Abstract
Active human dendritic cells (DCs), which efficiently induce immune responses through their functions as antigen-presenting cells, exhibit direct anti-tumour killing activity in response to some pathogens and cytokines. These antigen-presenting and tumour killing abilities may provide a breakthrough in cancer immunotherapy. However, the mechanisms underlying this killer DC activity have not been fully proven, despite the establishment of interferon-α (IFN-α)-generated killer DCs (IFN-DCs). Here mature IFN-DCs (mIFN-DCs), generated from IFN-DCs primed with OK-432 (streptococcal preparation), exhibited elevated expression of CD86 and human leukocyte antigen-DR (minimum criteria for DC vaccine clinical trials) as well as antigen-presenting abilities comparable with those of mature IL-4-DCs (mIL-4-DCs). Interestingly, the killing activity of mIFN-DCs, which correlated with the expression of CD56 (natural killer cell marker) and was activated via the tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) and Fas ligand pathway, was stronger than that of IFN-DCs and remarkably stronger than that of mIL-4-DCs. Therefore, mIFN-DCs exhibit great potential as an anti-cancer vaccine that would promote both acquired immunity and direct tumour killing.
Significant advances have been made in the surgical and radiotherapeutic techniques and chemotherapeutic agents (e.g. immune checkpoint inhibitors) that comprise the field of cancer therapeutics1,2,3,4,5,6. However, the treatment of advanced cancers, which are characterized by organ involvement and distant metastasis, remains extremely difficult. Accordingly, oncological researchers have sought immunologic therapies, such as anti-tumour vaccination.
Thus far, antigen-presenting cell (APC)-based vaccination with active dendritic cells (DCs) has been evaluated as a method of efficient immunity against cancer antigens7. In this process, autologous monocyte-derived mature DCs are conventionally manufactured using granulocyte-macrophage colony-stimulating factor (GM-CSF) and interleukin-4 (IL-4) and are principally targeted against a specific cancer antigen8,9,10. However, human DC-based vaccine technology will require a breakthrough to achieve effective cancer treatment. We note that a population of cytotoxic DCs can directly kill tumour cells, in addition to inducing tumour antigen-specific cytotoxic T lymphocytes (CTLs); these ‘killer DCs’, therefore, appear to exhibit strong potential in the field of cancer immunotherapy.
DCs are generally divided into two major subtypes, myeloid DCs and plasmacytoid DCs (pDCs); however, in mice, interferon-producing killer DCs (IKDCs) have been described as a third subtype11,12. These latter cells produce substantial amounts of type I interferon (IFN) and IL-12 or IFN-γ, depending on the activating stimuli and can kill typical targets of natural killer (NK) cells via NK-activating receptors in response to stimulation with CpG11. In particular, B220+ NK1.1+ DCs have been reported to secrete large amounts of IFN-α and to promote the tumour necrosis factor-related apoptosis-inducing ligand (TRAIL)-dependent lysis of tumour cells12. In addition to IKDCs in mice, several subsets of killer DCs that exhibit anti-tumour cytotoxicity have been reported in humans13. These human killer DCs can be generated from monocytes in vitro in response to some pathogens and cytokines14; for example, immature IL-4-DCs (imIL-4-DCs) generated using GM-CSF and IL-4 exhibit killing activity following stimulation with bacterial lipopolysaccharide (LPS)15, CD40 ligand16 or OK-432, a streptococcal preparation17.
In Japan, clinical-grade OK-432 has been used as anti-tumour agent for more than 20 years, and its safety is well established18,19,20,21,22,23. Mechanistically, OK-432 promotes the functional maturation of imIL-4-DC through ligation of TLR424 and TLR925, and this maturation correlates with the upregulated expression of CD80, CD83 and CD8617,26,27, thus promoting the effective induction of antigen-specific T cells26. Combined treatment of mature IL-4 DCs (mIL-4-DCs) with OK-432 and prostaglandin E2 (PGE2) upregulates the expression of CD197 (CCR7), which is associated with migration to lymph nodes27. Katy et al., reported that following OK-432 activation, human mIL-4-DCs could specifically kill tumour cells via a novel CD40/CD40 ligand-mediated mechanism, without affecting normal cells17. OK-432 also induces the production of IL-12 from matured DCs without increasing the production of immuno-suppressive cytokines such as IL-1017.
Similarly, GM-CSF and IFN-α-generated DCs (IFN-DCs) also exhibit killing activity28,29. These cells express higher mRNA levels of NK cell markers, such as TRAIL, granzymes and killer cell lectin-like receptors (KLRs)28, and kill tumour cells via soluble TRAIL29, a factor that targets various tumours but does not affect normal cells30,31,32. According to previous reports, IFN-DCs exhibit a semi-mature phenotype, and full maturation can be achieved using CD40 ligand, LPS or polyribocytidylic acid (poly I-C)33,34. However, the effects of OK-432 on the maturation or killing activity of IFN-DCs have not previously been evaluated.
In the present study, we investigated the role of OK-432 in this setting and found that this agent not only induced the maturation, but also facilitated the killing activity of IFN-DCs. The mature IFN-DCs (mIFN-DCs) derived from OK-432-primed immature IFN-DCs exhibited similarly strong antigen-presenting abilities as mIL-4-DCs. Further study indicated that the killing activity of mIFN-DCs was stronger than that of IFN-DCs and remarkably superior to that of mIL-4-DCs. These characterizations suggest the strong clinical potential of a mIFN-DC-based vaccine for clinical use, as such an agent would be expected to induce acquired immunity and direct tumour killing.
Results
OK-432 induces a mature IFN-DC phenotype
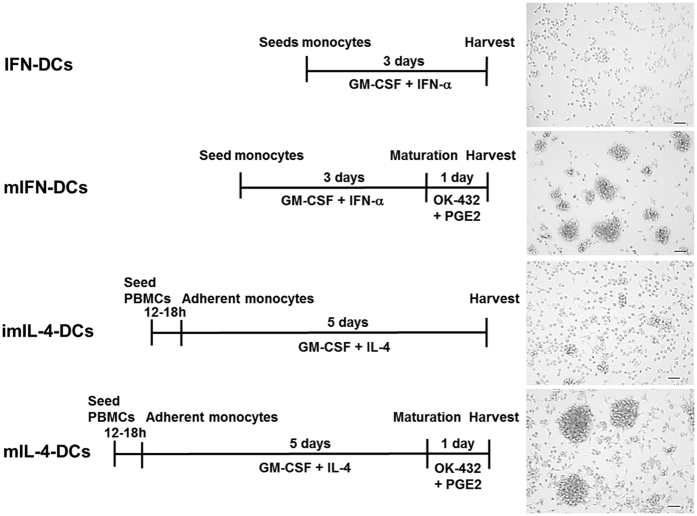
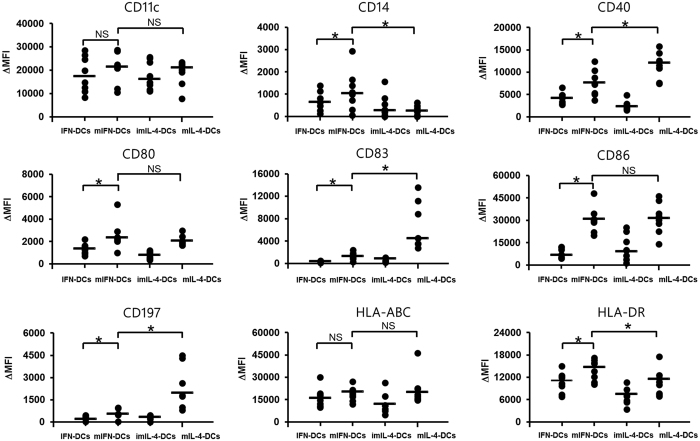
We first examined the phenotypic effects of OK-432 on mIFN-DCs and mIL-4-DCs. After OK-432 stimulation, similar remarkable clusters of cells bearing the morphologic features of mature DCs were observed equally among mIFN-DCs and mIL-4-DCs (Fig. 1). A phenotypic assessment of surface markers revealed the increased expression of costimulatory molecules such as CD80 and CD86 on mIFN-DCs, whereas the levels of these markers on mIL-4-DCs had not significantly changed (Fig. 2). Similarly, increases in the levels of CD14 and human leukocyte antigen (HLA)-DR were more evident on mIFN-DCs than on mIL-4-DCs. In contrast, mIL-4-DCs featured more strongly elevated expression of CD40, CD83 and CD197.
Figure 1. Dendritic cell (DC) preparation.
IFN-DCs were generated from monocytes that were purified from PBMCs using CD14 microbeads and subjected to a 3-day non-adherent culture in the presence of GM-CSF and IFN-α. For maturation, IFN-DCs were incubated with OK-432 and PGE2 for an additional 24 h. Alternatively, imIL-4-DCs and mIL-4-DCs were prepared using a conventional adhesion protocol. Adherent monocytes were cultured with GM-CSF and IL-4 for 5 days to generate imIL-4-DCs. Subsequently, imIL-4-DCs were stimulated with OK-432 and PGE2 to yield mIL-4-DCs. During each DC preparation process, cellular morphology was observed via microscopy prior to harvesting. Black bar = 50 μm.
Figure 2. Phenotypic comparison of dendritic cells (DCs) stimulated with OK-432.
DCs generated from patients (N = 8) were stained with mAbs for typical DC markers and analysed via flow cytometry. The change in mean fluorescence intensity (MFI) was calculated by subtracting the MFI values of the isotype control from the sample values. *p < 0.05; NS, not significant.
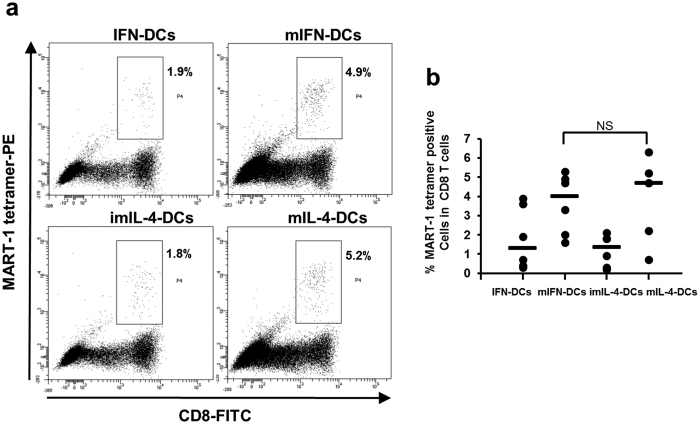
Comparison of the functions of mIFN-DCs and mIL-4-DCs
DCs and MART-1 peptides were used to induce CTLs in an in vitro system and thus confirm the antigen presentation abilities of our DC populations. As shown in Fig. 3a, the frequency of MART-1 specific CTLs among total CD8+ T cells was 2.4-fold higher following mIFN-DC induction, compared to IFN-DC induction (mIFN-DCs vs. IFN-DCs = 4.9% vs. 1.9%). In contrast, the percentages of CTLs induced by mIFN-DCs and mIL-4-DCs did not differ significantly (Fig. 3b).
Figure 3. The antigen presentation ability of mIFN-DCs is similar to that of mIL-4-DCs.
(a) Representative dot plots of data are shown. The percentages of MART-1 tetramer positive cells among CD3- and CD8-gated T cells are shown in each panel. (b) Summary of MART-1 CTL induction by DCs (N = 6).
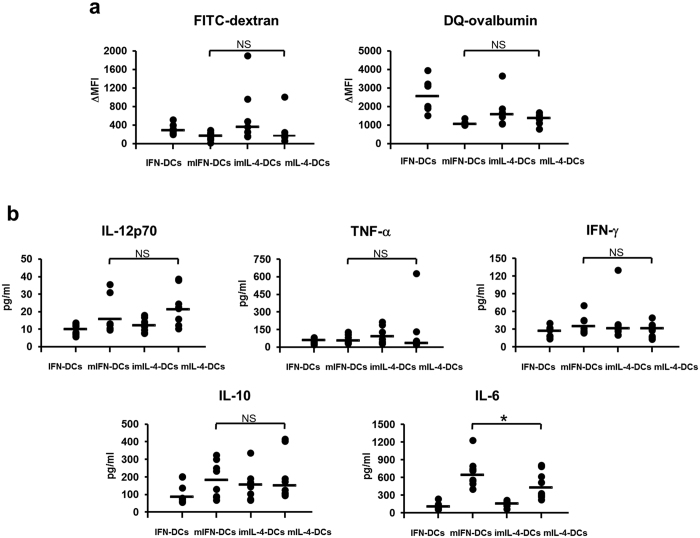
FITC-dextran uptake by DCs was determined to assess pinocytotic activity. The change in mean fluorescence intensity (MFI) of FITC-dextran was slightly lower in mIFN-DCs than in IFN-DCs, similar to mIL-4-DCs (Fig. 4a, left). Next, DQ-ovalbumin, a self-quenched albumin that fluoresces upon proteolytic degradation, was used to demonstrate an obvious reduction in the phagocytotic activity of mIFN-DCs upon OK-432 stimulation; this was also observed in mIL-4-DCs (Fig. 4a, right).
Figure 4. The functional analyses of DCs stimulated with OK-432.
(a) DCs were incubated with FITC-dextran to assess pinocytotic activity (N = 6) and with DQ-ovalbumin to examine phagocytotic activity (N = 6). For each experiment, the results are expressed as the change in mean fluorescence intensity (MFI) and calculated by subtracting the MFI at 4 °C from that at 37 °C. (b) DCs were seeded into 24-well plates at a density of 2 × 105 cells/ml for 24 h, and the supernatants were subjected to enzyme-linked immunosorbent assay (ELISA) analysis to determine the levels of IL-12p70, IFN-γ, TNF-α, IL-10 and IL-6. A summary of the cytokine production data is shown (N = 8).
Cytokine production was also investigated, using the supernatants of cells incubated in AIM-V medium for 24 h (Fig. 4b). In response to OK-432, mIFN-DCs and mIL-4-DCs produced similar amounts of IL-12p70, IFN-γ, TNF-α and IL-10. In contrast, mIFN-DCs produced significantly higher levels of IL-6, compared with mIL-4-DCs.
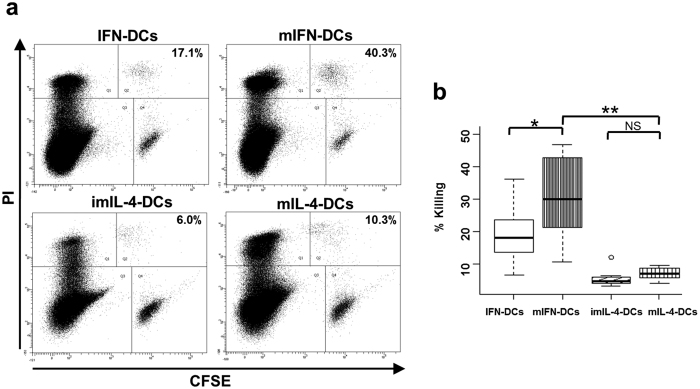
mIFN-DCs possess stronger cytotoxic activity than mIL-4-DCs
The killing activity of DCs against K562 cells was investigated using flow cytometry. In a representative experiment, IFN-DCs exhibited a killing activity of 17.1%, compared with 40.3% by mIFN-DCs (Fig. 5a), indicating a significant increase only in mIFN-DCs relative to IFN-DCs (Fig. 5b). Moreover, mIFN-DCs showed remarkably enhanced killing activity against K562 cells when compared with mIL-4-DCs. Unexpectedly, we did not observe a significant increase in tumour killing activity by mIL-4-DCs following priming with OK-432 (Fig. 5b). Accordingly, we next focused on the mechanisms underlying this enhanced tumour killing by mIFN-DCs.
Figure 5. The killing activity of mIFN-DCs is stronger than that of IFN-DCs and, particularly, mIL-4-DCs.
(a) CFSE-labelled K562 cells were incubated with indicated DCs at a ratio of 50:1 for 18 h. Incubated cells were subsequently subjected to flow cytometry and gated on a FSC and SSC dot plot to identify single cells. Subsequently, the gated cells were subgated according to CFSE and PI staining. DC killing activities are shown as percentages in the dot plot panels (representative of N = 11). (b) DC killing activity against K562 cells is indicated in the box plot (N = 11). *p < 0.05, **p < 0.01.
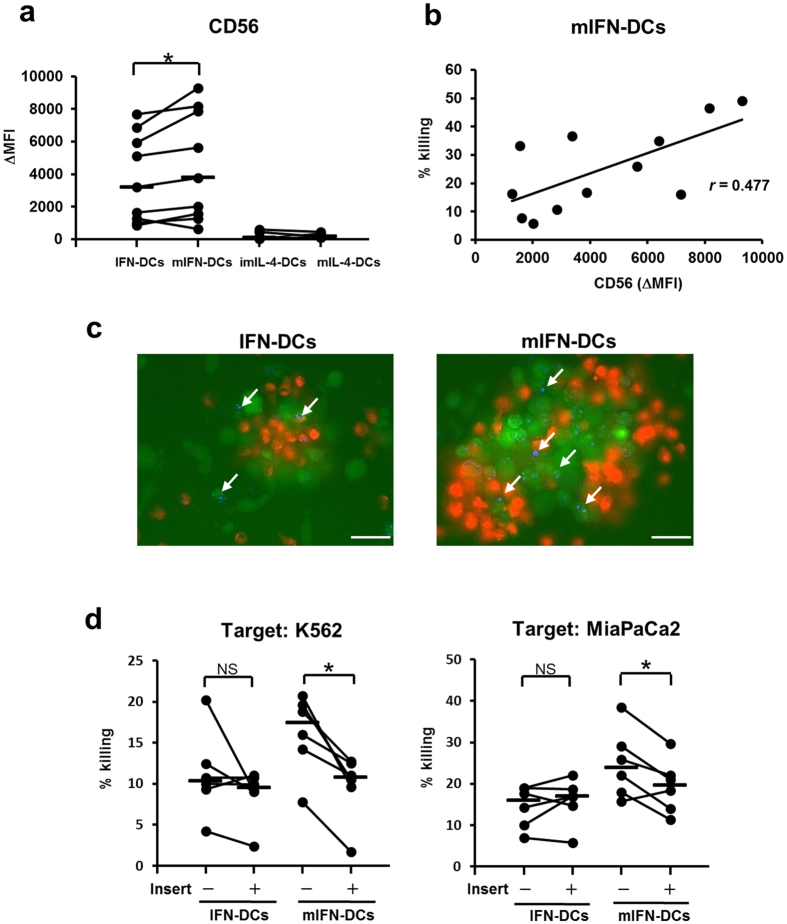
Tumour killing activity of mIFN-DCs correlates with the expression of CD56 and depends on soluble factor(s) and cell contact
Relative to the expression of IFN-DCs, CD56 was significantly increased on mIFN-DCs following OK-432 treatment (Fig. 6a), and a weak correlation was observed between the expression of CD56 and the killing activity of mIFN-DCs (r = 0.477; Fig. 6b). In contrast, the expression of CD56 on imIL-4-DCs and mIL-4-DCs was extremely low, consistent with the observed weak killing activity (Fig. 6a).
Figure 6. In mIFN-DCs, killing activity correlates with the expression of CD56 and is dependent on cell-to-cell contact.
(a) The expression of CD56 on DCs is shown in terms of the mean fluorescence intensity (MFI). The expression of CD56 on mIFN-DCs and IFN-DCs was compared (N = 12). (b) Correlation between the expression of CD56 and mIFN-DC killing activity (N = 12). (c) Observed tumour killing mediated by IFN-DCs or mIFN-DCs in vitro. CFSE (green)-labelled K562 cells were incubated with PKH 26 (red)-stained IFN-DCs or mIFN-DCs at a ratio of 1:1. After an 18-h incubation, the cells were stained with DAPI. White arrows indicate dead cells stained with DAPI. White bar = 50 μm. (d) IFN-DCs or mIFN-DCs were incubated with K562 or Mia PaCa2 cells at a ratio of 50:1 and in the presence or absence of an insert membrane for 18 h (N = 6).
Killing activity of mIFN-DCs against K562 cells was observed using fluorescence microscopy to confirm the cell contact dependency of tumour killing. IFN-DCs or mIFN-DCs were labelled with the red fluorescence dye PKH26, followed by incubation with K562 cells labelled with the green fluorescence dye CFSE. Remarkably, mIFN-DCs were found to form larger clusters with K562 cells, compared with IFN-DCs (Fig. 6c). Furthermore, large numbers of dead K562 cells (Fig. 6c: white arrows = DAPI staining) in clusters with mIFN-DCs, whereas only a few dead cells were observed in clusters with IFN-DCs. These results suggest that the formation of clusters between mIFN-DCs and target cells is important for tumour killing by mIFN-DCs. The involvement of cell contact was additionally investigated using transwell membrane assays. The killing activity of mIFN-DCs against K562 or MiaPaCa2 cells was reduced significantly in the presence of a transwell membrane insert, whereas no effect was observed for IFN-DCs (Fig. 6d). A cytotoxic assay in the presence of transwell inserts revealed that the killing activity of mIFN-DCs was reduced to a level similar to that of IFN-DCs (against K562 cells: median, IFN-DC = 9.5%, mIFN-DCs = 10.8%; against MiaPaCa2 cells: IFN-DCs = 17.0%, mIFN-DCs = 19.7%).
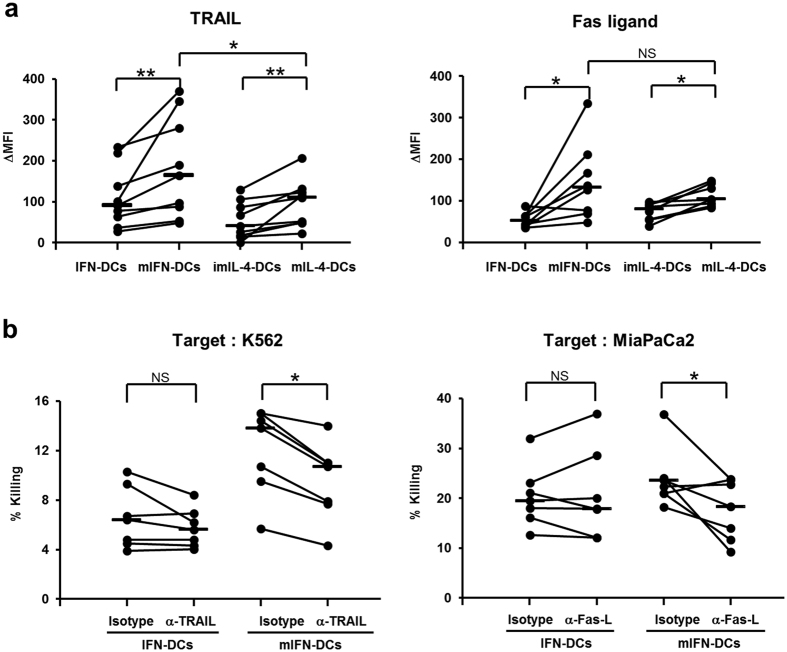
mIFN-DCs exert killing activity through the TRAIL and Fas ligand pathway
TNF family members (TNF-α, Fas ligand, TRAIL)35,36,37,38,39,40, perforin/granzyme B41, NO42,43 and peroxynitrites44 have been reported to be involved in the tumour killing mechanisms of killer DCs. The above results suggested that the increased killing activity of mIFN-DCs in response to OK-432 depended on a cell contact mechanism, leading to the speculation of involvement by cell surface-localized cytotoxic factors in mIFN-DC-mediated tumour killing. Notably, increased cell surface expression of TRAIL and Fas ligand was observed on both mIFN-DCs and mIL-4-DCs primed with OK-432 (Fig. 7a). In particular, the expression of TRAIL was significantly higher on mIFN-DCs than on mIL-4-DCs, whereas both cell populations exhibited similar increases in the expression of Fas ligand.
Figure 7. mIFN-DCs killing activity involves the TRAIL and Fas ligand pathway.
(a) Summary of cell surface expression of TRAIL and Fas ligand (N = 9, TRAIL; N = 8, Fas ligand). (b) Blockade of IFN-DC or mIFN-DC killing activity with mAbs against TRAIL or Fas ligand (Fas-L). IFN-DC or mIFN-DCs were pre-treated with the indicated mAbs for 2 h, followed by incubation with CFSE-labelled K562 or MiaPaCa2 cells for 18 h at a ratio of 50:1 (N = 7).
We subsequently examined whether the tumour killing activity of mIFN-DCs was dependent on TRAIL and Fas ligand. K562 (TRAIL sensitive)17 and MiaPaCa2 (Fas sensitive) cell lines45 were treated with antibodies specific for TRAIL or Fas ligand, respectively, to test the blocking of each ligand. TRAIL antibody blockade significantly suppressed the killing of K562 cells by mIFN-DCs (Fig. 7b, left panel), whereas this treatment had no significant effect on the killing of K562 cells by IFN-DCs. Similarly, Fas ligand antibody blockade reduced the killing of MiaPaCa2 cells by mIFN-DCs (Fig. 7b, right panel), whereas this treatment did not influence IFN-DCs-mediated killing. These results suggested that, in contrast to IFN-DCs, the killing activity of mIFN-DCs is mediated through the TRAIL and Fas ligand pathway.
Discussion
OK-432 has been well established as a clinical agent for DC maturation18,19,20,21,22,23. Accordingly, a 4-day non-adherent culture system in which IFN-DCs were primed with OK-432 was developed to generate mIFN-DCs. In contrast to mIL-4-DCs, the short-term generation of mIFN-DCs is also clinically beneficial because although mIFN-DCs express lower levels of CD40 and CD83, the increased expression levels of CD86 and HLA-DR, which were similar to those of mIL-4-DCs, met the minimum release criteria for DC vaccines46. Based on the pinocytotic and phagocytotic activity, cytokine production and antigen presenting profiles of mIFN-DCs were found to correlate with those of mature DCs, similar to mIL-4-DCs. Interestingly, OK-432 also facilitated an increase in the killing activity of IFN-DCs. However, the killing activity of mIFN-DCs, which correlated with the expression of CD56, was stronger than that of both IFN-DCs and mIL-4-DCs. OK-432 upregulated the expression of CD56 and cell surface TRAIL and Fas ligand on mIFN-DCs, and the independent involvement of TRAIL and Fas ligand in mIFN-DC-mediated tumour killing was proven via specific antibody blockade.
Although OK-432-activated human DCs kill tumour cells through CD40/CD40 ligand interactions17, other factors that may be involved in this cytotoxic process have not been fully examined. The association of CD56 with cell adhesion47,48 suggested that tumour killing by mIFN-DCs with expression of CD56 would depend on cell contact. We further speculated that cell surface cytotoxic molecules, such as tumour necrosis factor (TNF) family members, might participate in the required cell-to-cell interactions. Although OK-432 stimulation was previously found to upregulate the expression of Fas ligand on mononuclear cells49, our report is the first to demonstrate the increased expression of CD56, cell surface TRAIL and Fas ligand on mIFN-DCs following OK-432 stimulation. The observed clustering of mIFN-DCs and tumour cells might facilitate tumour killing via either cell surface TRAIL or Fas ligand. The reduced killing activity of mIFN-DCs in the presence of anti-TRAIL antibody suggests that these cells use mechanisms other than CD40/CD40 ligand signalling to exert their cytotoxic effects50. In contrast to previous reports, however, OK-432 did not promote a significant increase in tumour killing by mIL-4-DCs, possibly because of differences in the maturation cocktail used in combination with OK-432 and PGE2, as well as the incubation time17; both factors might have affected tumour killing by OK-432-induced DCs.
Clearly, OK-432-induced mIFN-DCs exhibited remarkably strong killing activity, which correlated with the expression of CD56 and depended on TRAIL and Fas ligand. Previously, CD56+ IFN-DCs exhibited stronger cytotoxicity against K562 cells, the majority of which are TRAIL positive, when compared with CD56− IFN-DCs29. However, in our study, we did not observe significant suppression of tumour killing by IFN-DCs in response to anti-TRAIL antibody treatment. The observed expression of granzyme B28 suggests that IFN-DCs might use multiple soluble factors to kill tumour cells. However, IFN-DCs are known to share phenotypic features with pDCs (e.g. CD11c and CD123)29, and pDC tumour-killing also correlates with the expression of TRAIL and CD56. Furthermore, the expression of TRAIL and TRAIL-dependent cytotoxicity are upregulated in pDCs in response to HIV infection51. pDCs activated by the tick-borne encephalitis vaccine FSME specifically upregulate the expression of CD56, which coincides with elevated levels of cytotoxic molecules such as TRAIL; furthermore FSME-activated pDCs specifically lyse NK target cell lines in a cell-cell contact dependent manner52. Accordingly, OK-432-induced mIFN-DCs might exhibit pDC-like responses.
It remains to be determined whether mIFN-DCs can kill tumour cells and induce CTLs in vivo. As mentioned above, mIFN-DCs express CD86 and HLA-DR46 and thus potentially possess antigen presentation ability comparable to that of mIL-4-DCs. However, the low level of expression of CD197 on mIFN-DCs might not be sufficient to promote migration to the lymph nodes and subsequent CTL induction. In addition to the ability to migrate to specific regions for direct tumour killing, the ability of antigen-pulsed mIFN-DCs to induce CTLs should be examined in tumour-bearing animal models. A report by Padovan et al., in which IFN-DCs produced IP10/CXCL10 and MIG/CXCL9 to attract activated CD8+ T cells and thus expand CTLs efficiently53, led to speculation that mIFN-DCs could potentially induce CTLs directly in the tumour regions, rather than in the lymph nodes. We further note that we observed higher levels of IL-6 in cultures of mIFN-DCs, compared with mIL-4-DCs (Fig. 4b). IL-6 mediates febrile and acute-phase responses by upregulating chemokines and cell adhesion molecules that support the growth of B cells and Th17 cells, but suppress regulatory T cells (T regs)54. Accordingly, the observed high production of IL-6 might provide mIFN-DCs with an advantage with respect to the induction of CTLs in tumour regions, which tend to harbour T regs55.
Clinically, mIFN-DCs may directly kill tumour cells that retain sensitivity to TRAIL and Fas ligand signalling. Unlike normal cells, various types of tumours are susceptible to TRAIL-induced apoptosis, and the Fas/Fas ligand-mediated killing activity of mIFN-DCs might be less advantageous for cancer treatment. Fas/Fas ligand interactions are known to induce apoptosis in hepatocytes56 and to have immunomodulatory effects on immune homeostasis and tolerance57. Although TRAIL- or Fas ligand-mediated apoptosis-resistant cancer cells have been reported, one option for cancer therapy would combine the anti-tumour effects of TRAIL and Fas ligand with standard chemotherapy58,59.
In conclusion, this study confirms that OK-432 induced the maturation of IFN-DCs with strong antigen-presenting abilities (comparable to mIL-4-DCs), and facilitated the TRAIL- and Fas ligand-mediated killing activity of these mIFN-DCs. Further clarification of the characteristics of mIFN-DCs is expected to contribute to the development of adaptive immunotherapies and the achievement of acquired anti-cancer immunity.
Methods
Subjects and Ethics Statement
DC vaccination therapy at the Shinshu University Hospital was approved by the Ethics Committee of Shinshu University School of Medicine (approval number 1123 and 1199). The Act on the Safety of Regenerative Medicine in Japan was enforced since November 25, 2014. Class III technologies use somatic cells with accumulated clinical experiences and are regarded as low risk technologies. The DC vaccination therapy (Class III technology) at the Shinshu University was approved on November 25, 2015 (approval number: PC3150643 and PC3150645). Human peripheral blood mononuclear cell (PBMC)-rich fraction was collected from blood samples of patients via leukapheresis with a COM.TEC cell separator (Fresenius Kabi Japan K.K., Tokyo, Japan). PBMCs were subsequently isolated using a Ficoll-Plaque Premium (GE Healthcare, Piscataway, NJ, USA) density gradient. The collection and use of blood complied with relevant guidelines and institutional practices from Ethics Committees of Shinshu University School of Medicine (approval number 2107). Written informed consent was obtained from all patients. All methods in this study were performed in accordance with the Ethical Guidelines for Medical and Health Research involving Human Subjects proposed by Ministry of Health, Labour and Welfare in Japan60.
DC generation
To generate IFN-DCs, monocytes were purified from PBMCs using CD14 microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany), which yielded a CD14+ monocyte purity of >95%. The monocytes were cultured in AIM-V medium (Gibco, Gaithersburg, MD, USA) containing GM-CSF (1,000 U/ml; Miltenyi Biotec) and PEGylated-IFN-α-2b (1 μg/ml of PEG-Intron; MSD, Tokyo, Japan) for 3 days in a HydroCell (Cell Seed, Tokyo, Japan).
For maturation, IFN-DCs were stimulated with OK-432 (10 μg/ml; Chugai Pharmaceutical Co, Ltd, Tokyo, Japan) and PGE2 (10 ng/ml; Daiichi Fine Chemical Co, Ltd, Toyama, Japan). After a 24-h incubation, mIFN-DCs were harvested for further analysis. Alternatively, imIL-4-DCs were generated using a previously reported adhesion protocol8,9,10. In brief, PBMCs were placed into 100-mm plastic tissue culture plates (BD Biosciences, San Jose, CA, USA) in AIM-V medium. After removing non-adherent cells, 50 ng/ml of GM-CSF (Gentaur, Brussels, Belgium) and 50 ng/ml of IL-4 (R&D Systems, Inc., Minneapolis, MN, USA) were added the following day, and the cells were cultured for 5 days to generate imDCs. ImIL-4-DCs were subsequently stimulated with 10 μg/ml of OK-432 and 50 ng/ml of PGE2 for 24 h to generate mIL-4-DCs.
Phenotyping of DCs
Fluorescein isothiocyanate (FITC)- or phycoerythrin (PE)-conjugated forms of monoclonal antibodies (mAbs) against the following DC markers were used: CD11c, CD80, CD86 and HLA-ABC (BD Pharmingen, San Diego, CA, USA); CD14, CD40, CD83 and HLA-DR (eBioscience, San Diego, CA, USA) and CD197 (R&D Systems, Minneapolis, MN, USA). To detect NK cell markers, DCs were incubated with allophycocyanin (APC)-conjugated anti-CD56 mAb (BD Pharmingen, San Diego, CA, USA). To evaluate cytotoxic cell surface molecules, PE-conjugated mAbs specific for anti-TRAIL (BD Pharmingen) and anti-Fas ligand (eBioscience) were used. All analyses were performed on a FACSCanto II flow cytometer (BD Biosciences).
CTL induction in vitro
PBMCs from HLA-A*02:01 patients were used to generate DCs, which were subsequently pulsed with 20 μg/ml of MART-1 26-35 A27L (ELAGIGILTV) peptide (MBL, Medical & Biological Laboratories Co., Ltd., Nagoya, Japan) at 37 °С for 1 h. After washing with AIM-V medium, DCs were treated with mitomycin C (25 μg/ml; Kyowa Hakko Kogyo Co, Ltd, Tokyo, Japan) at 37 °C for 1 h. After two washes, the prepared DCs were used as stimulator cells; non-adherent PBMCs collected after seeding into plastic tissue-culture plates were used as responder cells. Stimulator (1 × 106) and responder cells were co-cultured at a ratio of 1:10 in AIM-V medium supplemented with IL-2 (2.5 U/ml; Imunace, Shionogi, Pharmaceutical, Osaka, Japan), IL-7 (5 ng/ml; R&D Systems) and IL-15 (10 ng/ml; PeproTech, Rocky Hill, NJ, USA) for 3−5 days. AIM-V media supplemented with 10% foetal bovine serum (FBS; Thermo Fisher Scientific K.K., Yokohama, Japan) was added depending on cell expansion. After a 2–3-day incubation, cells were harvested and stained with FITC-conjugated anti-CD8 (Beckman Coulter, Inc., Brea, CA, USA) and APC-conjugated anti-CD3 (eBioscience) mAbs and T-select HLA-A*02:01 MART-1 tetramer-ELAGIGILTV-PE (MBL).
Pinocytotic and phagocytotic assay
To evaluate pinocytotic activity, DCs were incubated with 250 μg/ml FITC-dextran (Molecular Probes, Eugene OR, USA) in AIM-V medium supplemented with 10% FBS at 37 °С for 3 h and subsequently washed twice with FACS buffer. DCs were then incubated with 10 μg/ml DQ-ovalbumin (Molecular Probes, Eugene OR, USA) at 37 °C for 30 min to examine phagocytotic activity. After two washes, cells were analysed using flow cytometry.
Cytokine production
DCs were seeded at a density of 2 × 105 cells/ml into a 24-well plate. After a 24-h incubation in AIM-V medium, cytokines were measured in the collected supernatants using ELISA kits for IL-12p70, IFN-γ (R&D Systems), TNF-α, IL-6 and IL-10 (BD Biosciences) according to the manufacturers’ protocols.
Cytotoxicity assay
To examine the cytotoxic activity of DCs, we used a previously reported method28 with slight modifications. Initially, 1 × 106 K562 (ATCC, Manassas, VA, USA) or MiaPaCa2 cells (RIKEN BRC, Tsukuba, Japan) were labelled with carboxyfluorescein succinimidyl ester (CFSE; 5 μM; Molecular Probes) in PBS supplemented with 0.1% FBS at 37 °C for 10 min, followed by two washes with AIM-V medium. Different numbers of DCs were used as effectors and were incubated with 1 × 104 CFSE-labelled K562 or MiaPaCa2 cells (targets) in AIM-V medium containing 10% FBS at 37 °C for 18 h. To evaluate intrinsic controls, an aliquot of K562 or MiaPaCa2 cells equivalent to the number of effector cells was incubated with labelled target cells. The cells were then washed in FACS buffer, stained with propidium iodide (PI; 2 μg/ml; Sigma-Aldrich Co. LLC., Tokyo, Japan) for 5 min and analysed using flow cytometry. Tumour-specific killing activity was determined as follows: % killing = experimental % of PI+ CFSE-labelled cells − intrinsic % of PI+ CFSE-labelled cells. To assess contact-dependent killing, CFSE-labelled target cells and effector cells were separated using transwell inserts fitted with 0.4-μm pore polyester membranes (Corning Inc., Corning, NY, USA). For the blocking experiment, effector cells were pre-treated with 10 μg/ml anti-TRAIL or anti-Fas ligand mAbs (Biolegend, San Diego, CA, USA) at 37 °C for 2 h and were incubated with labelled target cells.
Fluorescence microscopy
IFN-DCs or mIFN-DCs were labelled with the red fluorescence dye PKH26 (2 μM; Sigma-Aldrich) according to the manufacturer’s instructions, and subsequently incubated with CFSE-labelled K562 cells at a ratio of 1:1. After an 18-h incubation, cells were stained with DAPI (1.5 μM; Molecular Probes) for 5 min to detect cell death and assessed under a fluorescence microscope.
Statistical analysis
The Wilcoxon signed-rank test with Bonferroni correction was used to compare differences among groups. Spearman’s rank-order correlation was used to calculate the correlation of the expression of CD56 with killing activity. All statistical analyses were performed using IBM SPSS Advanced Statistics software, version 23.0 (IBM Japan, Tokyo, Japan). Differences were considered statistically significant at a p value < 0.05.
Additional Information
How to cite this article: Koya, T. et al. Interferon-α-inducible Dendritic Cells Matured with OK-432 Exhibit TRAIL and Fas Ligand Pathway-mediated Killer Activity. Sci. Rep. 7, 42145; doi: 10.1038/srep42145 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
This work was supported by Grants-in-Aid for Scientific Research (KAKENHI; 24501330 to S. S.) and scientific research from The Japan Society for the Promotion of Science (JSPS; AS2621549N to S.S.). We thank Drs Koichi Hirabayashi and Takashi Kobayashi for providing medical care.
Footnotes
The authors declare no competing financial interests.
Author Contributions T.K., R.Y. and S.S. performed study design; T.K. manufactured dendritic cell vaccines; H.Y. and K.S. analyzed immune monitoring data; and T.K. and S.S. took special responsibility for this study and wrote the article. All authors reviewed the manuscript.
References
- Hodi F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363, 711–723 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topalian S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366, 2443–2454 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamid O. et al. Safety and tumour responses with lambrolizumab (anti-PD-1) in melanoma. N. Engl. J. Med. 369, 134–144 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahmer J. R. et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N. Engl. J. Med. 366, 2455–2465 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchok J. D. et al. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 369, 122–133 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber J. S. et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or-naive melanoma. J. Clin. Oncol. 31, 4311–4318 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R. M. Decisions about dendritic cells: past, present, and future. Annu. Rev. Immunol. 30, 1–22 (2012). [DOI] [PubMed] [Google Scholar]
- Koido S. et al. Treatment with chemotherapy and dendritic cells pulsed with multiple Wilms’ tumour 1 (WT1)-specific MHC class I/II-restricted epitopes for pancreatic cancer. Clin. Cancer. Res. 20, 4228–4239 (2014). [DOI] [PubMed] [Google Scholar]
- Saito S. et al. Safety and tolerability of allogeneic dendritic cell vaccination with induction of Wilms tumour 1-specific T cells in a paediatric donor and paediatric patient with relapsed leukaemia: a case report and review of the literature. Cytotherapy. 17, 330–335 (2015). [DOI] [PubMed] [Google Scholar]
- Sakai K. et al. Dendritic cell-based immunotherapy targeting Wilms’ Tumor 1 (WT1) in patients with relapsed malignant glioma. J. Neurosurg. 123, 989–997 (2015). [DOI] [PubMed] [Google Scholar]
- Chan C. W. et al. Interferon producing killer dendritic cells provide a link between innate and adaptive immunity. Nat. Med. 12, 207–213 (2006). [DOI] [PubMed] [Google Scholar]
- Taieb J. et al. A novel dendritic cell subset involved in tumour immunosurveillance. Nat. Med. 12, 214–219 (2006). [DOI] [PubMed] [Google Scholar]
- Larmonier N., Fraszczak J., Lakomy D., Bonnotte B. & Katsanis E. Killer dendritic cells and their potential for cancer immunotherapy. Cancer. Immunol. Immunother. 59, 1–11 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tel J. et al. Tumoricidal activity of human dendritic cells. Trend. Immunol. 35, 38–46 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakomy D. et al. Cytotoxic dendritic cells generated from cancer patients. J. Immunol. 187, 2775–2782 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu G. et al. Innate direct anticancer effector function of human immature dendritic cells, II: Role of TNF, lymphotoxin-a1b2, Fas ligand, and TNF related apoptosis-inducing ligand. J. Immunol. 168, 1831–1839 (2002). [DOI] [PubMed] [Google Scholar]
- Hill K. S. et al. OK432-activated human dendritic cells kill tumour cells via CD40/CD40 ligand interactions. J. Immunol. 181, 3108–3115 (2008). [DOI] [PubMed] [Google Scholar]
- Torisu M., Katano M., Kimura Y., Itoh H. & Takesue M. New approach to management of malignant ascites with a streptococcus preparation, OK-432. I. Improvement of host immunity and prolongation of survival. Surgery. 93, 357–364 (1983). [PubMed] [Google Scholar]
- Watanabe Y. & Iwa T. Clinical value of immunotherapy with the streptococcal preparation OK-432 in non-small cell lung cancer. J. Biol. Response. Mod. 6, 169–180 (1987). [PubMed] [Google Scholar]
- Kikkawa F. et al. Randomised study of immunotherapy with OK-432 in uterine cervical carcinoma. Eur. J. Cancer. 29A, 1542–1546 (1993). [DOI] [PubMed] [Google Scholar]
- Maehara Y. et al. Postoperative immunochemotherapy including streptococcal lysate OK-432 is effective for patients with gastric cancer and serosal invasion. Am. J. Surg. 168, 36–40 (1994). [DOI] [PubMed] [Google Scholar]
- Kitahara S. et al. Inhibition of head and neck metastatic and/or recurrent cancer by local administration of multi-cytokine inducer OK-432. J. Laryngol. Otol. 110, 449–453 (1996). [DOI] [PubMed] [Google Scholar]
- Sato M. et al. Effect of intradermal administration of streptococcal preparation OK-432 on interferon and natural killer cell activities in patients with oral cancer. Int. J. Oral. Surg. 13, 7–15 (1984). [DOI] [PubMed] [Google Scholar]
- Okamoto M. et al. Involvement of Toll-like receptor 4 signalling in interferon-γ production and antitumor effect by streptococcal agent OK-432. J. Natl. Cancer Inst. 95, 316–326 (2003). [DOI] [PubMed] [Google Scholar]
- Oshikawa T. et al. Antitumor effect of OK-432-derived DNA: one of the active constituents of OK-432, a streptococcal immunotherapeutic agent. J. Immunother. 29, 143–150 (2006). [DOI] [PubMed] [Google Scholar]
- Nakahara S., Tsunoda T., Baba T., Asabe S. & Tahara H. Dendritic cells stimulated with a bacterial product, OK-432, efficiently induce cytotoxic T lymphocytes specific to tumour rejection peptide. Cancer. Res. 63, 4112–4118 (2003). [PubMed] [Google Scholar]
- Sato M. et al. Generation of mature dendritic cells fully capable of T helper type 1 polarization using OK-432 combined with prostaglandin E2. Cancer. Sci. 94, 1091–1098 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korthals M. et al. Monocyte derived dendritic cells generated by IFN-alpha acquire mature dendritic and natural killer cell properties as shown by gene expression analysis. J. Transl. Med. 5, 46 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papewalis C. et al. IFN-alpha skews monocytes into CD56+ -expressing dendritic cells with potent functional activities in vitro and in vivo. J. Immunol. 180, 1462–1470 (2008). [DOI] [PubMed] [Google Scholar]
- Griffith T. S., Chin W. A., Jackson G. C., Lynch D. H. & Kubin M. Z. Intracellular regulation of TRAIL-induced apoptosis in human melanoma cells. J. Immunol. 161, 2833–2840 (1998). [PubMed] [Google Scholar]
- Walczak H. et al. Tumoricidal activity of tumour necrosis factor-related apoptosis-inducing ligand in vivo. Nat. Med. 5, 157–163 (1999). [DOI] [PubMed] [Google Scholar]
- Griffith T. S. et al. A. Monocyte-mediated tumoricidal activity via the tumour necrosis factor–related cytokine, TRAIL. J. Exp. Med. 189, 1343–1353 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohty M. et al. IFN-alpha skews monocyte differentiation into Toll-like receptor 7-expressing dendritic cells with potent functional activities. J. Immunol. 171, 3385–3393 (2003). [DOI] [PubMed] [Google Scholar]
- Tosi. D. et al. Role of cross-talk between IFN-alpha-induced monocyte-derived dendritic cells and NK cells in priming CD8+ Tcell responses against human tumour antigens. J. Immunol. 172, 5363–5370 (2004). [DOI] [PubMed] [Google Scholar]
- Chapoval A. I., Tamada K. & Chen L. In vitro growth inhibition of a broad spectrum of tumour cell lines by activated human dendritic cells. Blood. 95, 2346–2351 (2000). [PubMed] [Google Scholar]
- Lu G. et al. Innate direct anticancer effector function of human immature dendritic cells, II: Role of TNF, lymphotoxin-a1b2, Fas ligand, and TNF related apoptosis-inducing ligand. J. Immunol. 168, 1831–1839 (2002). [DOI] [PubMed] [Google Scholar]
- Raftery M. J. et al. Targeting the function of mature dendritic cells by human cytomegalovirus: a multilayered viral defence strategy. Immunity. 15, 997–1009 (2001). [DOI] [PubMed] [Google Scholar]
- Yang R., Xu D., Zhang A. & Gruber A. Immature dendritic cells kill ovarian carcinoma cells by a FAS/FASL pathway, enabling them to sensitize tumour-specific CTLs. Int. J. Cancer 94, 407–413 (2001). [DOI] [PubMed] [Google Scholar]
- Vidalain P. O. et al. Measles virus induces functional TRAIL production by human dendritic cells. J. Virol. 74, 556–559 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yu Y., Zhang M., Wang W. & Cao X. The involvement of TNF-α-related apoptosis-inducing ligand in the enhanced cytotoxicity of IFN-β-stimulated human dendritic cells to tumour cells. J. Immunol. 166, 5407–5415 (2001). [DOI] [PubMed] [Google Scholar]
- Kim S. K. et al. Enhanced anti-cancer activity of human dendritic cells sensitized with gamma-irradiation-induced apoptotic colon cancer cells. Cancer. Lett. 335, 278–288 (2013). [DOI] [PubMed] [Google Scholar]
- Huang J., Tatsumi T., Pizzoferrato E., Vujanovic N. & Storkus W. J. Nitric oxide sensitizes tumour cells to dendritic cell-mediated apoptosis, uptake, and cross-presentation. Cancer. Res. 65, 8461–8470 (2005). [DOI] [PubMed] [Google Scholar]
- Nicolas A. et al. Dendritic cells trigger tumour cell death by a nitric oxide dependent mechanism. J. Immunol. 179, 812–818 (2007). [DOI] [PubMed] [Google Scholar]
- Fraszczak J. et al. Peroxynitrite dependent killing of cancer cells and presentation of released tumour antigens by activated dendritic cells. J. Immunol. 184, 1876–1884 (2010). [DOI] [PubMed] [Google Scholar]
- Yuan K. et al. Calmodulin mediates Fas-induced FADD-independent survival signalling in pancreatic cancer cells via activation of Src-extracellular signal-regulated kinase (ERK). J. Biol. Chem. 286, 24776–24784 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterfield L. H. et al. Recommendations from the iSBTc-SITC/FDA/NCI workshop on immunotherapy biomarkers. Clin. Cancer Res. 17, 3064–3076 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamerman J., Ogasawara, A., K. & Lanier L. L. NK cells in innate immunity. Curr. Opin. Immunol. 17, 29–35 (2005). [DOI] [PubMed] [Google Scholar]
- Moretta A. Natural killer cells and dendritic cells: rendezvous in abused tissues. Nat. Rev. Immunol. 2, 957–964 (2002). [DOI] [PubMed] [Google Scholar]
- Toda K. et al. The cytocidal activity of OK-432-activated mononuclear cells against human glioma cells is partly mediated through the Fas ligand/Fas system. Jpn. J. Cancer. Res. 87, 972–976 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgopoulos N. T. et al. A novel mechanism of CD40-induced apoptosis of carcinoma cells involving TRAF3 and JNK/AP-1 activation. Cell. Death. Differ. 13, 1789–1801 (2006). [DOI] [PubMed] [Google Scholar]
- Hardy A. W., Graham D. R., Shearer G. M. & Herbeuval J.-P. HIV turns plasmacytoid dendritic cells (pDC) into TRAIL-expressing killer pDC and down-regulates HIV coreceptors by Toll-like receptor 7-induced IFN-alpha. Proc. Natl. Acad. Sci. USA. 104, 17453–17458 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tel J. et al. Human plasmacytoid dendritic cells are equipped with antigen-presenting and tumoricidal capacities. Blood. 120, 3936–3944 (2012). [DOI] [PubMed] [Google Scholar]
- Padovan E., Spagnoli G. C., Ferrantini M. & Heberer M. IFN-alpha2a induces IP-10/CXCL10 and MIG/CXCL9 production in monocyte-derived dendritic cells and enhances their capacity to attract and stimulate CD8+ effector T cells. J. Leukoc. Biol. 71, 669–676 (2002). [PubMed] [Google Scholar]
- Pasare C. & Medzhitov R. Toll pathway-dependent blockade of CD4+ CD25+ T cell-mediated suppression by dendritic cells. Science. 299, 1033–1036 (2003). [DOI] [PubMed] [Google Scholar]
- Woo E. Y. et al. Regulatory CD4(+)CD25(+) T cells in tumours from patients with early-stage non-small cell lung cancer and late-stage ovarian cancer. Cancer. Res. 61, 4766–4772 (2001). [PubMed] [Google Scholar]
- Lacronique V. et al. Bcl-2 protects from lethal hepatic apoptosis induced by an anti-Fas antibody in mice. Nat. Med. 2, 80–86 (1996). [DOI] [PubMed] [Google Scholar]
- Askenasy N., Yolcu E. S., Yaniv I. & Shirwan H. Induction of tolerance using Fas ligand: a double-edged immunomodulator. Blood. 105, 1396–1404 (2005). [DOI] [PubMed] [Google Scholar]
- Zhu H. et al. Overcoming acquired resistance to TRAIL by chemotherapeutic agents and calpain inhibitor I through distinct mechanisms. Mol. Ther. 9, 666–673 (2004). [DOI] [PubMed] [Google Scholar]
- Iwase M., Watanabe H. & Kondo G. Enhanced susceptibility of oral squamous cell carcinoma cell lines to FAS-mediated apoptosis by cisplatin and 5-fluorouracil. Int. J. Cancer. 106, 619–625 (2003). [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Labour and Welfare in Japan. Ethical Guidelines for Medical and Health Research Involving Human Subjects http://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000080278.pdf (2015).