Fig. 1.
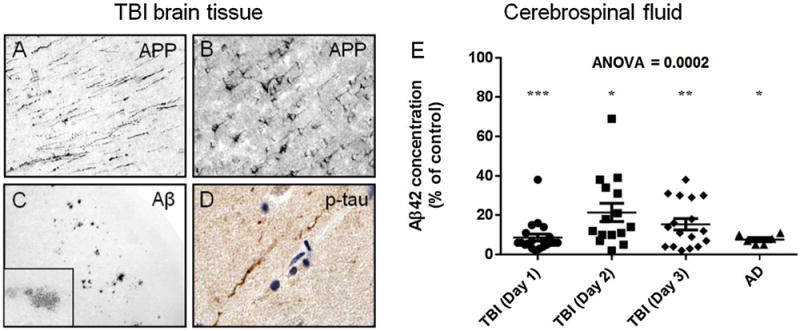
A–D: Brain tissue sections from a temporal cortex biopsy resected 12 h after severe TBI in a 39-year old subject from the University of Pittsburgh Brain Trauma Research Center (BTRC) were processed for immunohistochemistry using antibodies against the Aβ precursor protein (APP; polyclonal antibody anti-6, Athena), Aβ (antibody clone 10D5, Elan), and p-tau (antibody clone PHF-1, P. Davies, Albert Einstein College of Medicine). After severe TBI, APP accumulates in axons in the white matter (A), in cell bodies of pyramidal neurons in the grey matter (B), and Aβ deposits in diffuse Aβ plaques (C and inset). Rare profiles of phosphorylated tau (p-tau) immunoreactive fibers are detected in the gray matter (D; brown color is p-tau immunoreactivity, blue color is hematoxylin histological counterstain). E: Aβ1–42 peptide (Aβ42) concentrations (ELISA, Biosource) in cerebral spinal fluid (csf) from severe TBI patients (from the University of Pittsburgh BTRC; average age = 35.8 ± 15.7, range 17–65) at one, two, and three days after injury and from end-stage AD patients (from the University of Pittsburgh Alzheimer’s Disease Research Center; average age = 76.3 ± 10.2, range 63–91) are similarly reduced relative to levels in csf from cognitively normal control subjects (average age = 56.8 ± 14.5, range 25–78). *p < 0.05, **p < 0.01, ***p < 0.001 (Bonferroni multiple comparison post hoc test). Abbreviations: Aβ, amyloid-β; APP, Aβprecursor protein; p-tau, phosphorylated tau.
