Abstract
Introduction
Miescher’s cheilitis is clinically characterized by persistent swelling of the lip(s). Its pathogenesis is still unknown. Histopathologically is characterized by sub-epithelial edema, increased number of dilated lymphatic vessels and an inflammatory infiltrate and/or non-caseating/non- necrotic granulomas. Even if the disorder must be controlled by medical therapy, surgery may be required to treat most severe cases.
Presentation of the case
We report a 30-year-old man who presented a persistent swelling of both lips since 8 years, previously treated with intralesional steroid and immunosuppressive therapy. Clinical examination did not show facial nerve palsy or other associated conditions. On the base of clinical and histopathological findings, a diagnosis of Miescher’s syndrome was made. Patient underwent Conway’s reduction cheilopasty repaired with local flaps. At one-year follow-up, the patient does not show local recurrence of the deformity; both oral continence and lip sensation are preserved.
Discussion
Because of its extreme rarity and unknown etiopathogenesis, Miescher’s cheilitis receives poor attention and may often remain misdiagnosed. Several medical therapies are proposed, in particular steroids and immunosuppression. Even if medical therapy remains the main treatment, surgery may be required.
Conclusion
Satisfactory results have been obtained combining medical therapy and surgical approach.
Keywords: Cheilitis granulomatosa, Miescher’s cheilitis, Lip, Swelling of the lips, Cheiloplasty, Case report
1. Introduction
Miescher’s cheilitis is a chronic disfiguring condition clinically characterized by persistent swelling of the lips, consisting in a granulomatous cheilitis [1]. The etiology of CG is still unknown, but a genetic predisposition may be possible [2]. It presents a series of closely related disease, characterized by lip swelling, such as sarcoidosis, Crohn’s disease, foreign body reaction, mycobacterial infections (tubercolosis, leprosy and atypical mycobacteria infection), deep fungal infection, contact allergy and dental infections. Therefore, diagnosis of CG is a diagnosis of exclusion and all major pathologies that can mimic this condition should be rule out to start the therapy, avoiding the exacerbation of the disease itself [3]. Histopathologically, it is characterized by sub-epithelial edema, increased number of dilated lymphatic vessels, inflammatory infiltrate and non necrotic and non caseating granulomas, consisting of lymphocytes and epithelioid histiocytes. Traditionally, medical therapies represent the first choice of treatment. It includes biologic agents, immunomodulators and intralesional infiltration of steroids [4], [5], [6], [7] Even if reduction cheiloplasty remains the only real effective solution for unresponsive cases, Miescher’s chelitis granulomatosa needs medical therapy to stabilize the surgical outcome and to prevent recurrence of the pathology. We herein report a case of Miescher’s cheilitis, unusual for its extreme severity, for the simultaneous involvement of both the lips completely unresponsive to the previous medical treatments.
2. Case report
A 30-year-old man of African descent came to our attention because of an extremely severe swelling involving both lips (Fig. 1). Such condition began in 2006 with the involvement first of the upper, followed by the lower lip. The disease progressively worsen up to the present. Both past medical and family history were unremarkable. Tuberculosis, sarcoidosis and Crohn’s disease were excluded by Chest High-resolution computed tomography (HRCT), colonoscopy and intestinal biopsy. Neurologic examination did not showed peripheral facial nerve palsy. The patient had already experienced several medical treatments including intra-lesional steroid injections (triamcinolone) and systemic steroids (prednisolone) with progression of the lip edema and off-label anti-TNF-alfa therapy (infliximab 5 mg/kg every 8 weeks) which was able to stabilize the disease. Local physical examination reported severe swelling of both lips. The superficial mucosa looked translucent, dry, with paramedian brownish dotting and fissured chaps. Consistency of the lips was firmly elastic, thus to limit facial mimic. Intra oral examination showed no particular tissue abnormalities, neither fissured tongue or lingua plicata. The patient referred lowered local sensation, functional limitation, but, above all, dramatic social embarrassment with a complete lack of confidence.
Fig 1.
Frontal preoperative view showing diffuse severe enlargement of both the lips, with fissuring in the midline of the lower.
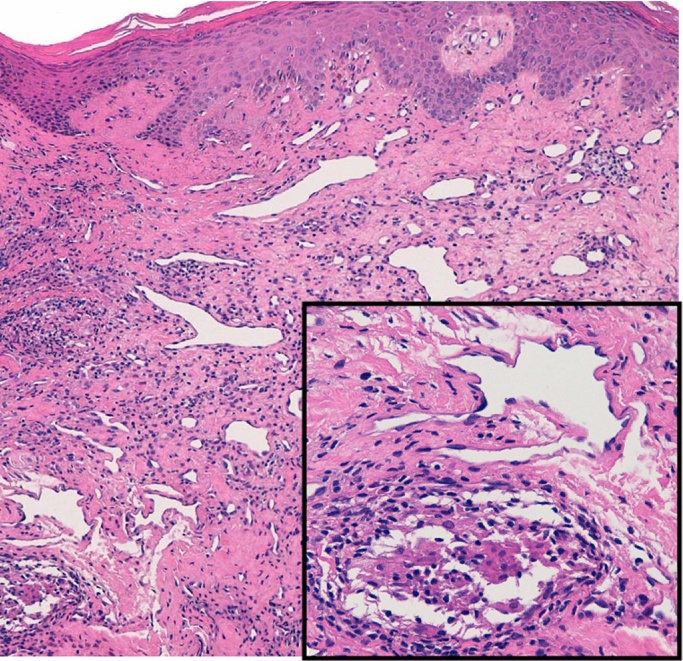
An incisional biopsy was taken from the upper lip. Histopathological examination showed numerous dilated lymphatic vessels and a mild inflammatory infiltrate, composed of lymphocytes and rare non caseating epithelioid granulomas in the subepithelial connective tissue (Fig. 2), consistent with a diagnosis of Miescher’s cheilitis. In vitro studies from a biopsy fragment revealed a mixed CD4+ and CD8+ T lymphocyte population able to produce high levels of Interferon (IFN-)-gamma and Tumor necrosis factor (TNF-)-alfa, consistent with the granulomatous inflammation (data not shown).
Fig. 2.
Histopathological examination of an incisional biopsy taken from the upper lip showed numerous dilated lymphatic vessels and a mild inflammatory infiltrate composed of lymphocytes and rare non-caseating granulomas in the subepithelial connective tissue (inset), consistent with a diagnosis of Miescher’s cheilitis.
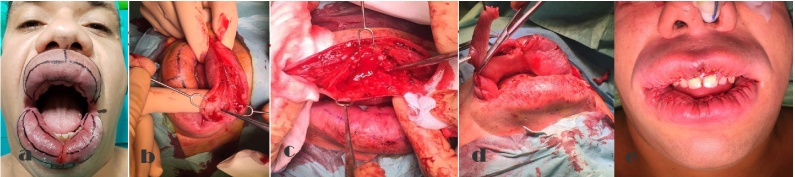
After a clinically stable preoperative period of two years with no further increase of lip dimensions, achieved with anti-TNF-alfa therapy, the patient underwent a surgical procedure. To reduce the pronounced anterior projection of the vermillion, the patient underwent a transverse sickle-shaped mucosa en block removal between 1.2 and 1.5 cm dorsal to the vermillion border, basing on Conway’s technique [8] (Fig. 3). Intra- and extra oral mucosal flaps were harvested to isolate and remove all the edematous tissue, which involved part of the orbicularis muscle. Macroscopically infiltrated muscle was also removed. Once the area was completely remodeled, the excess of mucosa was removed and the defect was closed in a double layer. After 12-months follow-up, the patient did not show local recurrence of the disease and the oral continence was preserved, with normal lip sensation (Fig. 4).
Fig. 3.
(a) Preoperative frontal view; (b) and (c) Transverse sickle-shaped mucosa en block removal between 1.2 and 1.5 cm dorsal to the vermillion border; (d) Removal of the mucosal excess; (e) Immediate postoperative frontal view.
Fig. 4.
One year post op follow-up frontal view.
3. Discussion
In 1945 Miescher [9] described a mono-symptomatic or oligo-symptomatic disease consisting in a granulomatous cheilitis, actually regarded as the most common manifestation of Melkersson-Rosenthal syndrome, which includes CG, facial palsy and fissured tongue [10]. It is estimated that the incidence of CG is 0,08% in the population [11].
Miescher’s cheilitis consists in an inflammatory disorder with non-infectious and non-necrotic granulomas and it appears as a painless enlargement of the lips, with or without facial edema, producing both aesthetic and functional deformities. Usually, it appears during the second decade of life, affecting mostly women, with no racial or ethnic predilection and it regresses with age. Although different medical treatments have been proposed, including intra-lesion injections of steroids or immune-modulator drugs [4], [5], [6], [7], surgical therapy often remains the only solution to treat unresponsive cases. This condition limits the social life due to severe embarrassment, especially in the most dramatic forms. Cheiloplasty acts the most efficient management of these unresponsive and disfiguring conditions, providing good aesthetic results and functional recovery even if the medical therapy needs to be administered [12], [13].
Due to its extreme rarity, Miescher’s cheilitis receives poor attention and may often remain misdiagnosed. Even if it is very difficult to correlate Miescher’s cheilitis to specific etiologic factors, probably the disorder is a poly-etiological disease based on genetic or acquired predisposition, associated to functional disturbance of autonomous nervous system resulting in a granulomatous reaction. [14] It may mimics angioedema but it does not respond to antihistamines or steroids. Although it may resolve spontaneously, after several recurrences it could become chronic, resulting in multiple non-infective and non-necrotic granulomas.
Granulomatous cheilitis usually affects only the upper lip [15], [16], [17] less frequently only the lower lip, and only rarely, as in our case report, both lips. Even if some permanent facial involvement has been reported following multiple attacks, facial nerve weakness usually resolves spontaneously. Sometimes patients may report pain or burning sensation, especially in intraoral involvement. Rarely, it appears in association with systemic symptoms such as fever, regional lymph nodes enlargement and general malaise [18], [19]. Miescher’s cheilitis may present alone or in conjunction with other chronic diseases (like Down’s syndrome, sarcoidosis, Crohn’s disease, psoriasis, thyroiditis, kerathitis, diabetes mellitus, ocular palsies, leprosy and multiple sclerosis.) In the latest stages of the disorder, non caseating granulomas can be present in the chorion even if their absence does not exclude the condition. Differential diagnosis should include every condition caused by granulomas, all the chronic forms of macrochelia and facial edema.
4. Conclusion
The medical treatment of Miescher’s cheilitis often results inefficient, requiring surgical treatment for satisfactory results. Reduction cheiloplasty is proven to be an effective method to correct the deformity, recovering both functional and satisfactory aesthetic appearance, when previous therapies failed. In any case, medical therapy is mandatory in post-surgical period to maintain the surgical result.
Conflict of interest
All authors disclose any financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work.
Financial disclosure
None.
Author contribution
All authors have contributed to create the paper.
Funding/Support
No sources of funding sponsored this study.
Ethical approval
All the procedure performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The patient’s consent was obtained for the case report.
This case report is compliant with the SCARE Guidelines [20].
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Dott. Alessandro Innocenti.
References
- 1.Nazzaro G., Muratori S. Cheilitis granulomatosa associated with lupus eritematosus discoid and treated with methotrexate: report of a case. An. Bras. Dermatol. 2015;90(3):200–202. doi: 10.1590/abd1806-4841.20153762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smeets E., Fryns J.P., Van den Berghe H. Melkersson-Rosenthal syndrome and de novo autosomal t(9;21)(pl 1; pl1) translocation. Clin. Genet. 1994;45:323. doi: 10.1111/j.1399-0004.1994.tb04041.x. [DOI] [PubMed] [Google Scholar]
- 3.El-Hakim, Chauvin Orofacial granulomatosis presenting as lip swelling. J. Oral Maxillofac. Surg. 2004;62:1114–1117. doi: 10.1016/j.joms.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Van der Waal R.I., Schulten E.A., van de Scheur M.R., Starink T.M., van der Wall I. Cheilitis granulomatosa: overview of 13 patients with long-term follow-up results of management. Int. J. Dermatol. 2002;41:225–229. doi: 10.1046/j.1365-4362.2002.01466.x. [DOI] [PubMed] [Google Scholar]
- 5.Bacci C., Valent M.L. Successful treatment of cheilitis granulomatosa with intralesional injection of triamcinolone. J. Eur. Acad. Dermatol. Venereol. 2010;24:363–364. doi: 10.1111/j.1468-3083.2009.03466.x. [DOI] [PubMed] [Google Scholar]
- 6.Rose A.E., Leger M., Chu J., Meehan S. Cheilitis granulomatosa. Dermatol. Online J. 2011;17(10):15. [PubMed] [Google Scholar]
- 7.Barry O., Barry J., Langan S., Murphy M., Fitzgibbon J., Lyons J.F. Treatment of granulomatous cheilitis with infliximab. Arch. Dermatol. 2005;141:1080–1082. doi: 10.1001/archderm.141.9.1080. [DOI] [PubMed] [Google Scholar]
- 8.Mouly R. Correction of the hypertrophy of the upper lip. Plast. Reconstr. Surg. 1970;462:262–264. doi: 10.1097/00006534-197009000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Miescher G. Über die essentielle granulomatöse Makrocheilie (granulomatöse Cheilitis) Dermatologica (Basel) 1945;91 (57 64) [Google Scholar]
- 10.Oudrhiri Lamia, Chiheb Soumiya, Marnissi Farida, Zamiati Soumaya, Benchikhi Hakima. Successful treatment of Miescher’s cheilitis in Melkersson-Rosenthal syndrome with betamethasone injections and doxycycline. Pan Afr. Med. J. 2012;13:75. [PMC free article] [PubMed] [Google Scholar]
- 11.Hornstein O.P. Melkersson-Rosenthal syndrome: a neuro-muco-cutaneous disease of complex origin. Curr. Prob. Dermatol. 1973;5:117. [PubMed] [Google Scholar]
- 12.Kruse-Losler B., Presser D., Metze D., Joos U. Surgical treatment of persistent macrocheilia in patients with Melkersson-Rosenthal syndrome and cheilitis granulomatosa. Arch. Dermatol. 2005;141(9):1085–1091. doi: 10.1001/archderm.141.9.1085. [DOI] [PubMed] [Google Scholar]
- 13.Worsaee N., Christensen K.C., Schiodt M. Reibel Melkersson-Rosenthal syndrome and cheilitis granulomatosa: a clinicopathological study of thirty-three patients with special reference to their oral lesione. J. Oral Surg. Oral Med. Oral Pathol. 1982;54:404–413. doi: 10.1016/0030-4220(82)90387-5. [DOI] [PubMed] [Google Scholar]
- 14.Ridder G.J., Fradis M., Löhle E. Cheilitis granulomatosa Miescher: treatment with clofazimine and review of the literature. Ann. Otol. Rhinol. Laryngol. 2001;110(10):964–967. doi: 10.1177/000348940111001013. [DOI] [PubMed] [Google Scholar]
- 15.Zimmer W.M., Rogers R.S., III, Reeve C.M. Orofacial manifestations of Melkersson-Rosenthal syndrome. A study of 42 patients and review of 220 cases from the literature. Oral Surg. Oral Med. Oral Pathol. 1992;74:610. doi: 10.1016/0030-4220(92)90354-s. [DOI] [PubMed] [Google Scholar]
- 16.Allen C.M., Camisa C., Hamzeh S. Chelitis granulomatosa: report of six cases and review of the literature. J. Am. Acad. Dermtol. 1990;23:444. doi: 10.1016/0190-9622(90)70238-d. [DOI] [PubMed] [Google Scholar]
- 17.Shaikh A.B., Arendorf T.M., Darling M.R. Granulomatous cheilitis: a review and report of a case. Oral Surg. Oral Med. Oral Pathol. 1989;67:527. doi: 10.1016/0030-4220(89)90267-3. [DOI] [PubMed] [Google Scholar]
- 18.Van der Waal R.I., Schulten E.A., van de Scheur M.R., Wauters I.M., Starink T.M., van der Waal I. Cheilitis granulomatosa. J. Eur. Acad. Dermatol. Venereol. 2001;15:519–523. doi: 10.1046/j.1468-3083.2001.00353.x. [DOI] [PubMed] [Google Scholar]
- 19.Hornstein O.P. Melkersson-Rosenthal syndrome: a neuromucocutaneous disease of complex origin. Curr. Prob. Dermatol. 1973;5:117–156. [PubMed] [Google Scholar]
- 20.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S. Orgill DP and the SCARE Group. The SCARE statement: consensus-baed surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]