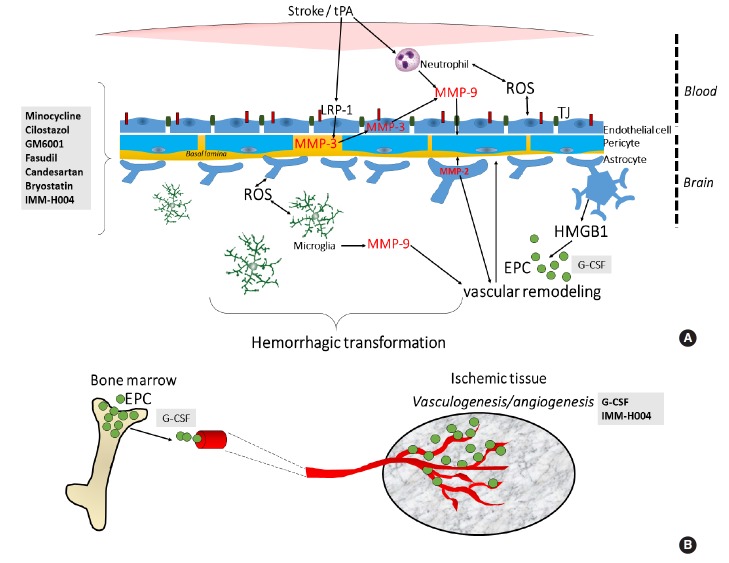
Figure 2.
Molecular targets of pharmacological agents tested to attenuate hemorrhagic transformation (HT) after delayed tPA treatment. (A) The HT that ensues after delayed tPA treatment has been ascribed to increased reperfusion and on tPA’s effect on metalloproteinase (MMP) activity and other signaling pathways including the lipoprotein receptor protein (LRP) signaling. In particular, tPA’s signaling actions in the neurovascular unit increases risk of blood-brain barrier (BBB) leakage, neurovascular cell death and HT. Minocycline, cilostazol, GM6001, fasudil, candesartan, bryostatin and IMM-H004 reduces the HT by preserving the BBB through their actions on various MMPs and tight junction (TJ) proteins. (B) Aside from restoring BBB integrity, enhancement of neovascularization or blood vessel formation may also counteract delayed tPA-induced HT. G-CSF and IMM-H004 may reduce the HT by enhancing neurovascularization. G-CSF’s therapeutic effects has been attributed to mobilization of EPCs which reconstitute the BBB. EPC, endothelial progenitor cell; G-CSF, granulocyte-colony stimulating factor; HMGB1, high-mobility-group-box-1; ROS, reactive oxygen species.