Abstract
Background
With an ageing HIV-positive population, sub-Saharan Africa is now facing a dual epidemic of communicable and non-communicable diseases (NCDs). This study aimed to assess trends in the prevalence of hypertension and factors associated with hypertension, among adults attending an ambulatory HIV clinic in Kampala, Uganda.
Methods
We conducted a retrospective chart review to identify patients with hypertension. We used a random number generator to select 400 patient charts from each year from 2009 to 2014. Blood pressure, age, body mass index (BMI), WHO disease stage and Karnofsky scores were extracted. Logistic regression was used to estimate the strength of the association between each of these factors and the presence of hypertension.
Results
In total, 1996 charts were included in this analysis. The mean age of participants was 31 years and 1311/1996 (65.7%) were female. The overall prevalence of hypertension was 418/1996 (20.9%). This rose from 16.9% in 2009 to 32.3% in 2013. Of the patients with hypertension, 96/418 (23.0%) were receiving adequate treatment. Patients >50 years of age had 3.12 times the odds of hypertension compared with patients aged 20–29 years (95% CI 2.00 to 4.85). Men had 1.65 times the odds of hypertension compared with women (95% CI 1.34 to 2.03) and patients with a BMI of 35–39 kg/m2 had 3.93 times the odds of hypertension compared with patients with a BMI <25 kg/m2.
Conclusions
The prevalence of hypertension is rising in the Ugandan HIV-positive population. There remains inadequate management and control of hypertension in this group highlighting the need to better integrate NCD care within the HIV clinical settings.
Key questions.
What is already known about this topic?
With advancements in HIV treatment and care, morbidity and mortality associated with HIV have decreased in many limited resource settings.
Since people are living longer lives and experiencing less complications as a result of HIV, patients are now presenting to primary care providers with non-communicable diseases, including hypertension.
At the population level, there is mixed evidence from low and middle income countries on the prevalence of hypertension among HIV-positive patients and its correlates.
What are the new findings?
We retrospectively performed a chart review on 1996 patients from 2009 to 2013 to identify hypertension and correlates among patients attending an ambulatory HIV clinic in Kampala, Uganda.
The overall prevalence of hypertension was 418/1996 (20.9%). This rose from 16.9% in 2009 to 32.3% in 2013.
Recommendations for policy
There is a need to better integrate NCD care within the HIV clinical settings.
Introduction
There has been a substantial reduction in HIV-associated morbidity and mortality as a result of the global scale-up of antiretroviral therapy (ART). This is particularly true in low and middle income countries, such as those in the sub-Saharan African region, which bear the largest burden of HIV.1–4 This reduction in mortality has substantially increased life expectancy, with estimates now approaching that of the general population.5–8 Now that HIV-positive individuals are living longer lives, there has been increased attention towards the emerging dual burden of HIV and non-communicable diseases (NCDs), such as hypertension.
Hypertension in HIV-positive patients has been reported to be as low as 8.7% and as high as 45.9% in low and middle income countries.9 10 Compared with the general population, some studies have suggested that hypertension is more prevalent among HIV-positive patients,9 11 whereas other studies have reported that patients with HIV have lower levels of hypertension, compared with the general population.12 13 Although there has been a comparable response to therapy for patients with hypertension with or without HIV infection,9 the dual burden of NCDs and HIV provides a challenge to weak healthcare systems in low and middle income countries.14 Establishing the magnitude of hypertension among HIV-positive patients and documenting the quality of care for these conditions within the HIV care setting provides an opportunity for improved care. The aim of this study was to determine the prevalence of hypertension, trends and associated factors among adults attending an ambulatory HIV clinic from 2009 to 2013 in Kampala, Uganda.
Methods
Study design and population
This was a retrospective study conducted at the Mulago AIDS Clinic, an outpatient clinic of Makerere University Joint AIDS Programme (MJAP), located in Kampala, Uganda. This clinic, supported by the President's Emergency Plan for AIDS Relief (PEPFAR), provides comprehensive HIV services to over 14 000 HIV-positive individuals, with the majority over the age of 18 years. Most of the patients live within a 20 km radius of the clinic. The HIV treatment guidelines (2014) at the clinic at the time of the study included eligibility for all patients with a CD4+ T-cell count of ≤500 cells/mm3, or the presence of WHO clinical disease stage 3 or 4, pregnancy, hepatitis B co-infection, HIV-associated nephropathy, or patients under 15 years of age. The clinic follows the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) clinical guidelines for the detection and management of hypertension.
Patients were eligible for inclusion if they were at least 18 years of age and visited the clinic between 2009 and 2014. Patients were randomly selected based on their year of intake into the HIV clinic and each patient was given a unique identifier at enrolment, so that patients do not appear on more than one sampling frame for each year. From this sampling frame, 400 patient charts from each year were randomly selected using a random number generator. For each of the 400 patient files selected, study variables were extracted.
Study variables
The primary outcome variable was prevalence of hypertension. In each year, patients were considered as hypertensive if their systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg at three consecutive measurements separated by at least 2 weeks and taken after 5–10 min of rest in a sitting position or if they were known to be hypertensive and on treatment.15 Adequate control for hypertension was defined as systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg at the second and successive visits.15
Additionally, we extracted data on demographic, clinical and biological characteristics including: WHO HIV disease stage, whether the patient was on ART, body mass index (BMI) and Karnofsky score that measures the degree of patient's functional impairment on a scale of 0–100.
Statistical analysis
Descriptive statistics were used to characterise the data. Prevalence of hypertension was calculated as the proportion of the study sample with a positive diagnosis, overall, and in each study year. Bivariable logistic regression was used to estimate the strength of the association between each study variable and the primary outcome, hypertension. A multivariable logistic model, adjusted for age and sex, was also constructed. Results are presented as ORs and adjusted ORs along with associated 95% CIs. All statistical tests were two-sided with α set at 0.05. Analyses were performed using STATA V.12 (StataCorp, College Station, Texas, USA).
Results
In total, 2000 (400 per year from 2009 to 2013) patients were randomly selected from a sampling frame of 13 550. In 2009, four patients did not have any information on the outcome, so the final analytic sample consisted of 1996 patients. Of these, 418 were considered hypertensive, an overall study prevalence of 20.9%. Table 1 displays patient demographic and clinical factors stratified by the presence of hypertension, while table 2 displays the characteristics of the sample by each year sampled.
Table 1.
Demographic and clinical factors stratified by hypertension
| No hypertension | Hypertension | ||
|---|---|---|---|
| n (%) | n (%) | p Value | |
| Age, years | |||
| <20 | 41 (2.7) | 5 (1.0) | <0.001 |
| 20–29 | 578 (38.2) | 144 (29.9) | |
| 30–39 | 629 (41.5) | 191 (39.7) | |
| 40–49 | 213 (14.1) | 99 (20.6) | |
| >50 | 54 (3.6) | 42 (8.7) | |
| Sex | |||
| Female | 1036 (68.3) | 273 (56.6) | <0.001 |
| Male | 481 (31.7) | 209 (43.4) | |
| BMI, kg/m2 | |||
| 18–24 | 1184 (78.8) | 329 (68.4) | <0.001 |
| 25–29 | 222 (14.8) | 97 (20.2) | |
| 30+ | 74 (4.9) | 37 (7.7) | |
| On ART | |||
| No | 281 (18.5) | 78 (16.2) | <0.001 |
| Yes | 1236 (81.5) | 404 (83.8) | |
| WHO HIV disease stage | |||
| Stage 1 and 2 | 1066 (70.3) | 385 (79.9) | <0.001 |
| Stage 3 and 4 | 451 (29.7) | 97 (20.1) | |
| Karnofsky score | |||
| 0–80 | 122 (9.6) | 14 (3.6) | <0.001 |
| 81–100 | 1146 (90.4) | 371 (96.4) | |
ART, antiretroviral therapy; BMI, body mass index.
Table 2.
Sample characteristics by year, 2009–2013
| n |
p Value | |||||
|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | ||
| Mean age (SE) | 33.7 (0.5) | 34.1 (0.4) | 33.5 (0.4) | 32.4 (0.5) | 31.7 (0.5) | — |
| Age, years | ||||||
| <20 | 8 | 3 | 4 | 6 | 25 | <0.001 |
| 20–29 | 139 | 124 | 135 | 176 | 148 | |
| 30–39 | 164 | 182 | 173 | 144 | 157 | |
| 40–49 | 62 | 71 | 65 | 53 | 61 | |
| >50 | 25 | 20 | 21 | 20 | 10 | |
| Sex | ||||||
| Female | 250 | 246 | 269 | 271 | 273 | 0.154 |
| Male | 148 | 154 | 129 | 128 | 131 | |
| BMI, kg/m2 | ||||||
| 18–24 | 332 | 324 | 291 | 286 | 280 | <0.001 |
| 25–29 | 45 | 52 | 77 | 80 | 65 | |
| 30+ | 20 | 22 | 24 | 31 | 55 | |
| WHO HIV disease stage | ||||||
| Stage 1 and 2 | 258 | 264 | 279 | 316 | 334 | <0.001 |
| Stage 3 and 4 | 140 | 136 | 119 | 83 | 70 | |
| Karnofsky score | ||||||
| 0–80 | 32 | 68 | 9 | 9 | 18 | <0.001 |
| 81–100 | 365 | 331 | 64 | 389 | 368 | |
BMI, body mass index.
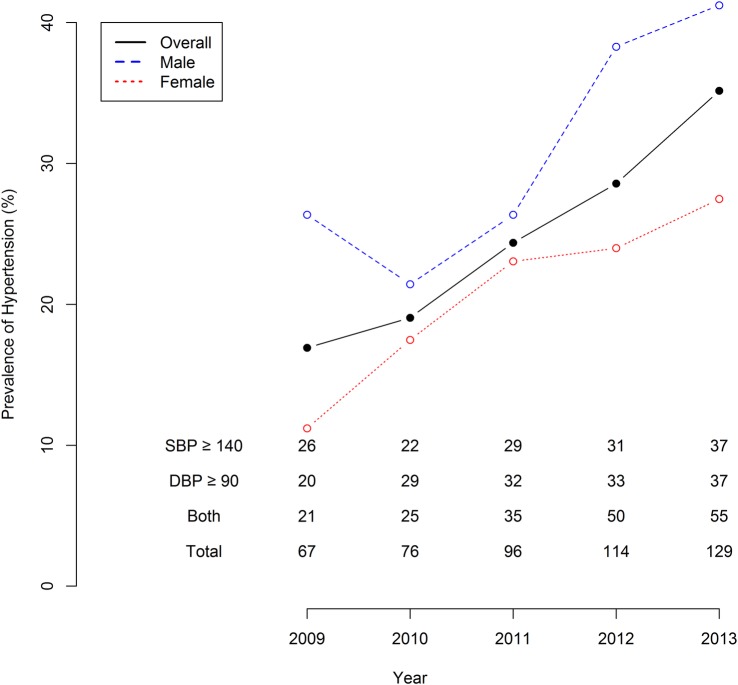
Figure 1 shows the prevalence of hypertension by study year. Each year, the prevalence of hypertension increased. The prevalence in 2009 was 67/396 (16.9%), in 2010 was 76/400 (19.0%), in 2011 was 96/400 (24.0%), in 2012 was 114/400 (28.5%), and in 2013 was 129/400 (32.3%). Of the patients with hypertension, 96/418 (23.0%) were receiving adequate treatment. The proportion of adequately treated patients rose from 14/53 (26.4%) in 2009 to 37/105 (35.2%) in 2013. Men had a higher prevalence of hypertension each year compared with women.
Figure 1.
Overall prevalence of hypertension by year of chart review. Note: Table indicates number of patients each year with each systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg, as well as SBP≥140 mm Hg and DBP≥90 mm Hg.
Table 3 displays the results of bivariable and multivariable logistic regression to estimate the strength of the association between each demographic and clinical factor and the presence of hypertension. Patients >50 years of age had 3.12 times the odds of hypertension compared with patients aged 20–29 years (95% CI 2.00 to 4.85). Men had 1.65 times the odds of hypertension compared with women (95% CI 1.34 to 2.03) and patients with a BMI of 35–39 kg/m2 had 3.93 times the odds of hypertension compared with patients with a BMI <25 kg/m2. Patients with a WHO disease staging of 3 or 4 had 0.60 times the odds of hypertension compared with patients with stage 1 or 2 (95% CI 0.46 to 0.76) and patients with a Karnofsky score of 81–100 had 2.82 times the odds of hypertension compared with patients with a score of 0–80 (95% CI 1.66 to 5.19). After adjusting for age and sex, the adjusted ORs changed minimally, indicating that confounding had a minimal influence on the model.
Table 3.
Bivariable and multivariable logistic regression identifying the strength of the association between demographic and clinical factors and presence of hypertension
| Unadjusted | Adjusted | |
|---|---|---|
| OR 95% CI | AOR 95% CI | |
| Age, years | ||
| <20 | 0.49 (0.17 to 1.15) | 0.43 (0.13 to 1.09) |
| 20–29 | Ref (—) | — |
| 30–39 | 1.22 (0.96 to 1.56) | 1.31 (1.00 to 1.73) |
| 40–49 | 1.86 (1.38 to 2.52) | 2.06 (1.45 to 2.91) |
| >50 | 3.12 (2.00 to 4.85) | 4.05 (2.40 to 6.83) |
| Sex | ||
| Female | Ref (—) | — |
| Male | 1.65 (1.34 to 2.03) | 2.02 (1.55 to 2.63) |
| BMI, kg/m2 | ||
| 18–24 | Ref (—) | — |
| 25–29 | 1.57 (1.20 to 2.05) | <0.01 |
| 30+ | 2.04 (1.43 to 2.89) | <0.01 |
| On ART | ||
| No | Ref (—) | — |
| Yes | 1.18 (0.90 to 1.56) | 0.24 |
| WHO HIV disease stage | ||
| Stage 1 and 2 | Ref (—) | — |
| Stage 3 and 4 | 0.60 (0.46 to 0.76) | <0.01 |
| Karnofsky score | ||
| 0–80 | Ref (—) | — |
| 81–100 | 2.82 (1.66 to 5.19) | <0.01 |
AOR, adjusted OR; ART, antiretroviral therapy; BMI, body mass index.
Discussion
This study sought to determine the prevalence, trend and correlates of hypertension among adults attending an ambulatory HIV clinic in Kampala, Uganda. We found a rise in the prevalence of hypertension from 2009 to 2013, from 16.9% to 32.2%. Similarly, HIV prevalence rose from 6.4% in 2005 to 7.3% in 2014 (The Joint United Nations Programme on HIV/AIDS (UNAIDS), Gap Report). This demonstrates a rising double burden of HIV and hypertension, consistent with reports that as the proportion of HIV-positive patients achieving viral suppression on combination ART grows larger and these patients age, they are experiencing a widening spectrum of non-AIDS-related diseases.1
Our study found an overall prevalence of 24.1% and a rising prevalence by year from 16.9% in 2009 to 32.3% in 2013. This is most likely due to the rising age of the patients accessing HIV care as well as the number of patients being put on antiretroviral therapy (ART). There might also be other factors which may not have been uncovered by the current study due to its retrospective nature. Compared with the general population in Uganda, the prevalence of hypertension in HIV-positive adults is within a similar range (21.2% vs 27.2%).16 Mateen et al10 in Uganda similarly reported a 28% prevalence of hypertension and 49% in those above 50 years with similar risk factors. In another Ugandan study, Sander et al9 reported a lower prevalence of hypertension 8.0%, although when they considered only one elevated blood pressure reading, the prevalence rose to 26.3%. In contrast to Sander et al,9 where 83% of participants diagnosed with hypertension were on antihypertensive medications, in our study only 20.9% were on recommended treatment for hypertension. In both studies, the most commonly used drugs were β-blockers and calcium channel blockers.9
Our results provide evidence that hypertension has become an important NCD in the HIV-positive population with prevalence rates similar to that of the general population. In addition, our study shows that management of HIV-positive patients with hypertension is still inadequate. This is partly explained by the current HIV care guidelines in Uganda, which do not routinely include an NCD programme for HIV-positive patients attending the ambulatory clinics. Furthermore, most of the effort from the government and international agencies is currently focusing on HIV, tuberculosis and malaria, with less attention to the rising burden of hypertension in the HIV ageing population. Justice1 recommends that focus must shift from a narrow interest in CD4 counts, HIV RNA and AIDS defining illnesses to determining the optimal management of HIV infection as a complex chronic disease in which the causes of morbidity and mortality are multiple and overlapping. We need a new paradigm of care with which to maximise functional status, minimise frailty and prolong life expectancy.1 The authors propose a composite index that summarises a patient’s risk of morbidity and mortality.
In this era of an ageing sub-Saharan African population on ART, we expect more patients to present with hypertension and other chronic conditions. This has become a substantial burden on resource-limited countries to manage a dual epidemic of infectious and chronic diseases. Few NCD programmes have been incorporated into HIV care and this highlights the importance of implementing screening, early diagnosis, and prevention measures for hypertension and other chronic diseases.
Our study has several strengths. The study was conducted in an ambulatory clinic, which serves a large proportion of the patients with HIV in urban Uganda. However, MJAP, being a centre of excellence in HIV, may not truly reflect what is happening elsewhere in the country where the access to expert service care may be more limited. Although we cannot use these data from a specialised urban HIV clinic to generalise hypertension care in Uganda, the findings demonstrate a missed opportunity for comprehensive care even among patients who frequently interface with healthcare providers. The findings therefore highlight a need for healthcare providers to develop indicators which can be used to monitor for improved care beyond HIV, in HIV-infected individuals with comorbidity. Additionally, the interpretation of our results must take into account some limitations. Most importantly, this was a chart review study and no patients were contacted; therefore, there were only a limited number of variables to extract and consider in the analysis. In particular, data on lifestyle factors important to hypertension, such as smoking status and alcohol intake, were sparse and not usable. Therefore, only a limited number of variables were available to construct a bivariable and multivariable model.
In conclusion, our study corroborates other studies that suggest an increasing prevalence of hypertension among HIV-positive patients in Uganda. Identifying risk factors will be important for clinicians to adequately manage a growing dual epidemic of infectious and chronic diseases in sub-Saharan Africa.
Footnotes
Handling editor: Soumitra Bhuyan
Contributors: RK and AK conceived of the study. FCS, AM and NK collected the data. DA and JIF conducted the analyses. EJM supervised the study. All authors contributed to the manuscript and approved the final draft for submission.
Competing interests: None declared.
Ethics approval: Research Ethics Review Board, School of Biomedical Sciences, Makerere University, Uganda.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Justice AC. HIV and aging: time for a new paradigm. Curr HIV/AIDS Rep 2010;7:69–76. 10.1007/s11904-010-0041-9 [DOI] [PubMed] [Google Scholar]
- 2.Deeks SG. Immune dysfunction, inflammation, and accelerated aging in patients on antiretroviral therapy. Top HIV Med 2009;17:118–23. [PubMed] [Google Scholar]
- 3.Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet 2008;372:293–9. 10.1016/S0140-6736(08)61113-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palella FJ Jr, Delaney KM, Moorman AC et al. . Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med 1998;338:853–60. 10.1056/NEJM199803263381301 [DOI] [PubMed] [Google Scholar]
- 5.May M, Gompels M, Delpech V et al. . Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ 2011;343:d6016 10.1136/bmj.d6016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cockerham L, Scherzer R, Zolopa A et al. . Association of HIV infection, demographic and cardiovascular risk factors with all-cause mortality in the recent HAART era. J Acquir Immune Defic Syndr 2010;53:102–6. 10.1097/QAI.0b013e3181b79d22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zwahlen M, Harris R, May M et al. . Mortality of HIV-infected patients starting potent antiretroviral therapy: comparison with the general population in nine industrialized countries. Int J Epidemiol 2009;38:1624–33. 10.1093/ije/dyp306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lohse N, Hansen AB, Pedersen G et al. . Survival of persons with and without HIV infection in Denmark, 1995–2005. Ann Intern Med 2007;146:87–95. 10.7326/0003-4819-146-2-200701160-00003 [DOI] [PubMed] [Google Scholar]
- 9.Sander LD, Newell K, Ssebbowa P et al. . Hypertension, cardiovascular risk factors and antihypertensive medication utilisation among HIV-infected individuals in Rakai, Uganda. Trop Med Int Health 2015;20:391–6. 10.1111/tmi.12443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mateen FJ, Kanters S, Kalyesubula R et al. . Hypertension prevalence and Framingham risk score stratification in a large HIV-positive cohort in Uganda. J Hypertens 2013;31:1372–8. discussion 78 10.1097/HJH.0b013e328360de1c [DOI] [PubMed] [Google Scholar]
- 11.Bloomfield GS, Hogan JW, Keter A et al. . Blood pressure level impacts risk of death among HIV seropositive adults in Kenya: a retrospective analysis of electronic health records. BMC Infect Dis 2014;14:284 10.1186/1471-2334-14-284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kayima J, Nankabirwa J, Sinabulya I et al. . Determinants of hypertension in a young adult Ugandan population in epidemiological transition-the MEPI-CVD survey. BMC Public Health 2015;15:830 10.1186/s12889-015-2146-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kavishe B, Biraro S, Baisley K et al. . High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Med 2015;13:126 10.1186/s12916-015-0357-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katende D, Mutungi G, Baisley K et al. . Readiness of Ugandan health services for the management of outpatients with chronic diseases. Trop Med Int Health 2015;20:1385–95. 10.1111/tmi.12560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black HR et al. . Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 16.Musinguzi G, Nuwaha F. Prevalence, awareness and control of hypertension in Uganda. PLoS ONE 2013;8:e62236 10.1371/journal.pone.0062236 [DOI] [PMC free article] [PubMed] [Google Scholar]