005 |
| Daily heroin usej,k | ||||||
| (yes vs. no) | 0.85 (0.41–1.76) | .660 | 0.75 (0.55–1.02) | .063 | 0.33 (0.25–0.43) | <.001 |
| Daily crack cocaine smokingj |
||||||
| (yes vs. no) | 0.68 (0.34–1.38) | .288 | 0.67 (0.49–0.91) | .011 | 0.69 (0.53–0.90) | .006 |
| Daily crystal methamphetamine usei,j |
||||||
| (yes vs. no) | 0.50 (0.24–1.05) | .066 | 0.54 (0.41–0.71) | <.001 | 0.44 (0.34–0.56) | <.001 |
| Non-fatal overdosej | ||||||
| (yes vs. no) | 0.11 (0.02–0.71) | .020 | – | – | – | – |
| Syringe sharingj | ||||||
| (yes vs. no) | – | – | 0.83 (0.62–1.13) | .238 | – | – |
| Sex workj | ||||||
| (yes vs. no) | 2.59 (1.42–4.75) | .002 | 0.65 (0.46–0.92) | .015 | 0.92 (0.67–1.26) | .612 |
| Unprotected sexj | ||||||
| (yes vs. no) | 1.10 (0.70–1.71) | .679 | 1.28 (1.08–1.52) | .004 | 1.31 (1.12–1.53) | <.001 |
GEE, generalized estimating equation.
Intensity of alcohol use: three separate models for (1) moderate vs. light drinking; (2) heavy vs. light drinking; and (3) and very heavy vs. light drinking.
Separate multivariable models for three separate models, each adjusted for age, gender, ethnicity, homelessness, daily cocaine use, daily crack cocaine use, daily heroin use, daily crystal methamphetamine use, syringe sharing, incarceration, non-fatal overdose, same sex activity in men, unprotected sex, engagement in sex work, and STIs.
All variables significant at the unadjusted level for were included in the multivariable analyses for each model.
Light alcohol use does not fulfil criteria for hazardous alcohol use and also reports drinking 0–2 drinks/day for women or 0–3 drinks/day for men.
Moderate alcohol use does not fulfil criteria for hazardous alcohol use and also reports drinking >2 drinks/day for women OR >3 drinks/day for men.
Heavy alcohol use does fulfil criteria for hazardous alcohol use (>14 drinks per week or >4 drinks on one occasion for men, and >7 drinks per week or >3 drinks on one occasion for women) and also reports <8 drinks/day for women OR <10 drinks per day for men.
Very heavy alcohol use does fulfil criteria for hazardous alcohol use and also reports drinking ≥8 drinks/day for women OR ≥10 drinks per day for men.
CI, confidence interval.
All activities refer to the previous six months.
Any route of consumption (i.e., sniffing, snorting, smoking, or injecting).
Figure 1.
Dose–response relationship for intensity of alcohol use. All above estimates used the reference category of “light drinking” that included all individuals who did not fulfil criteria for hazardous alcohol use and also reported a daily drinking average during the last week of ≤2 drinks for women or ≤3 drinks for men. “Moderate drinking” included individuals who did not fulfil criteria for hazardous alcohol use and also reported a daily drinking average during the last week of >2 drinks for women of >3 drinks for men. “Heavy drinking” included individuals who did fulfil criteria for hazardous alcohol use and also reported a daily drinking average during the last week <8 for women or <10 for men. “Very heavy drinking” included individuals who reported hazardous alcohol use and also reported a daily drinking average during the last week ≥8 for women OR ≥10 for men. Explanatory variables of interest included: age, gender, ethnicity, homelessness, daily cocaine use, daily crack cocaine use, daily heroin use, daily crystal methamphetamine use, syringe sharing, incarceration, non-fatal overdose, same sex activity in men, unprotected sex, engagement in sex work, and STIs. Variables significant at the p < .10 threshold in bivariable analyses for each exposure group were included in the fixed multivariable models.
DISCUSSION
Among our cohort of street-involved youth who use illicit drugs, hazardous alcohol use was reported by over half of the sample. After intensive covariate adjustment, unprotected sex and homelessness were positively associated with hazardous alcohol use, while older age, and multiple markers of high-intensity illicit drug use, specifically daily use of heroin, crack cocaine and crystal methamphetamine were all negatively associated with hazardous alcohol use. In sub-analysis, associations for unprotected sex, homelessness, and daily heroin use were found to largely follow a dose–response pattern suggesting a dose–response relationship between intensity of alcohol use and these key variables of interest.
Causal links have been established for hazardous alcohol use and HIV transmission via risky sexual behaviour in the general population (Sheeran, Abraham, & Orbell, 1999; Sheeran & Orbell, 1998). Increased sexual risk behaviours have also been documented in youth who drink (Cooper, 2002; Parker, Harford, & Rosenstock, 1994), as well as populations who use injection drugs (Arasteh, DesJarlais, & Perlis, 2008; Cheng, Kerr, et al., 2016). In one study involving people who inject drugs, a dose–response relationship was observed between alcohol consumption and subsequent HIV infection (Howe, Cole, Ostrow, & Mehta Kirk, 2011). Though causality cannot be inferred from our study, we hypothesize that the acute intoxicating effects of alcohol alter cognitive reasoning and increase sexual arousal, negatively impacting the ability to negotiate safe sex and consistently use condoms (Ehrenstein et al., 2004; MacDonald, MacDonald, Zanna, & Fong, 2000).
We found negative associations between hazardous alcohol use and high-intensity illicit substance use, including daily heroin, crack cocaine, and crystal methamphetamine use. The negative association observed here between hazardous alcohol use and drug use behaviours, including daily substance use, to our knowledge has not previously been reported for street-involved youth. In fact, one study of adult people who inject drugs found an association between “at- risk” alcohol use and increased drug-related risk, including syringe sharing (Stein et al., 2000). The negative association of hazardous alcohol use with drug- related risk behaviour, taken together with finding a positive association with unprotected sex, suggests that hazardous alcohol use may be working primarily through risky sexual behaviour to increase HIV infection risk among street youth (Marshall et al., 2008; Roy et al., 2003).
Hazardous alcohol use was independently associated with homelessness in our study. Several studies have found that rent subsidy and housing assistance programmes are associated with reductions in HIV risk behaviours and improved clinical outcomes for HIV- infected adults (Aidala, Lee, Abramson, Messeri, & Siegler, 2007; Dasinger & Speiglman, 2007). In addition, residential stability was associated with decreased daily alcohol consumption in a cohort of street-involved youth in Montreal (Roy et al., 2011). Addressing homelessness is therefore one intervention that may impact youths’ ability to negotiate sexual risk and reduce alcohol use, independent of individual risk characteristics (Marshall, 2008).
Given the association between hazardous alcohol use and markers of increased risk for morbidity and mortality, assessment of alcohol use and integration of alcohol-specific interventions into addiction treatment and HIV prevention programmes for street-involved youth are warranted. Specifically, our study findings highlight the importance of having healthcare providers working with street-involved youth routinely performing the Alcohol Use Disorders Identification Test or other well-validated standard screening techniques to ascertain which individuals would benefit from addiction treatment interventions (Clark & Moss, 2010; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). The use of screening and brief intervention for hazardous alcohol use in youth is endorsed by the NIAAA (2004/2005). Anti-craving medications, in particular naltrexone which has demonstrated efficacy in reducing problematic alcohol use in youth (Miranda et al., 2014), are currently underutilized and should be scaled up.
Our study has several limitations. First, because street youth are a “hidden” population, our methods employed snowball sampling and street-based outreach, which do not produce a truly random sample. Second, because survey questions often touched on behaviours that youth may not have felt comfortable discussing, socially desirable reporting among our sample is possible. Third, as this was an observational cohort, though we hypothesized hazardous alcohol use was an outcome of increased sexual risk behaviour, further research is needed to determine causality. Fourth, because we relied on self-report of diagnosed STIs for our study, we may have underestimated the true prevalence of infection that resulted in a non-significant association with hazardous alcohol use (Medlow, Klineberg, & Steinbeck, 2014). Fifth, in the dose–response analysis, the “moderate drinking” group was relatively small, which may have led to non-significant findings between the “moderate drinking” and “light drinking” groups.
Our findings indicate that hazardous alcohol use is associated with unsafe sexual, but not drug-related, risk behaviours. Screening and intervention for hazardous alcohol use and associated sexual risk behaviours should be central to HIV prevention efforts among street- involved youth.
Acknowledgments
Funding
The study was supported by the US National Institutes of Health (U01DA038886). KD is supported by a MSFHR/St. Paul’s Hospital-Providence Health Care Career Scholar Award and a Canadian Institutes of Health Research New Investigator Award. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine, which supports EW.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
REFERENCES
- Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS and Behavior. 2007;11(Suppl. 6):101–115. doi: 10.1007/s10461-007-9276-x. [DOI] [PubMed] [Google Scholar]
- Arasteh K, DesJarlais DC, Perlis TE. Alcohol and HIV sexual risk behaviors among injection drug users. Drug & Alcohol Dependence. 2008;95(1–2):54–61. doi: 10.1016/j.drugalcdep.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baan R, Straif K, Grosse Y, Secretan B, ElGhissassi F, Bouvard V, Cogliano V. Carcinogenicity of alcoholic beverages. Lancet Oncology. 2007;8(4):292–293. doi: 10.1016/s1470-2045(07)70099-2. [DOI] [PubMed] [Google Scholar]
- Boivin JF, Roy E, Haley N, Galbaud du Fort G. The health of street youth: A Canadian perspective. Canadian Journal of Public Health. 2005;96(6):432–437. doi: 10.1007/BF03405183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng T, Johnston C, Kerr T, Nguyen P, Wood E, DeBeck K. Substance use patterns and unprotected sex among street-involved youth in a Canadian setting: A prospective cohort study. BMC Public Health. 2016;16:4. doi: 10.1186/s12889-015-2627-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng T, Kerr T, Small W, Nguyen P, Wood E, DeBeck K. High prevalence of risky income generation among street-involved youth in a Canadian setting. International Journal of Drug Policy. 2016;28:91–97. doi: 10.1016/j.drugpo.2015.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ. Focus on: The burden of alcohol use – trauma and emergency outcomes. Alcohol Research. 2013;35(2):150–154. [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Moss HB. Providing alcohol-related screening and brief interventions to adolescents through health care systems: Obstacles and solutions. PLoS Medicine. 2010;7(3):e1000214. doi: 10.1371/journal.pmed.1000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol, Supplement. 2002;14:101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cui J. QIC program and model selection in GEE analyses. Stata Journal. 2007;7:209–220. [Google Scholar]
- Dasinger LK, Speiglman R. Homelessness prevention: The effect of a shallow rent subsidy program on housing outcomes among people with HIV or AIDS. AIDS and Behavior. 2007;11(Suppl. 6):128–139. doi: 10.1007/s10461-007-9250-7. [DOI] [PubMed] [Google Scholar]
- DeMatteo D, Major C, Block B, Coates R, Fearon M, Goldberg E, Read SE. Toronto street youth and HIV/AIDS: Prevalence, demographics, and risks. Journal of Adolescent Health. 1999;25(5):358–366. doi: 10.1016/s1054-139x(99)00059-2. [DOI] [PubMed] [Google Scholar]
- Ehrenstein V, Horton NJ, Samet JH. Inconsistent condom use among HIV-infected patients with alcohol problems. Drug and Alcohol Dependence. 2004;73(2):159–166. doi: 10.1016/j.drugalcdep.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Farrow JA, Deisher RW, Brown R, Kulig JW, Kipke MD. Health and health needs of homeless and runaway youth. A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health. 1992;13(8):717–726. doi: 10.1016/1054-139x(92)90070-r. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, Mathers CD. Global burden of disease in young people aged 10–24 years: A systematic analysis. The Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Hasin DS. Epidemiology of DSM-5 alcohol use disorder: Results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halcon LL, Lifson AR. Prevalence and predictors of sexual risks among homeless youth. Journal of Youth and Adolescence. 2004;33:71–80. [Google Scholar]
- Health Canada, Office of Research and Surveillance, Controlled Substances and Tobacco Directorate. Canadian Alcohol and Drug Use Monitoring Survey for 2012. 2015 Retrieved from http://www.hc-sc.gc.ca/hc-ps/drugs- drogues/stat/_2012/summary-sommaire-eng.php. [Google Scholar]
- Howe CJ, Cole SR, Ostrow DG, Mehta Kirk GD. A prospective study of alcohol consumption and HIV acquisition among injection drug users. AIDS. 2011;25(2):221–228. doi: 10.1097/QAD.0b013e328340fee2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston CL, Callon C, Li K, Wood E, Kerr T. Offer of financial incentives for unprotected sex in the context of sex work. Drug & Alcohol Review. 2010;29(2):144–149. doi: 10.1111/j.1465-3362.2009.00091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith E, Kerr T, Zhang R, Montaner J, Wood E. High prevalence of syringe sharing among street involved youth. Addiction Research & Theory. 2008;16(4):353–358. [Google Scholar]
- MacDonald TK, MacDonald G, Zanna MP, Fong GT. Alcohol, sexual arousal, and intentions to use condoms in young men: Applying alcohol myopia theory to risky sexual behavior. Health Psychology. 2000;19(3):290–298. [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Donenberg GR, Ouellet LJ. Prevalence of psychiatric disorders among young injection drug users. Drug and Alcohol Dependence. 2012;124(1–2):70–78. doi: 10.1016/j.drugalcdep.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BD. The contextual determinants of sexually transmissible infections among street-involved youth in North America. Culture, Health & Sexuality. 2008;10(8):787–799. doi: 10.1080/13691050802295719. [DOI] [PubMed] [Google Scholar]
- Marshall BD, Kerr T, Livingstone C, Li K, Montaner JS, Wood E. High prevalence of HIV infection among homeless and street-involved Aboriginal youth in a Canadian setting. Harm Reduction Journal. 2008;5(1):35. doi: 10.1186/1477-7517-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medlow S, Klineberg E, Steinbeck K. The health diagnoses of homeless adolescents: A systematic review of the literature. Journal of Adolescence. 2014;37(5):531–542. doi: 10.1016/j.adolescence.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Milburn NG, Rotheram-Borus MJ, Rice E, Mallet S, Rosenthal D. Cross-national variations in behavioral profiles among homeless youth. American Journal of Community Psychology. 2006;37(1–2):63–76. doi: 10.1007/s10464-005-9005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Ray L, Blanchard A, Reynolds EK, Monti PM, Chun T, Ramirez J. Effects of naltrexone on adolescent alcohol cue reactivity and sensitivity: An initial randomized trial. Addiction Biology. 2014;19(5):941–954. doi: 10.1111/adb.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. Screening and brief intervention part 1: An overview. Alcohol Research & Health. 2004/2005;28(1) [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. Bethesda, MD: US Government Printing Office; 2007. Helping patients who drink too much: A clinician’s guide; pp. 1–34. [Google Scholar]
- Parker DA, Harford TC, Rosenstock IM. Alcohol, other drugs, and sexual risk-taking among young adults. Journal of Substance Abuse. 1994;6(1):87–93. doi: 10.1016/s0899-3289(94)90117-1. [DOI] [PubMed] [Google Scholar]
- Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug & Alcohol Review. 2010;29(4):437–445. doi: 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- Roy E, Haley N, Leclerc P, Cedras L, Weber AE, Claessens C, Boivin JF. HIV incidence among street youth in Montreal, Canada. AIDS. 2003;17(7):1071–1075. doi: 10.1097/00002030-200305020-00017. [DOI] [PubMed] [Google Scholar]
- Roy E, Haley N, Leclerc P, Sochanski B, Boudreau JF, Boivin JF. Mortality in a cohort of street youth in Montreal. Journal of the American Medical Association. 2004;292(5):569–574. doi: 10.1001/jama.292.5.569. [DOI] [PubMed] [Google Scholar]
- Roy E, Robert M, Vaillancourt E, Boivin JF, Vandermeerschen J, Martin I. Residential trajectory and HIV high-risk behaviors among Montreal street youth – a reciprocal relationship. Journal of Urban Health. 2011;88(4):767–778. doi: 10.1007/s11524-011-9574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychological Bulletin. 1999;125(1):90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- Sheeran P, Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. British Journal of Social Psychology. 1998;37(Pt 2):231–250. doi: 10.1111/j.2044-8309.1998.tb01167.x. [DOI] [PubMed] [Google Scholar]
- Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, Ezzati M. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: A pooled analysis. PLoS One. 2013;8(7):e65174. doi: 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Hanna L, Natarajan R, Clarke J, Marisi M, Sobota M, Rich J. Alcohol use patterns predict high-risk HIV behaviors among active injection drug users. Journal of Substance Abuse Treatment. 2000;18(4):359–363. doi: 10.1016/s0740-5472(99)00070-7. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Author; 2014. Results from the 2013 National Survey on Drug Use and Health: Summary of national findings. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. [PubMed] [Google Scholar]
- Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, Rehm J. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug & Alcohol Dependence. 2010;110(1– 2):108–116. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Ryan GW, Golinelli D, Ewing B, Wenzel SL, Kennedy DP, Zhou A. Substance use and other risk factors for unprotected sex: Results from an event-based study of homeless youth. AIDS and Behavior. 2012;16(6):1699–1707. doi: 10.1007/s10461-011-0017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler K, Melander L. The effect of drug and sexual risk behaviours with social network and non-network members on homeless youths’ sexually transmissible infections and HIV testing. Sexual Health. 2010;7(4):434–440. doi: 10.1071/SH09113. [DOI] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: The ARYS study. Harm Reduction Journal. 2006;3:18. doi: 10.1186/1477-7517-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]