Abstract
Background
Ultrasound can be used to facilitate lumbar puncture, especially in obese patients.
Methods
In this study, midline and paramedian approaches with curved and linear transducers were compared in patients with Body Mass Index (BMI) above 25 kg/m2 for the identification of spinal landmarks. In each view, six major landmarks, including spinous process, ligamentum flavum, laminae, epidural space, subarachnoid space and posterior longitudinal ligament, were detected by emergency medicine residents and were then reviewed by radiologists.
Results
Sixty patients with a mean BMI of 29.18 enrolled in the study. This study showed that a curved transducer detected major landmarks more accurately compared to a linear transducer. There was also a poor kappa correlation between these transducers in the midline and paramedian approaches.
Conclusion
This study showed that ultrasound can detect lumbar landmarks in overweight and obese patients, with the paramedian approach and a curved transducer being superior to the midline approach and a linear transducer in detecting these landmarks.
Keywords: Ultrasound, lumbar puncture
Introduction
Lumbar puncture (LP) is widely used to obtain diagnostic samples of cerebrospinal fluid in the emergency department. This method is used to evaluate infections, neoplasms, inflammatory disorders and hemorrhage;1 moreover, LP can be used for therapeutic purposes, such as in benign intracranial hypertension and delivering therapeutic agents to the intrathecal space.2,3 In order to perform this procedure, the patient is placed in a lateral decubitus position. Tuffier’s line, which connects right and left iliac crests, is used to detect the L4–L5 interspinous space. This space or one space above is usually used for LP. This method is dependent on personal expertise and finding the required landmarks might be challenging in patients with obesity or anatomical variations.3 This might be time consuming. Repeated attempts in inserting the needle can also be painful for the patient, resulting in decreased satisfaction and an increase in traumatic LP.4 Traumatic LP also affects the results of the test, obscuring the detection of leukocytosis.5
Since ultrasound is a safe, cheap and widely available imaging method, ultrasound scanning has been used to facilitate this procedure. It can help the physician in finding the optimal puncture point and the depth and angle of needle insertion. Studies have been done to evaluate this method, especially in adult obese patients.3,6 There are few studies that have used the paramedian approach and a curved transducer for detecting spinal landmarks. In this study, patients with a BMI above 25 kg/m2 were evaluated by ultrasound using two different transducers and three different approaches in order to find an optimal method for detecting lumbar puncture landmarks.
Methods
This was a prospective, diagnostic test evaluation study. The study protocol was approved by the Clinical Ethics Board of Imam Khomeini Hospital and the affiliated medical school. The study was done in the emergency department of a referral hospital and trauma center during January–June 2015. Written informed consent was obtained from all patients after thorough explanation of the study. The inclusion criteria were: BMI above 25 kg/m2 and age above 18 years. During the study period, all patients with BMI above 25 kg/m2, who came to the emergency department for any reason, were included in the study. The exclusion criteria were pregnancy and previous lumbar surgery.
Three PGY3 emergency medicine residents were first trained in a 3-h workshop. The scientific content of the workshop was validated by a panel of radiologists and emergency medicine physicians. The workshop was divided into an hour of lectures followed by a 2-hour hands-on training session, in which residents practiced the skills needed for identifying LP anatomic landmarks, including spinous process, ligamentum flavum, laminae, epidural space, subarachnoid space and posterior longitudinal ligament on standardized patients. The ultrasound device utilized was a Sonosite Edge 2 (FUJIFILM SonoSite Inc., Bothwell, WA, USA), equipped with a linear transducer (7.5–10 MHz, Model: HFL38xi) and a curved one (2–5 MHz, Model: rC60xi).7 During the clinical shifts of the residents, lumbosacral ultrasound was done using both the linear and curved transducers with midline and left and right paramedian approaches on patients in the lateral decubitus position. The above-mentioned landmarks were named, scanned, recorded and printed by the emergency residents after each scan. Thus a total of six scans (midline, right and left paramedian with both linear and curved transducers) were recorded for each participant and submitted to the corresponding supervisor to assess the accuracy of identifying landmarks and the results were also recorded. Three radiologists were in the panel of supervisors. All radiologists were board certified with over 10 years experience and were part of the faculty of the affiliated medical school. The panel of radiologists did not perform any ultrasound scans and were only responsible for reviewing the scans from 20 patients each. The radiologists scored the images taken by the residents. If the residents had detected each landmark correctly, it was marked as correct by the supervisor. If they made a mistake in identifying a landmark or were not able to detect it, it was marked as incorrect or undetected, respectively. The numbers of correct, incorrect and undetected landmarks were recorded. To calculate inter-rater reliability, the first 20 scans were reviewed by all radiologists and the results were used to determine kappa correlation.
The sample size n required for the study was calculated using the following formula
where is the standard score of 1.96 for an α value of 0.05. p is the expected proportion of detected landmarks (q = 1-p) and was assigned a value of 0.97 following a study done by Ferre and Sweeney,6 and the margin of error d was estimated at 4.5%. The required sample size was calculated as 56.
All data were gathered on individual data sheets for each patient and were analyzed using SPSS version 16, (Chicago, SPSS Inc) using Chi square and kappa correlation.
Results
Sixty subjects were enrolled in this study. All participants were white Caucasians. There were 32 (53.3%) male and 28 (46.7%) female participants. The mean age ± SD was 40.13 ± 13.65 years. The mean BMI ± SD was 29.18 ± 2.64 Kg/m2. The minimum and maximum BMI were 25.1 and 36.8 kg/m2, respectively (Table 1). Twenty-four participants had a BMI above 30 and the rest had BMI values between 25 and 30.
Table 1.
Baseline characteristics of study participants
| Age (Years ± SD) | 40.13 ± 13.65 | Range: 13–65 |
|---|---|---|
| BMI (kg/m2 ± SD) | 29.18 ± 2.64 | Range: 25.1–36.8 |
| Gender | Female: 28 (46.7%) Male: 32 (53.3%) |
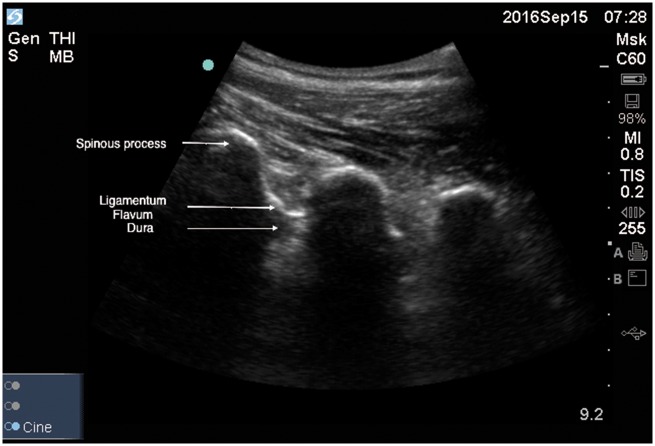
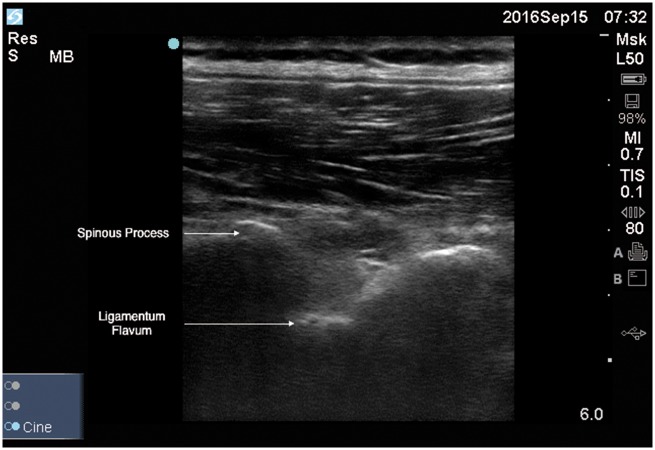
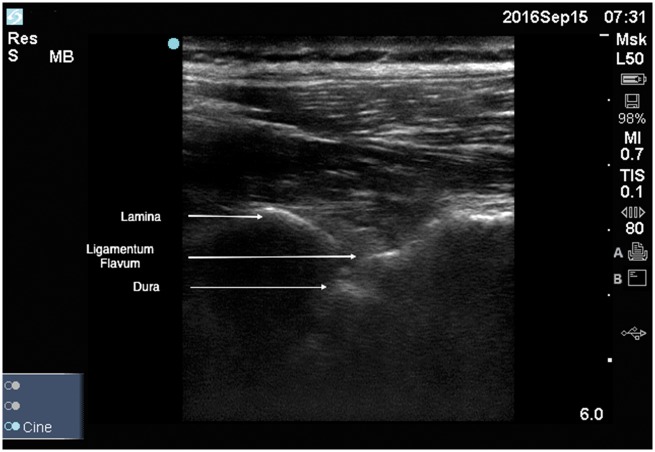
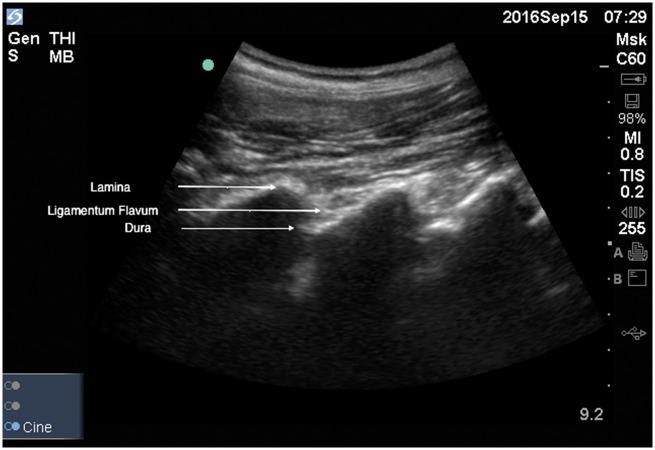
The inter-rater reliability between the three radiologists was substantial, kappa = 0.68, p < 0.0001. Figures 1 to 4 show the ultrasound scans performed on one of the patients using both transducers in the midline and paramedian approaches.
Figure 1.
Midline view with the curved transducer.
Figure 2.
Midline view with the linear transducer.
Figure 3.
Paramedian view with the linear transducer.
Figure 4.
Paramedian view with the curved transducer.
The results of the midline approach using linear and curved transducers are summarized in Table 2. The right and left paramedian results using linear and curved transducers are also summarized in Table 3. Table 4 provides the kappa correlation and p-values in each approach using both linear and curved transducers.
Table 2.
Midline vertebral approach in detecting LP landmarks using linear and curved transducers
| Landmark | Identification condition | Linear probe | Curved probe |
|---|---|---|---|
| Spinous process | Correct | 58 (96.7%) | 60 (100%) |
| Incorrect | 0 | 0 | |
| Not detected | 2 (3.3%) | 0 | |
| Ligamentum flavum | Correct | 20 (33.3%) | 36 (60%) |
| Incorrect | 7 (11.7%) | 15 (25%) | |
| Not detected | 33 (55%) | 9 (15%) | |
| Lamina | Correct | 8 (13.3%) | 32 (53.4%) |
| Incorrect | 43 (71.7%) | 24 (40%) | |
| Not detected | 9 (15%) | 4 (6.6%) | |
| Epidural space | Correct | 8 (13.3%) | 30 (50%) |
| Incorrect | 45 (75%) | 21 (35%) | |
| Not detected | 7 (11.7%) | 9 (15%) | |
| Subarachnoid space | Correct | 8 (13.3%) | 31 (51.6%) |
| Incorrect | 44 (73.4%) | 25 (41.7) | |
| Not detected | 8 (13.3%) | 4 (6.7%) | |
| Posterior longitudinal ligament | Correct | 15 (25%) | 47 (78.3%) |
| Incorrect | 0 | 0 | |
| Not detected | 45 (75%) | 13 (21.7%) |
Table 3.
Right and left paramedian approach in detecting LP landmarks using linear and curved transducers
| Landmark | Identification condition | Linear probe |
Curved probe |
||
|---|---|---|---|---|---|
| Right | Left | Right | Left | ||
| Spinous process | Correct | 56 (93.3%) | 54 (93.3%) | 60 (100%) | 60 (100%) |
| Incorrect | 1 (1.7%) | 4 (6.7%) | 0 | 0 | |
| Not detected | 3 (5%) | 0 | 0 | 0 | |
| Ligamentum flavum | Correct | 31 (51.7%) | 27 (45%) | 56 (93.3%) | 58 (96.7%) |
| Incorrect | 8 (13.3%) | 11 (18.3%) | 3 (5%) | 1 (1.7%) | |
| Not detected | 21 (35%) | 22 (36.7%) | 1 (1.7%) | 1 (1.7%) | |
| Lamina | Correct | 26(43.3%) | 21 (35%) | 56 (53.3%) | 54 (90%) |
| Incorrect | 13 (21.7%) | 17 (28.3%) | 4 (6.7%) | 5 (8.3%) | |
| Not detected | 21 (35%) | 22 (36.7%) | 0 | 1 (1.7%) | |
| Epidural space | Correct | 24(40%) | 18 (30%) | 56 (53.3%) | 54 (90%) |
| Incorrect | 8 (13.3%) | 10 (16.7%) | 3 (5%) | 4 (6.7% | |
| Not detected | 28 (46.7%) | 32 (53.3%) | 1 (1.7%) | 2 (3.3%) | |
| Subarachnoid space | Correct | 24(40%) | 20 (33.3%) | 56 (93.3%) | 54 (90%) |
| Incorrect | 15 (25%) | 18 (30%) | 4 (6.7%) | 5 (8.3%) | |
| Not detected | 21(35%) | 22 (36.7%) | 0 | 1 (1.7%) | |
| Posterior longitudinal ligament | Correct | 17 (28.3%) | 18 (30%) | 58 (96.7%) | 57 (95%) |
| Incorrect | 0 | 0 | 0 | 0 | |
| Not detected | 43 (71.7%) | 42 (70%) | 2 (3.3%) | 3 (5%) | |
Table 4.
Comparison between linear and curved transducers in midline, right and left paramedian approaches
| Approach | Landmark | Kappa correlation | p Value |
|---|---|---|---|
| Midline | Spinous process | N/A | N/A |
| Ligamentum flavum | 0.2 | 0.006 | |
| Lamina | 0.04 | 0.34 | |
| Epidural space | 0.04 | 0.47 | |
| Subarachnoid space | 0.07 | 0.12 | |
| Posterior longitudinal ligament | −0.01 | 0.047 | |
| Right paramedian | Spinous process | N/A | N/A |
| Ligamentum flavum | 0.043 | 0.37 | |
| Lamina | −0.017 | 0.716 | |
| Epidural space | 0.02 | 0.62 | |
| Subarachnoid space | N/A | N/A | |
| Posterior longitudinal ligament | −0.02 | 0.49 | |
| Left paramedian | Spinous process | N/A | N/A |
| Ligamentum flavum | 0.01 | 0.76 | |
| Lamina | −0.02 | 0.72 | |
| Epidural space | −0.02 | 0.72 | |
| Subarachnoid space | −0.02 | 0.64 | |
| Posterior longitudinal ligament | −0.005 | 0.9 |
The spinous process in the midline approach was the most detected landmark with linear and curved transducers, 96.7% and 100%, respectively. When considering the midline approach, there was poor kappa correlation between linear and curved transducers in all landmarks and a statistically significant difference for ligamentum flavum and posterior longitudinal ligament (p = 0.006, 0.047). Using the curved transducer improved landmark detection compared to the linear transducer. In the left and right paramedian approaches, there was also a poor kappa correlation in detecting different landmarks; however, there was not a statistically significant difference in detecting landmarks by linear and curved transducers. When considering the overall performance of both approaches, the paramedian approach was superior to the midline approach in landmark detection.
Finally, when comparing overweight with obese participants, there was not a significant difference in detecting landmarks except for ligamentum flavum and subarachnoid space (p = 0.04 and p = 0.03 respectively). These two landmarks were detected accurately more frequently in overweight participants compared to obese participants.
Discussion
This study was done on 60 patients with a mean BMI of 29.18 to compare the use of linear and curved transducers in detecting six spinal landmarks using ultrasound. In the hospital setting, both linear and curved transducers are available and physicians are able to use each transducer to get a better view. This study showed substantial inter-rater reliability between the panel of radiologists (kappa = 0.68). Then, there was poor correlation between the transducers in midline, left and right paramedian approaches and with better detection when using the curved transducer in a paramedian approach. This might be due to the characteristics of the curved transducer, which includes lower frequency and higher depth of penetration and better anatomical skin contact. The small sonographic window between spinous processes could also result in this difference.6
Nowadays, with an increased number of obese patients presenting to ED, the results of this study could be used to facilitate performing LP using ultrasound in this population, since age and gender have minimal impact on the anatomy of spine.
Studies have been done using ultrasound in detecting spinal landmarks and lumbar puncture sites. In a study done by Ferre et al.,6 76 patients, with a BMI of 31.4 ± 9.8, were included and five different landmarks (spinous processes or laminae, ligamentum flavum, dura mater, epidural space and subarachnoid space) were detected by linear and curved array transducers in the midline and paramedian approaches. When comparing both approaches, in the paramedian approach, both linear and curved transducers detected bone and soft tissue landmarks; however, the midline approach, due to a smaller window and the presence of spinous process, was less successful. It also showed that an increase in BMI makes palpating landmarks more difficult, but landmark detection by ultrasound is superior to palpation.6 Our study was able to detect landmarks less frequently compared to this study. This could be due to the limited experience of our residents compared to the ED physicians in that study. In a study published in 2006, ultrasound was able to detect L4–L5 spinous processes and spinal canal in 76% of patients who were obese and had difficult to palpate landmarks.8 Another study showed that the most important landmarks in order to perform lumbar puncture are spinous process and ligamentum flavum.9 Our study was able to detect spinous process in 100% patients using a curved transducer in midline and paramedian approaches and ligamentum flavum in 96.7% of patients using a curved transducer in the right paramedian approach.
Ultrasound has also been used in difficult epidural punctures. Grau and colleagues have shown that a paramedian approach is superior for viewing spinal anatomy.10 When considering the results of our study, the paramedian approach was also superior to the midline approach.
To our knowledge, this study was the first to detect posterior longitudinal ligament. This ligament was correctly detected in 78.3% of patients using a curved transducer compared to 25% with a linear transducer. The location of the posterior longitudinal ligament could provide a better understanding of the depth of the structures and help in performing LP.
Limitations
This study was done in the emergency department of a referral hospital and aimed to assess the optimal technique for new operators to detect anatomical landmarks prior to LP. Further studies could be done to assess the optimal technique and learning curve of participants in multicenter studies with an increased number of study participants. It is also recommended to conduct the study on obese patients who require LP to see if ultrasound could really increase LP success rate. Since ultrasound is an operator-dependent diagnostic tool, in order to limit individual variations, only three PGY3 residents were part of this study. Other studies covering an increased number of residents and comparing the results obtained by each individual could be conducted. Since ultrasound techniques require experience, it is suggested to evaluate the learning curve of each resident to see if their performance improved with practice. Finally, lumbar MRI is the gold standard for detecting lumbar landmarks. It is recommended to compare the results of ultrasound to MRI in future studies.
Conclusion
This study showed that ultrasound can be used in detecting lumbar landmarks in overweight and obese patients. The paramedian approach is superior to the midline approach and the curved transducer could detect more landmarks compared to the linear transducer.
Acknowledgement
The study team would like to express their deepest gratitude to all patients who participated in this study.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
The study was approved by the Clinical Ethics Board of Imam Khomeini Hospital and the affiliated medical school.
Guarantor
SBH
Contributors
SF and SBH researched literature and conceived the study. SS1, MA and SBH were involved in protocol development and gaining ethical approval. SS2 was responsible for patient recruitment. MA did data analysis. MA and SBH wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
References
- 1.Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA 2006; 296: 2012–2022. [DOI] [PubMed] [Google Scholar]
- 2.Shaikh F, Brzezinski J, Alexander S, et al. Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ 2013; 346: f1720–f1720. [DOI] [PubMed] [Google Scholar]
- 3.Mofidi M, Mohammadi M, Saidi H, et al. Ultrasound guided lumbar puncture in emergency department: time saving and less complications. J Res Med Sci 2013; 18: 303–307. [PMC free article] [PubMed] [Google Scholar]
- 4.Seeberger MD, Kaufmann M, Staender S, et al. Repeated dural punctures increase the incidence of postdural puncture headache. Anesth Analg 1996; 82: 302–305. [DOI] [PubMed] [Google Scholar]
- 5.Peterson MA, Pisupati D, Heyming TW, et al. Ultrasound for routine lumbar puncture. Acad Emerg Med 2014; 21: 130–136. [DOI] [PubMed] [Google Scholar]
- 6.Ferre RM, Sweeney TW. Emergency physicians can easily obtain ultrasound images of anatomical landmarks relevant to lumbar puncture. Am J Emerg Med 2007; 25: 291–296. [DOI] [PubMed] [Google Scholar]
- 7.Sonosite Edge II, http://www.sonosite.com/edge-2 (accessed 19 December 2016).
- 8.Stiffler KA, Jwayyed S, Wilber ST, et al. The use of ultrasound to identify pertinent landmarks for lumbar puncture. Am J Emerg Med 2007; 25: 331–334. [DOI] [PubMed] [Google Scholar]
- 9.Huang MY, Lin AP, Chang WH. Ultrasound-assisted localization for lumbar puncture in the ED. Am J Emerg Med 2008; 26: 955–957. [DOI] [PubMed] [Google Scholar]
- 10.Grau T, Liepold RW, Conradi R, et al. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand 2001; 45: 766–771. [DOI] [PubMed] [Google Scholar]