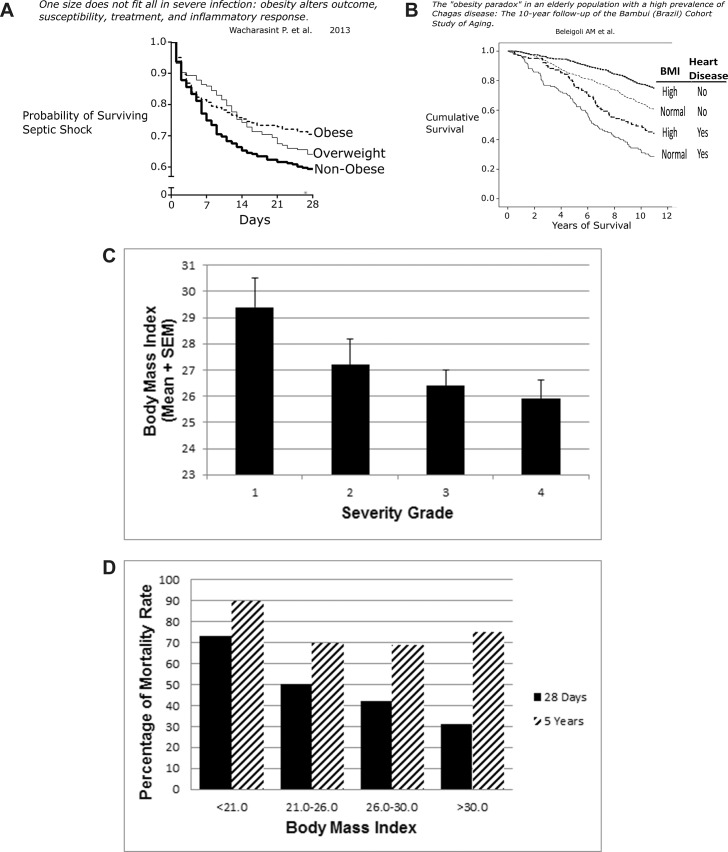
Figure 4.
(A) Survival with septic shock. Among 730 patients in hospital with septic shock, mortality recorded in the initial 28 d was inversely related to BMI (P < 0.02) (24). (B) This longitudinal study is from a small city in Brazil where longstanding endemic Chagas was stopped by 1970 through the use of insecticides. Residents over 60 years of age who acquired Chagas in their youth (n = 1271) were followed from (1997–2007) with normal BMI = 18.(5–24).9 and high BMI > 25. Heart disease was defined by EKG and B-type natriuretic peptide measurements. The Kaplan-Meier survival curves show that among patients without heart disease, 10-year survival of obese patients was better than their thinner, normal-weight counterparts. Patients with heart disease showed much lower survival than those free of heart disease, but those with heart disease and elevated BMI did better than patients with heart disease and normal weight (28). (C) Biliary tract infection. All patients in this group had biliary bacteria. Association of BMI and illness severity was significant (P < 0.02). Group 1: jaundice but no evidence of infection or inflammation. Group 2: fever, leukocytosis, tachypnea and tachycardia. Group 3: cholangitis, empyema of gallbladder, gangrenous cholecystitis or abscess. Group 4: bacteremia, hypotension, organ dysfunction (29). (D) Peritonitis with sepsis. The graph depicts the short-term mortality (28 d, black bar) and long-term mortality (5 years, striped bar) in 253 consecutive patients with peritonitis and sepsis who needed intensive care for more than 2 d postoperatively. Patients were severely ill, with high APACHE II scores, which correlated well with the mortality rate. Excluded were patients with acute pancreatitis or primary spontaneous bacterial peritonitis (31).