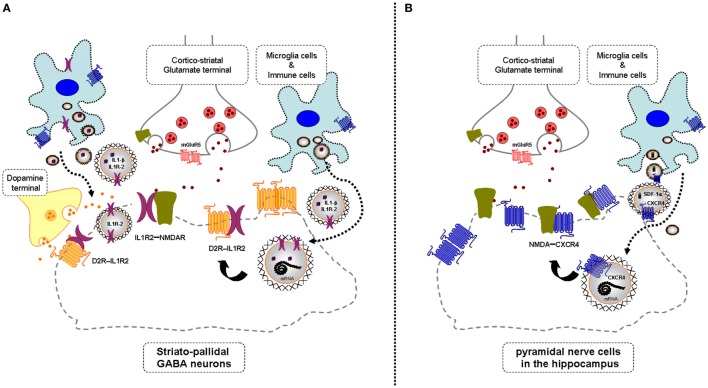
Figure 1.
Illustration of the potential chemokine and cytokine receptor transfer via extracellular vesicle-volume transmission (VT) from immune and microglial cells to striatopallidal GABA neurons [containing dopamine (DA) D2Rs and NMDARs] and hippocampus pyramidal neurons (containing NMDA receptors) in mild inflammation. One mechanism is shown for how chemokine C-X-C chemokine receptor type 4 (CXCR4) and cytokine receptor IL1-R2 including their mRNAs can produce schizophrenia-like symptoms in neuroinflammation. These receptors may be transferred via extracellular vesicle-mediated VT from immune cells, activated microglia, and/or astroglia to nerve cells containing DA D2R and NMDA receptors. Upon internalization, the receptors CXCR4 and IL1-R2 can according to the triplet puzzle theory (see Table 1) form complexes with DA D2R and NMDAR as illustrated here. (A) is shown the D2R-interleukin 1 receptor type II (IL1R2) heteromers in striatopallidal GABA neurons and how they reach the plasma membrane NMDAR via early endosomes and recycling endosomes. (B) is shown the NMDAR-CXCR4 heteromers in the pyramidal nerve cells in the hippocampus with microglial extracellular vesicles containing CXCR4 and also SDF-1alpha reaching the NMDAR in the plasma membrane via internalization and endosomes in the pyramidal cells. Through the development of novel allosteric receptor–receptor interactions in such heteroreceptor complexes, D2R and NMDAR signaling may become pathologically altered contributing to schizophrenia-like symptoms.