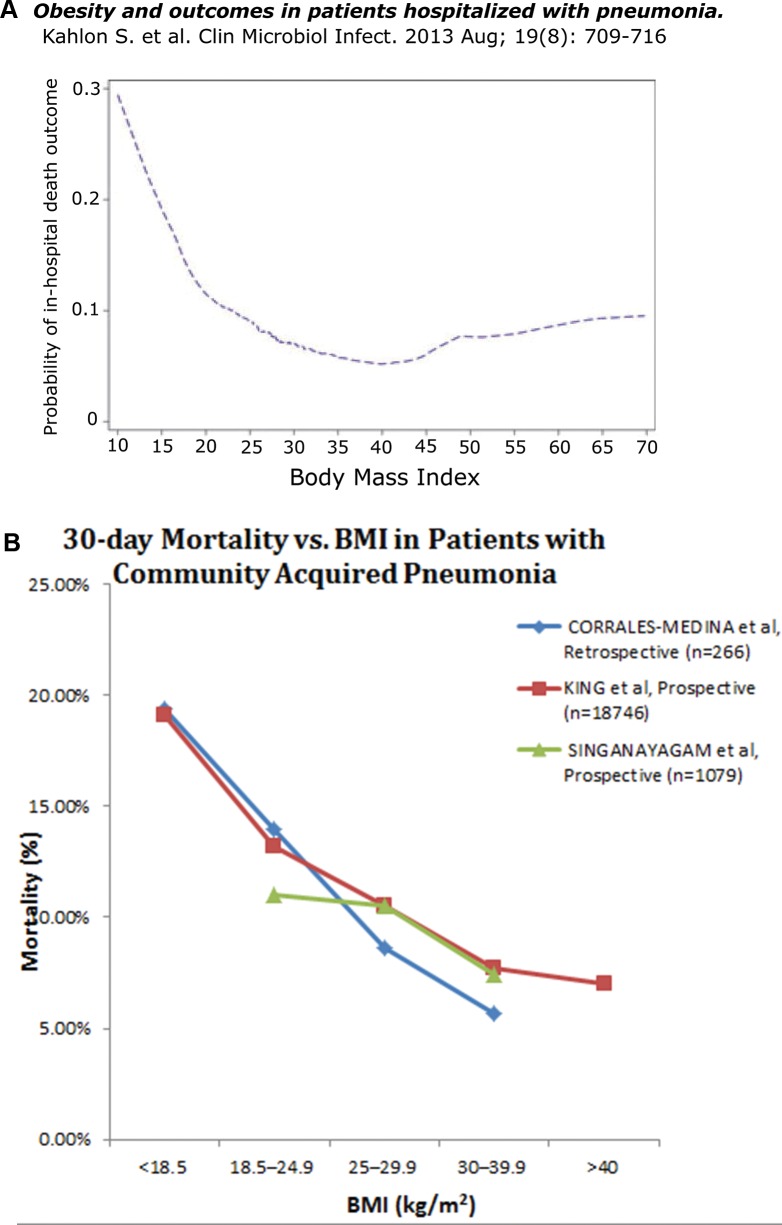
Figure 3.
(A) Among the 907 patients with community-acquired pneumonia in this prospective study admitted to six hospitals in Edmonton, Canada, the in-hospital mortality rate was inversely related to BMI (P < 0.001). The nadir in the mortality rate was at BMI = 40, with only a shallow slope upward at BMI levels over 40 that we associate with extreme obesity (17). (B) Three additional studies. 1) In this retrospective study of 266 patients with proven community-acquired pneumococcal (or Hemophilus) pneumonia, mortality at d 30 of admission is plotted as a function of BMI. The inverse relationship between mortality and BMI is significant at P < 0.01 in univariate and multivariate logistic regression analyses (18). 2) From this retrospective study of 18,746 patients with a discharge diagnosis of pneumonia (using data from the Department of Veterans Affairs), 30 d post-admission mortality is plotted as a function of BMI. In the univariate model, there is an inverse relationship between mortality and BMI (P < 0.0001). This relationship persists after adjusting for potential confounders in regression models, i.e., obesity is associated with decreased mortality (OR 0.86, 95% CI 0.74-0.99) and underweight patients had increased mortality (OR 1.40, 95% CI 1.14-1.73) (19). 3) The results of a prospective observational study from Edinburgh. The 30 d mortality is plotted against BMI for 1,079 patients diagnosed with community-acquired pneumonia. After Cox proportional hazards regression analysis, obesity is independently associated with decreased 30 d mortality (HR 0.53, 95% CI 0.29–.98) (20).