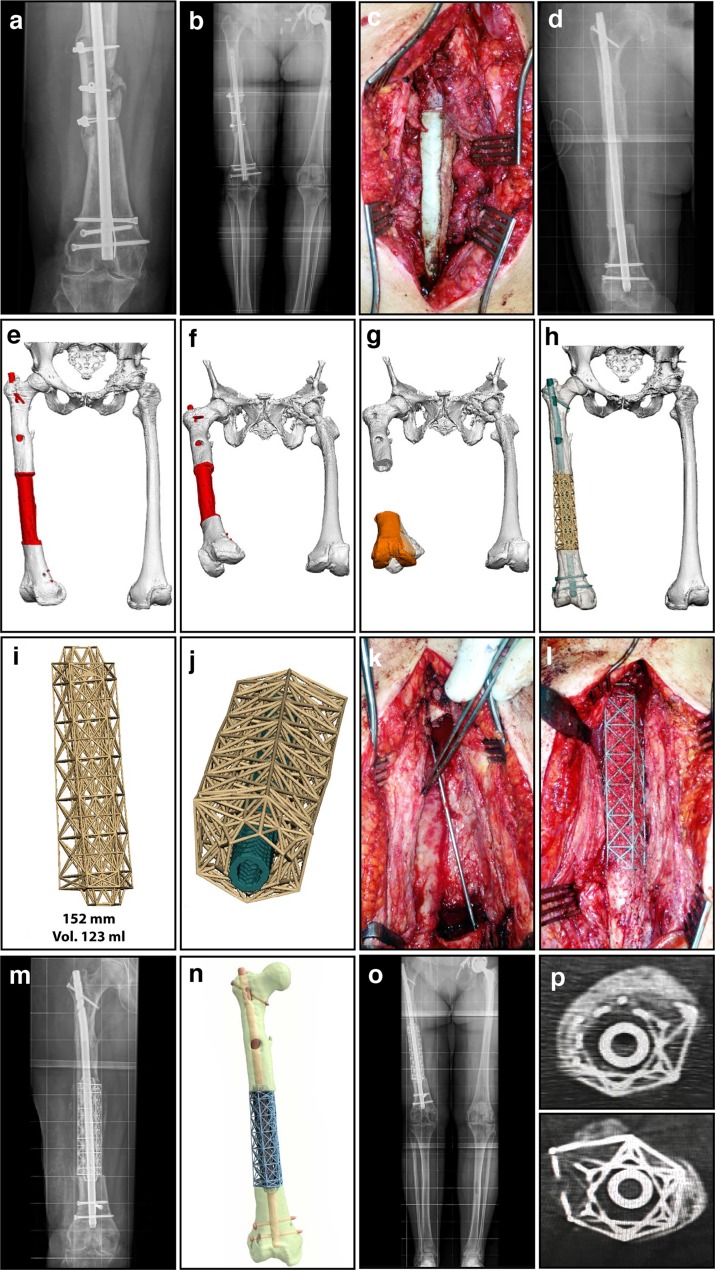
Figure 1.
Diaphyseal femoral segmental defect (15.2 cm) – infected non-union. (a) Anteroposterior (AP) radiograph of femoral mid-diaphyseal infected non-union, with a sequestrum consisting of the remnants of a prior intercalary allograft. (b) Long-standing radiograph of femoral mid-diaphyseal infected non-union, demonstrating alignment and limb lengths. (c) Intra-operative image during the 1st stage, illustrating a temporary antibiotic-loaded PMMA spacer. (d) Radiograph showing an antibiotic-loaded PMMA spacer fashioned to completely fill the defect, enveloping the bone at both the proximal and distal ends. (e) 3D modelling image showing the antibiotic spacer spanning the defect. (f) Axial view of 3D modelling image, demonstrating a 32° internal rotation deformity. (g) 3D virtual procedure images showing the distal fragment internal rotation of 32°, malaligned in 5° excess valgus, and flexed 9°, with a 12 mm residual limb length discrepancy. The planning for correcting the orientation of the distal fragment (amber), restoring its normal anatomic position by using the mirrored image of the contralateral uninvolved normal limb as a template. (h) 3D virtual procedure images showing the truss cage implant, designed to allow stabilization by a large diameter nail. (i) Final titanium truss implant design for the mid-diaphyseal femur, with tapered intramedullary extensions to improve torsional and translational stability. (j) The truss implant design here incorporates an axial hole designed to fit a suitable IM nail for stabilization of the mid-diaphyseal femur. (k) Intra-operative image during the second stage after the PMMA spacer was removed, demonstrating the membrane. (l) Intra-operative image during the second stage, following insertion of the titanium implant with bone graft packed into the open cells of the truss cage. (m) AP radiograph illustrating the final position of the implant, with a nail inserted through the truss cage locked proximally and distally. (n) Computer rendered image of the definitive reconstruction, stabilized with a nail inserted through the truss cage. (o) Long-standing radiograph of the lower extremities post-operatively, demonstrating excellent alignment and equal limb lengths. (p) CT scan at six-month post-operative confirming solid incorporation of bone graft, best demonstrated at the host/implant junctions proximally and distally.