Highlights
-
•
Although short-term efficacy and safety of Bisphosphonates (BPs) agents are well established, their long-term adverse effects still remain to be elucidated.
-
•
Long-term BP therapy inhibited bone turnover in the majority of patients, as confirmed by bone biopsy analysis.
-
•
Common clinical characteristics of atypical femoral fractures secondary to long-term BP include pain lasting for a couple of months, absence of injury history and bilateral femoral fractures in selected cases.
Keywords: Atypical femoral fracture, Bisphosohonate, Femoral shaft fracture, Adverse effects, Stress reaction
Abstract
Background
Bisphosphonates (BPs) are one of the most commonly used agents in the treatment of post-menopausal osteoporosis and other metabolic bone diseases.
Methods
Between 2010 and 2015, data of 22 osteoporotic women with femoral fractures due to low-energy trauma who received BPs previously were analysed.
Results
The mean duration of BP therapy was 7.6 years. The mean duration of union was 7.4 months. Five patients had non-union. Stress reaction was observed in the contralateral femur in 11 patients.
Conclusion
Radiographic studies should be performed on a regular basis to prevent atypical femoral fractures in patients on long-term BP therapy.
1. Introduction
Bisphosphonates (BPs) are one of the most commonly used agents in the treatment of post-menopausal osteoporosis and other metabolic bone diseases.1, 2, 3 These agents are potent inhibitors of bone resorption and exert their effects by reducing the osteoclast activity and increasing apoptosis.1, 2, 3 To date, several comparative studies have shown that BPs are effective, safe and welltolerated.1, 3, 4
Although short-term efficacy and safety of these agents are wellestablished, there are some concerns regarding their long-term adverse effects.5, 6, 7, 8, 9, 10, 11 It has been suggested that long-term BP therapy eventually impairs the ability of bone to remodel, leading to the accumulation of micro-damage and diminution of bone strength.7, 12
Several studies on long-term BP therapy-induced spontaneous femoral fractures have been published in the recent years.5, 9, 11, 13, 14, 15 In 2005, after the initial report on this subject by Odvina,8several authors established the relationship between long-term alendronate treatment and atypical femoral fractures and suggested an over-suppression of bone restoration in the underlying pathogenesis.5, 9, 13, 14, 15 Some authors advocated that over-suppressionhalted the osteoclastic activity, a process for the daily repair of micro-traumas, and led to stress fractures.5, 16As aforementioned, the common characteristic is the presence of prodromal pain before the fracture formation in the thigh region without an injury with a subtrochanteric/diaphyseal transverse or short oblique complete or incomplete non-comminuted fracture line with focal lateral cortical thickening and beaking of the cortex on one side, as evidenced by the imaging studies.5, 6, 17, 18, 19, 20
In this study, we aimed to evaluate the clinical and radiological outcomes of atypical femoral shaft fractures secondary to long-term BP therapy in post-menopausal osteoporotic women.
2. Materials and methods
Between March 2010 and June 2015, data of 22 osteoporotic women (mean age: 73 years; range, 51–85 years) with femoral fractures due to low-energy trauma (14 right, 12 left and four bilateral) who received BPs previously were retrospectively analysed. Patients with femoral fractures due to high-energy trauma and those with metabolic bone disease or renal failure (serum creatinine level <150 μmol/L) were excluded.
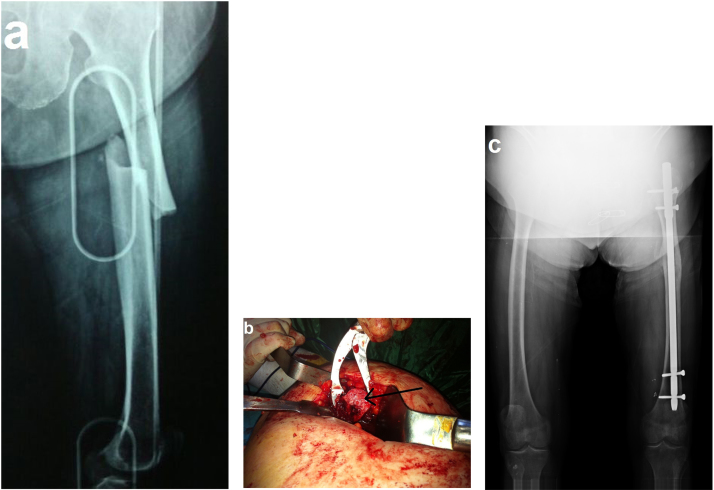
All patients had common characteristics of atypical femoral fractures secondary to BP therapy, as described previously as atypical complete or incomplete femoral fractures by any radiographic evidence of a transverse or short oblique fracture line, medial spike and focal lateral cortical thickening (Fig. 1).5, 6, 11, 15, 19, 20
Fig. 1.
(a) Radiographic image of an atypical fracture pattern of the left femoral shaft (lateral cortical thickening, transverse fracture line and medial cortical spike) in an 86-year-old female with a 10-year history of alendronate therapy; (b) An intraoperative image of thickened lateral cortex and narrowed femoral medulla (arrow); (c) Radiographic image of the fracture treated with intra-medullary nailing at 2 years.
Bone mineral density (BMD) values were calculated within the first week postoperatively from healthy hip images obtained by dual-energy X-ray absorptiometry (DXA; QDR 4500 DXA System; Hologic, Bedford, USA). Femoral fractures were evaluated using imaging studies.
Stress reactions and fracture healing were assessed by an independent observer. Radiographic healing was defined as callus bridging of three of four cortices on anteroposterior and lateral radiographs,21 as well as painless weight bearing on the affected extremity.
The femoral shaft fractures were treated with antegrade, locked and reamed intra-medullary (IM) nailing through the piriformis fossa in all patients. Open reduction was performed in 21 femurs, while IM nailing was performed with close reduction in five femurs. The study was approved by our Institutional Review Board, and all patients provided informed consent.
3. Results
The mean age of the subjects was 73 years (range, 51–85 years). The mean duration of BP therapy was 7.6 years (range, 4–15 years). The BPs used varied, including ibandronate in eight patients and alendronate in 14 patients. All patients suffered from pain radiating to the anterior thigh and groin during walking, in particular, and relieving with the use of non-steroidal anti-inflammatory drugs 7 days to 8 months before the fracture formation. The mean (±SD) lumbar spine T-score was 3.0 ± 1.0. The mean femoral neck BMD T-score was 2.7 ± 0.9. The mean length of hospital stay was 4.5 days (range, 3–10 days).
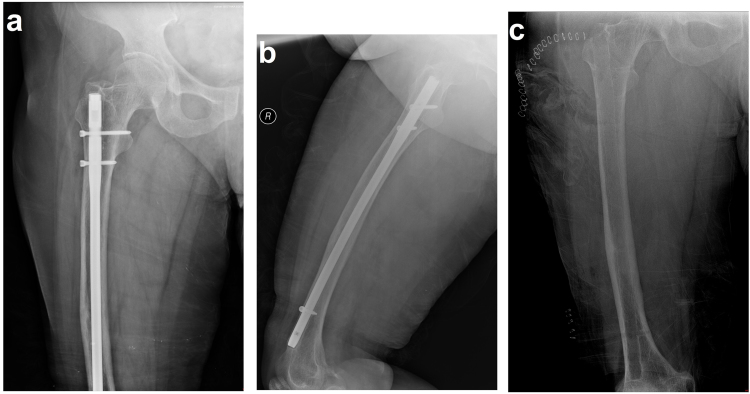
Stress reactions of all femurs were assessed. Eleven patients (50%) with localised cortical thickening of the femoral shaft or lateral subtrochanter with lateral bowing and incomplete transverse or oblique atypical femoral fracture were recommended prophylactic IM nailing; however, only one patient with prodromal pain underwent the procedure (Fig. 2, Fig. 3). Four of the remaining patients (18.1%) with contralateral femoral shaft fractures underwent IM nailing 18.2 months (range, 14–26 months) after the first fracture formation.
Fig. 2.
(a) An anteroposteriorradiographic image of a 67-year-old female with a 9-year history of alendronate therapy with prodromal pain showing the incomplete transverse fracture line in the right femoral shaft and focal lateral cortical thickening. (b) Coronal and (c) sagittal computed tomography scans showing lateral cortical thickening in the femoral shaft and a fracture line perpendicular to the cortex with sclerotic alterations and heterogeneity of the medulla. (d) A coronal T1-weighted magnetic resonance image showing low-signal heterogeneous intensity alterations. (e) Anteroposteriorand (f) lateral radiographic images after prophylactic intra-medullary nailing.
Fig. 3.
(a) Anteroposteriorand (b) lateral radiographic images of the aforementioned case at 3 years. (c) A radiographic image of the femur after implant removal due to pain on the surface of the anterior cortex, distal to the femur.
The mean duration of union was 7.4 months (range, 4–12 months). Five patients had non-union. One of them underwent a thicker reamed IM nailing with autografting, and union was achieved 8 months later. Two patients refused a repeat surgery. The remaining two patients underwent hemiarthroplasty for femoral head fracture on the same side, removing the IM nails 1 year after the femoral shaft fracture. Non-union femoral shaft fractures were treated with grafting and plate osteosynthesis. Union was achieved 16 months later in these patients.
Calcium, phosphate and creatinine levels were normal in all patients. However, alkaline phosphatase levels slightly increased in four patients, and parathyroid hormone levels slightly increased in three patients. In addition, six patients had vitamin D deficiency.
4. Discussion
Although the exact epidemiology and pathogenesis of atypical femoral fractures secondary to long-term BP therapy remain unclear, a possible imbalance between femoral bone resorption and bone formation has been suggested as an underlying mechanism.5, 7, 10, 12, 13 Over-suppression of the cortical bone turnover, which has already low remodelling, has been proposed to impair the removal function of the micro-damages.5, 9, 10, 13, 14 Several studies have demonstrated over-suppression of bone resorption in bone biopsy specimens collected from patients with femoral fractures who were using BP therapy.5, 11, 20
In an experimental animal model study, the mechanical strength of bones with normal bone density was shown to be reduced after receiving alendronate therapy.22Another study reported that long-term BP therapyinhibited bone turnover in the majority of patients, as confirmed by bone biopsy analysis.23
Although BPshave been shown to be effective in preventing osteoporotic fractures,3, 24 the incidence of stress fracture formation was found to be 1:1000 among patients receiving BP therapy for at least 42 months, while the incidence was 46-fold lower in those not receiving BP therapy.25Nonetheless, it was concluded that the incidence of stress fractures was acceptable in patients treated with BP therapy, as it is effective in preventing osteoporotic fractures.11, 15, 24, 26
On the other hand, there are several studies showing no clear association between atypical femoral fractures and BP therapy.27, 28 In a study including 14,195 women, Black et al.28 reported that subtrochanteric/diaphyseal femoral fractures were extremely rare in women using BP therapy for 10 years, suggesting that BP therapy does not substantially increase the risk of fracture formation.
Common clinical characteristics of atypical femoral fractures secondary to long-term BP include pain lasting for a couple of months, absence of injury history and bilateral femoral fractures in selected cases.5, 6, 11, 15, 17, 18, 19 In addition, imaging studies can demonstrate simple transverse or short oblique non-comminuted fractures with complete or incomplete detachment in the cortical hypertrophy region along with unicortical beaking.5, 6, 11, 15, 17, 18, 19
Long-term BP therapy may lead to stress reactions in the lateral femoral cortex before the fracture formation.6, 11 It may also induce cortical stress reactions in the contralateral femur.6, 11, 29 The incidence of bilateral atypical femoral fractures secondary to BP therapy has been reported to be 38% in the literature.12 In our study, we found this ratio to be 18%. In another series of 17 patients with alendronate-associated femoral insufficiency fractures, six patients had a radiological evidence of stress reaction affecting the contralateral femur, whereas three of them subsequently sustained fractures.29
Furthermore, nearly 56–76% of patients with alendronate-associated femoral insufficiency fractures had prodromal pain in the lower extremity weeks or months before the fracture formation.6, 29 In patients with pain and stress reactions, prophylactic IM nailing can be performed to prevent fracture formation, while conservative treatment is suggested in asymptomatic patients.6, 19 In our study, all patients suffered from prodromal pain before the fracture formation. In addition, six patients (54.5%) with contralateral femoral stress reaction had prodromal pain. In four of these, femoral shaft fractures developed later.
Moreover, IM nailing is effective in the treatment of BP therapy-related femoral fractures.15, 26 Of note, the healing process may prolong to 8 months, which is typically 3–6 months.26 In agreement with the literature data, the mean duration of union was 7.4 months in our study.
Despite successful union rates with IM nailing in the previous reports, we found union at a rate of 80% in our study. This can be attributed to the late healing process of femoral fractures secondary to BP therapy. Therefore, specific medical and surgical treatment strategies have been suggested for the treatment of BP therapy-related femoral fractures, rather than the approaches used in the treatment of conventional femoral fractures.15 Chiang et al.30 reported that teriparatide was effective in reducing pain in atypical fractures, contributing to the healing process with increased bone remodelling. They also suggested that teriparatide could prevent the formation of contralateral femoral fractures.
In conclusion, BP therapy, which is effective in preventing osteoporotic fractures, may induce atypical femoral fractures in the long term. Considering the fact that femoral fractures may increase the mortality and morbidity in elderly with increased complication rates, radio graphic studies should be performed on a regular basis to prevent atypical femoral fractures in patients on long-term BP therapy. In addition, pre-evaluation of stress reactions and increasing the awareness of patients on thigh pain would be preventive.
Conflicts of interest
The authors have none to declare.
References
- 1.Black D.M., Cummings S.R., Karpf D.B. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:15351541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 2.Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev. 1998;19:80–100. doi: 10.1210/edrv.19.1.0325. [DOI] [PubMed] [Google Scholar]
- 3.Ensrud K.E., Barrett-Connor E.L., Schwartz A. Randomized trial of effect of alendronate continuation versus discontinuation in women with low BMD: results from the Fracture Intervention Trial long-term extension. J Bone Miner Res. 2004;19:1259–1269. doi: 10.1359/JBMR.040326. [DOI] [PubMed] [Google Scholar]
- 4.Girgis C.M., Seibel M.J. Guilt by association? Examining the role of bisphosphonate therapy in the development of atypical femur fractures. Bone. 2011;48:963–965. doi: 10.1016/j.bone.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Somford M.P., Draijer F.W., Thomassen B.J., Chavassieux P.M., Boivin G., Papapoulos S.E. Bilateral fractures of the femur diaphysis in a patient with rheumatoid arthritis on long-term treatment with alendronate: cluesto the mechanism of increased bone fragility. J Bone Miner Res. 2009;24:1736–1740. doi: 10.1359/jbmr.090408. [DOI] [PubMed] [Google Scholar]
- 6.Wang K., Moaveni A., Dowrick A., Liew S. Alendronate-associated femoral insufficiency fractures and femoral stress reactions. J Orthop Surg. 2011;19:89–92. doi: 10.1177/230949901101900121. [DOI] [PubMed] [Google Scholar]
- 7.Ott S.M. Long-term safety of bisphosphonates. J Clin Endocrinol Metab. 2005;90:1897–1899. doi: 10.1210/jc.2005-0057. [DOI] [PubMed] [Google Scholar]
- 8.Odvina C.V., Zerwekh J.E., Rao D.S., Maalouf N., Gottschalk F.A., Pak C.Y. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90:1294–1301. doi: 10.1210/jc.2004-0952. [DOI] [PubMed] [Google Scholar]
- 9.Yoon R.S., Hwang J.S., Beebe K.S. Long-term bisphosphonate usage and subtrochanteric insufficiency fractures. J Bone Joint Surg Br. 2011;93:1289–1295. doi: 10.1302/0301-620X.93B10.26924. [DOI] [PubMed] [Google Scholar]
- 10.Hollick R., Reid D. Role of bisphosphonates in the management of postmenopausal osteoporosis: an update on recent safety anxieties. Menopause Int. 2011;17:66–72. doi: 10.1258/mi.2011.011014. [DOI] [PubMed] [Google Scholar]
- 11.Nieves J.W., Cosman F. Atypical subtrochanteric and femoral shaft fractures and possible association with bisphosphonates. Curr Osteoporos Rep. 2010;8:34–39. doi: 10.1007/s11914-010-0007-2. [DOI] [PubMed] [Google Scholar]
- 12.Giusti A., Hamdy N.A., Papapoulos S.E. Atypical fractures of the femur and bisphosphonate therapy: a systematic review of case/case series studies. Bone. 2010;47:169–180. doi: 10.1016/j.bone.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Capeci C.M., Tejwani N.C. Bilateral low-energy simultaneous or sequential femoral fractures in patients on long-term alendronate therapy. J Bone Joint Surg Am. 2009;91:2556–2561. doi: 10.2106/JBJS.H.01774. [DOI] [PubMed] [Google Scholar]
- 14.Lenart B.A., Neviaser A.S., Lyman S. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporos Int. 2009;20:1353–1362. doi: 10.1007/s00198-008-0805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weil Y.A., Rivkin G., Safran O., Liebergall M., Foldes A.J. The out come of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011;71:186–190. doi: 10.1097/TA.0b013e31821957e3. [DOI] [PubMed] [Google Scholar]
- 16.Li J., Mashiba T., Burr D.B. Bisphos phonate treatment suppresses not only stochnasticre modeling but also the target edrepair of micro damage. Calcif Tissue Int. 2001;69:281–286. doi: 10.1007/s002230010036. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg Z.S., La RoccaVieira R., Chan S.S. Bisphosphonate-related complete a typical subtrochanteric femoral fractures: diagnosticutility of radiography. AJR Am J Roentgenol. 2011;197:954–960. doi: 10.2214/AJR.10.6262. [DOI] [PubMed] [Google Scholar]
- 18.Shane E., Burr D., Abrahamsen B. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29:1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 19.Egol K.A., Park J.H., Prensky C., Rosenberg Z.S., Peck V., Tejwani N.C. Surgical treatment improves clinical and functional outcomes for patients who sustain incomplete bisphosphonate related femur fractures. J Orthop Trauma. 2013;27:331–335. doi: 10.1097/BOT.0b013e31827240ae. [DOI] [PubMed] [Google Scholar]
- 20.Chan S.S., Rosenberg Z.S., Chan K., Capeci C. Subtrochanteric femoral fractures in patients receiving long-term alendronate therapy: imaging features. AJR Am J Roentgenol. 2010;194:1581–1586. doi: 10.2214/AJR.09.3588. [DOI] [PubMed] [Google Scholar]
- 21.Whelan D.B., Bhandari M., McKee M.D. Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation. J Bone Joint Surg Br. 2002;84:15–18. doi: 10.1302/0301-620x.84b1.11347. [DOI] [PubMed] [Google Scholar]
- 22.Allen M.R., Burr D.B. Changes in vertebral strength-density and energy absorption-density relationships following bisphosphonate treatment in beagle dogs. Osteoporos Int. 2008;19:95–99. doi: 10.1007/s00198-007-0451-8. [DOI] [PubMed] [Google Scholar]
- 23.Armamento-Villareal R., Napoli N., Diemer K. Bone turnover in bone biopsies of patients with low-energy cortical fractures receiving bisphosphonates: a case series. Calcif Tissue Int. 2009;85:37–44. doi: 10.1007/s00223-009-9263-5. [DOI] [PubMed] [Google Scholar]
- 24.Black D.M., Cummings S.R., Karpf D.B. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 25.Schilcher J., Aspenberg P. Incidence of stress fractures of the femoral shaft in women treated with bisphosphonate. Acta Orthop. 2009;80:413–415. doi: 10.3109/17453670903139914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egol K.A., Park J.H., Rosenberg Z.S., Peck V., Tejwani N.C. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res. 2014;472:2728–2734. doi: 10.1007/s11999-013-2963-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abrahamsen B., Eiken P., Eastell R. Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res. 2009;24:1095–1102. doi: 10.1359/jbmr.081247. [DOI] [PubMed] [Google Scholar]
- 28.Black D.M., Kelly M.P., Genant H.K. Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med. 2010;362:1761–1771. doi: 10.1056/NEJMoa1001086. [DOI] [PubMed] [Google Scholar]
- 29.Kwek E.B., Goh S.K., Koh J.S., Png M.A., Howe T.S. An emerging pattern of subtrochanteric stress fractures: a long-term complication of alendronate therapy? Injury. 2008;39:224–231. doi: 10.1016/j.injury.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 30.Chiang C.Y., Zebaze R.M., Ghasem-Zadeh A., Iuliano-Burns S., Hardidge A., Seeman E. Teriparatide improves bone quality and healing of atypical femoral fractures associated with bisphosphonate therapy. Bone. 2013;52:360–365. doi: 10.1016/j.bone.2012.10.006. [DOI] [PubMed] [Google Scholar]