Abstract
Context
Rosacea fulminans is a rare skin disorder with a multifactorial etiology. Stress is one of the common precipitating factors of this condition but is not often targeted in treatment. Isotretinoin is considered part of the first-line therapy for this condition but, in cases where its use is restricted, other therapeutic interventions as part of an integrative approach may be effective.
Patient Concerns
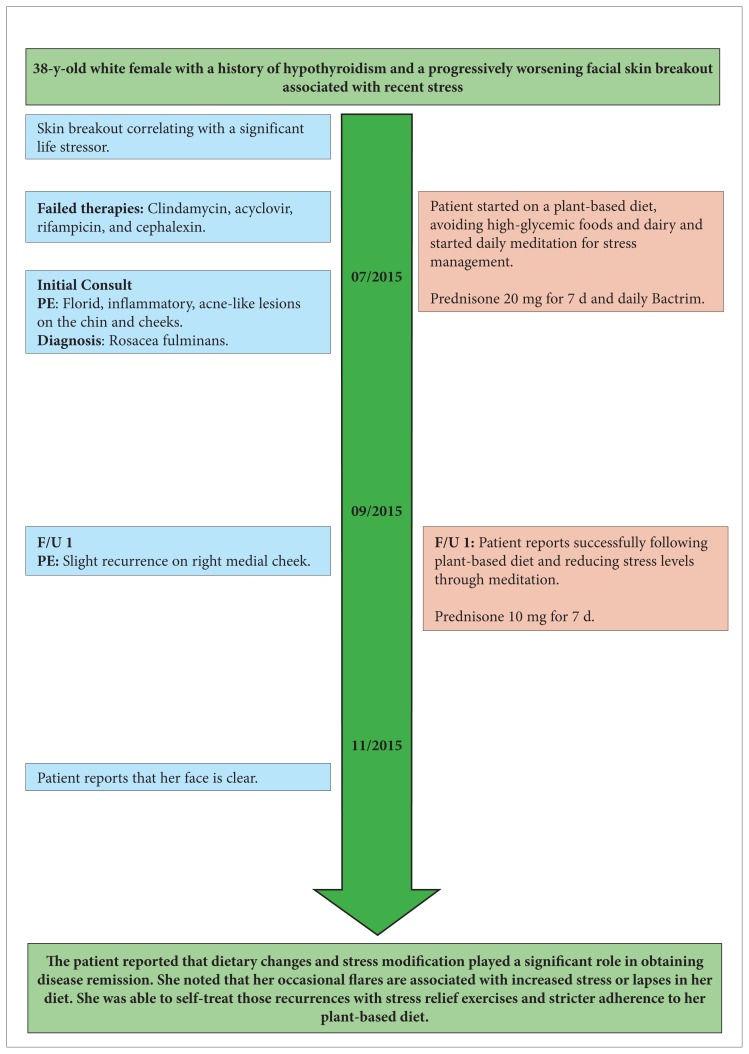
A 38-y-old female presented with rosacea fulminans brought on by an acutely stressful event. After multiple failed therapies, she experienced resolution of her symptoms with a combination of systemic corticosteroids, antibiotics, diet modification, and stress reduction, with the treatment of stress playing a significant role.
Conclusions
Stress management and diet modification are key adjunctive therapies in the treatment of rosacea fulminans and need to be addressed more often in treatment. In cases where patients are reluctant or unable to take isotretinoin, an integrative approach may be effective in achieving symptomatic improvement.
Rosacea fulminans, also known as pyoderma faciale, is a rare skin disorder that manifests as an acute onset of inflamed papules, pustules, coalescing nodules, and associated erythema of the nose, chin, and malar regions. It is primarily seen in women in their 20s and 30s but has been seen in males and children in isolated cases.1,2 The true etiology is unknown but is considered multifactorial, implicating vascular hyperactivity, genetic factors, hormonal fluctuations, and stress, among others.3 Stress, although often touted as a precipitating or aggravating factor in many skin conditions including rosacea fulminans, is often not actively considered as being of significant importance and hence not treated by dermatologists. This case details a 38-year-old female who presented with rosacea fulminans brought on by an acutely stressful event. After multiple failed therapies, she experienced resolution of her symptoms with a combination of systemic corticosteroids, antibiotics, diet modification, and stress reduction, with the treatment of stress playing a significant role in our clinical opinion.
Patient Information
A 38-year-old white female with a history of hypothyroidism presented with an acute occurrence of florid inflammatory acneiform lesions on the chin and cheeks that were indicative of pyoderma faciale. History revealed that the eruption began during, and progressively worsened soon after, admission of her brother to a drug rehabilitation center. The patient had previous skin reactions to stressful life situations as she endured a fluctuating course of seborrheic dermatitis of the scalp and periauricular area for 18 years, beginning with what became a troublesome marriage.
Prior to presentation, the patient attended multiple clinics and was offered various treatments without much relief. She was first prescribed oral clindamycin and acyclovir and later placed on a 9-day course of rifampin and cephalexin without improvement. One day prior to presentation, she received 80 mg of intramuscular triamcinolone and was started on oral trimethoprim/sulfamethoxazole (Bactrim) by another dermatologist. Despite reporting minimal subsidence at her first visit following systemic steroids and initiation of Bactrim, her pyoderma faciale was still clinically florid (Figure 1).
Figure 1.
Florid, Inflammatory, Acneiform Lesions on the Patient’s Chin and Cheeks That Indicate Rosacea Fulminans
Timeline
Intervention
The patient was prescribed an additional 20 mg of prednisone for 7 days and was to continue Bactrim until returning for follow-up after 2 months. The patient was counseled regarding the importance of approaching her skin condition in an integrative method, which would include lifestyle changes, diet modification, stress reduction, and exercise. She was strongly advised to cut out consumption of all dairy products, reduce or eliminate her intake of high-glycemic and processed foods, and consider a plant-based diet. To help with the high stress levels emanating from her severely troubled marriage and other family dynamics, it was suggested she try mindfulness-based meditation and seek counseling from a psychiatrist or clinical psychologist. Treatment with isotretinoin was not pursued in this patient because of her reluctance to take the drug after she reported side effects with past use for her acne, particularly staphylococcal infections.
Upon return to clinic 2 months later, the patient reported considerable improvement of her condition. During this period, she completely eliminated dairy from her diet and avoided red meats and high-glycemic foods. She routinely practiced deep breathing and meditation, but she did not seek the assistance of a psychiatrist. The inflammatory component of her pyoderma faciale markedly resolved, except for a slight recent recurrence on her right medial cheek (Figure 2). She was prescribed a week-long course of prednisone (10 mg daily) for the mild flare up and continued to take her daily Bactrim. Since that time, her skin has cleared (Figure 3), but she has noticed outbreaks associated with stress and addresses them by practicing meditation and avoiding stress-inducing situations.
Figure 2.
Two-month follow-up after diet modification and stress reduction. The photo shows that the patient had had only a mild recurrence on her right medial cheek
Figure 3.
Resolution of Rosacea Fulminans
Discussion
Rosacea fulminans is a rare skin condition that was first described in 1940 by O’Leary and Kierlan.4 This original study examined the cases of 13 female patients who presented with features that were atypical of classical acne. The presence of pustules coalescing to form larger lesions involving a majority of the face prompted the authors to term the condition pyoderma faciale. The term rosacea fulminans was not suggested until 1992 when Plewig et al5 detailed 20 additional cases that they stated were more representative of a variant of rosacea. Rosacea fulminans can be differentiated from acne because it primarily occurs in postadolescent women and is localized to the central face, sparing the neck, back, and chest. It has a more fulminant course than acne and is not associated with the presence of comedones.6 Since this condition was discovered, more than 60 cases have been reported in females as well as several in males and 1 in a 3-year-old girl.1,2,4,5,7,8
The underlying pathophysiology of rosacea fulminans is unknown but thought to be multifactorial including immunologic, hormonal, and vascular factors.3 The role of psychological stress and diet in the occurrence of rosacea fulminans has been acknowledged in the past but should be considered more often as a possible trigger and target for therapy. In Massa et al,8 8 patients had lesions that were preceded by a traumatic emotional experience, including death of a loved one, divorce, severe family turmoil, or a major medical problem. Facial dermatoses such as rosacea have been found to be more common in those who experience a higher intensity of stress from critical life events than those without such events. The level of stress and emotional state of patients can affect the onset and severity of the condition and uncontrolled stress may hinder the recovery process.9 In recent years, there have only been a handful of cases reported and few, if any, that address the contributions of stress management and diet adjustment in the treatment.1,7
Stress affects the skin thorough various mediators, with the hypothalamic-pituitary-adrenal (HPA) axis being the major player. In response to stress, the HPA axis is activated, resulting in the release of cortisol, which acts on the skin by altering the inflammatory pathway, cell proliferation, and skin barrier function. Stress also acts though catecholamines released from the adrenal medulla, which affect the skin by altering blood flow, immune function, and the function of cells. Neuropeptides such as substance P are secreted from nerves and inflammatory cells, and act as local stress responders mediating neurogenic inflammation.10
Elements of diet, including high-glycemic foods and dairy products, can be proinflammatory as evidenced by their association with acne, and they may contribute to the presentation of pustular lesions in rosacea fulminans.11 High-glycemic foods can cause acute hyperinsulinemia resulting in increased levels of androgens and insulin-like growth factor 1 (IGF-1). This process increases sebum production which ultimately obstructs the pilosebaceous unit, allowing for colonization with bacteria and release of inflammatory cytokines.12 Cow’s milk and its products act via a similar mechanism in that they naturally contain androgens, which increase IGF-1 in the body and lead to inflammatory skin symptoms.13 Adopting a Mediterranean diet including olive oil, fish, fruits, and vegetables, with a scarcity of high-glycemic foods, has been shown to be protective regarding the development of acne as well as cardiovascular disease.14
Pharmacologic therapy for rosacea fulminans typically involves a short course of oral corticosteroids to lessen inflammation followed by oral isotretinoin (0.5 to 1 mg/kg daily) for 4 to 6 months.15 Other therapies including oral and topical antibiotics have had less success, although there have been cases where dapsone has been helpful.16 Our patient was unresponsive to multiple antibiotics early in the course of her disease and began to see improvement with the addition of corticosteroids. Complete resolution of her condition was not achieved until she addressed the stress in her life that was perpetuating her rosacea fulminans.
Mechanisms for reducing stress include, but are not limited to, meditation, yoga, and counseling. This patient was specifically encouraged to try meditation as a way to cope with her stress. Meditation can blunt the body’s stress response by affecting the HPA axis and, ultimately, decreasing cortisol levels, or at least minimizing their increase in response to stress. A study regarding integrative body-mind training (IMBT) has shown that it can reduce salivary cortisol levels when compared to an equal amount of general relaxation time.17 This study also suggests that meditation or IMBT has a dose-response relationship, with a longer time spent meditating correlating with greater effect on cortisol levels. Addressing long-term stress and the associated elevation in cortisol can be beneficial in the altering the onset and course of cutaneous conditions as well as hypertension, diabetes, depression, and cancer.18
Conclusions
Our patient was a 38-year-old woman with florid rosacea fulminans for whom initial therapies failed. She was able to achieve remission once an integrative approach combining pharmacotherapy, diet modification, and stress reduction was employed to treat her condition. We believe it is important that dermatologists recognize the treatment options available beyond pharmacotherapy that can affect many cutaneous diseases, including stress management and diet.
References
- 1.Smith LA, Meehan SA, Cohen DE. Rosacea fulminans with extrafacial lesions in an elderly man: successful treatment with subantimicrobial-dose doxycycline. J Drugs Dermatol. 2014;13(6):763–765. [PubMed] [Google Scholar]
- 2.Firooz A, Firoozabadi MR, Dowlati Y. Rosacea fulminans (pyoderma faciale): Successful treatment of a 3-year old girl with oral isotretinoin. Int J Dermatol. 2001;40(3):203–205. doi: 10.1046/j.1365-4362.2001.01138-5.x. [DOI] [PubMed] [Google Scholar]
- 3.Crawford GH, Pelle MH, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004 Sep;51(3):327–341. doi: 10.1016/j.jaad.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 4.O’Leary PA, Kierland RR. Pyoderma faciale. Arch Dermatol Syphilol. 1940;41(3):451–462. [Google Scholar]
- 5.Plewig G, Jansen T, Kligman AM. Pyoderma faciale: A review and report of 20 additional cases: is it rosacea? Arch Dermatol. 1992;128(12):1611–1617. doi: 10.1001/archderm.128.12.1611. [DOI] [PubMed] [Google Scholar]
- 6.Fender AB, Ignatovich Y, Mercurio MG. Pyoderma faciale. Cutis. 2008;81(6):488–490. [PubMed] [Google Scholar]
- 7.Razeghi S, Halvorson CR, Gaspari AA, Cross RK. Successful treatment of localized pyoderma faciale in a patient with Crohn’s disease. Gastroenterol Hepatol. 2013;9(8):541–543. [PMC free article] [PubMed] [Google Scholar]
- 8.Massa MC, Su WP. Pyoderma faciale: A clinical study of twenty-nine patients. J Am Acad Dermatol. 1982;6(1):84–91. doi: 10.1016/s0190-9622(82)70008-8. [DOI] [PubMed] [Google Scholar]
- 9.Orion E, Wolf R. Psychologic factors in the development of facial dermatoses. Clin Dermatol. 2014;32(6):763–766. doi: 10.1016/j.clindermatol.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Lyga J. Brain-skin connection: Stress, inflammation and skin aging. Inflamm Allergy-Drug Targets. 2014;13(3):177–190. doi: 10.2174/1871528113666140522104422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Veith WB, Silverberg NB. The association of acne vulgaris with diet. Cutis. 2011;88(2):84–91. [PubMed] [Google Scholar]
- 12.Smith RN, Mann NJ, Braue A, et al. A low-glycemic-load diet improves symptoms in acne vulgaris patients: A randomized controlled trial. Am J Clin Nutr. 2007;86(1):107–115. doi: 10.1093/ajcn/86.1.107. [DOI] [PubMed] [Google Scholar]
- 13.Adebamowo CA, Spiegelman D, Danby FW, et al. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52(2):207–214. doi: 10.1016/j.jaad.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 14.Skroza N, Tolino E, Semyonov L, et al. Mediterranean diet and familial dysmetabolism as factors influencing the development of acne. Scand J Public Health. 2012;40(5):466–474. doi: 10.1177/1403494812454235. [DOI] [PubMed] [Google Scholar]
- 15.Ribeiro L, Ramos-e-Silva M. Rosacea fulminans. Cutis. 2013;92(1):29–32. [PubMed] [Google Scholar]
- 16.Patterson CR, Wilkinson JD, Lewis FM. Rosacea fulminans confined to the nose. J Eur Acad Dermatol Venereol. 2009;23(9):1101–1102. doi: 10.1111/j.1468-3083.2009.03098.x. [DOI] [PubMed] [Google Scholar]
- 17.Fan Y, Tang YY, Posner MI. Cortisol level modulated by integrative meditation in a dose-dependent fashion. Stress Health. 2014;30(1):65–70. doi: 10.1002/smi.2497. [DOI] [PubMed] [Google Scholar]
- 18.Rabin BS. Stressor-induced alteration of health across the life span: There is more to it than immunology. Clin Appl Immunol Rev. 2005;2:207–224. [Google Scholar]