Figure 7. Multiple NaV isoforms mediate the in vivo effects of P-CTX-1.
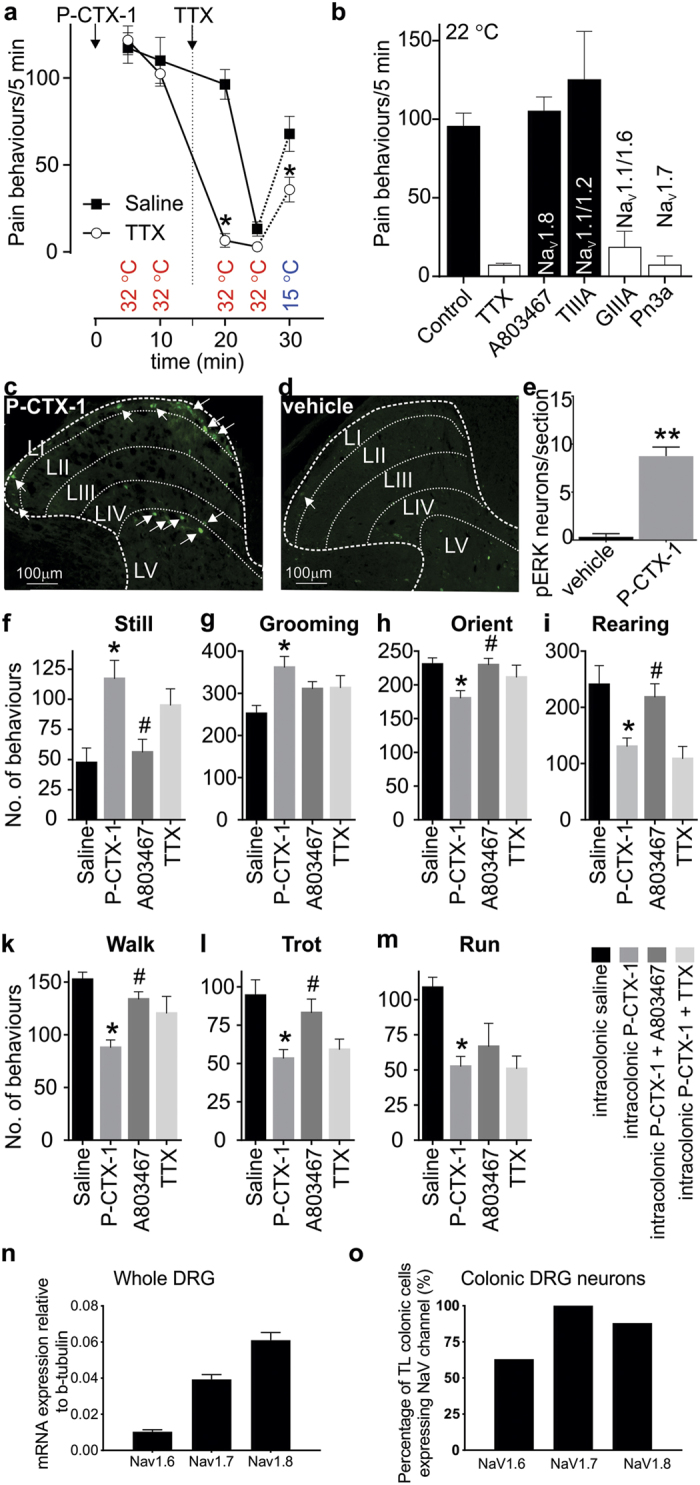
(a) Intraplantar injection of P-CTX-1 in C57BL/6 mice causes spontaneous pain behaviours at 32 °C which are completely blocked by local administration of TTX (2 μM). Cold allodynia evoked at 15 °C is partially reduced by TTX. (n = 5/group) (b) At ambient temperature, P-CTX-1-induced nocifensive behaviours were significantly decreased by co-administration of TTX (1 μM), the selective NaV1.7 inhibitor Pn3a (3 μM) and the NaV1.6 inhibitor GIIIA (10 μM), but not the NaV1.8 inhibitor A803467 (10 μM) or the NaV1.1/1.2 inhibitor TIIIA (10 μM). (n = 4–12 animals/group). (c) In vivo intra-colonic administration of P-CTX-1 (1 nM) activates nociceptive endings within the wall of the colon, leading to signalling into the dorsal horn and activation of neurons within the thoracolumbar spinal cord, as identified by pERK immunoreactivity (arrows). pERK-IR neurons were predominantly located in the nociresponsive superficial dorsal horn (laminae I) and also in laminae V. (d) Intracolonic administration of vehicle alone did not induce dorsal horn neuron pERK immunoreactivity. (e) Group data showing that P-CTX-1 evoked significant dorsal horn neuron activation (**p < 0.005) compared with vehicle administered mice (n = 3–4 animals/group). (f–m) A novel mouse model of P-CTX-1-induced visceral pain. Intracolonic administration of P-CTX-1 (50 μl, 10 nM) caused a significant (*p < 0.05 compared with Saline control) increase in (f) still and (g) grooming behaviours as well as a significant (*p < 0.05 compared with Saline control) decrease in (h) orienting, (i) rearing, (k) walking, (l) trotting and (m) running. These behavioural changes were reversed by A803467 (100 mg/kg; #p < 0.05 compared with P-CTX-1) but not intracolonic TTX (100 nM). (n = 6–12 animals/group) (n) NaV1.8 is the most highly expressed NaV isoform in whole thoracolumbar DRG (n = 5 animals/target). (o) NaV1.8 is highly expressed within thoracolumbar DRG neurons innervating the colon (88%: 21 out of 24 colonic neurons). Data are presented as mean ± SEM. Statistical significance (defined as p < 0.05) was determined using student’s t-test (a,e) or One-way ANOVA with Sidak’s multiple comparison (b,f–m).
