Summary
A question remains regarding differential effects of exposure-based vs. non-exposure-based therapies on specific PTSD symptom clusters. Traumatized emergency room patients were randomized to receive prolonged exposure (PE) or cognitive therapy (CT) without exposure. PE/CT had no differential effect on individual symptom clusters, and change in total PTSD score remained significant even after controlling for the reductions in all 3 symptom clusters. In addition, baseline levels of PTSD avoidance/intrusion/hyper-arousal did not moderate the effects of PE and CT on total PTSD symptom scores. Taken together, these findings challenge the notion that PE and CT are specifically, and differentially, useful in treating one particular PTSD symptom cluster.
Keywords: PTSD, Prolonged Exposure, Cognitive Therapy, Randomized Controlled Trial
INTRODUCTION
To date, trauma-focused CBT has gained considerable empirical support for effectiveness in treating PTSD (e.g. Bisson et al., 2007). However, direct comparisons between PTSD treatments with and without exposure have yielded inconclusive results (e.g., Taylor et al., 2003).
The efficacy of both Prolonged Exposure (PE) and Cognitive Therapy (CT) in treating PTSD has received considerable empirical support (Rauch, Eftekhari, & Ruzek, 2012; Paunovic & Öst, 2001, respectively). However, while many studies have assessed treatment effectiveness in terms of reduction in total PTSD severity (e.g. Powers, Halpern, Ferenschak, Gillihan, & Foaet, 2010), data is missing regarding the differential effect of PE/CT on individual PTSD symptom clusters of intrusion, avoidance/numbing, and hyper-arousal, and implicitly about their use in a more targeted manner to address specific PTSD symptoms (e.g. Foa, Keane, Friedman, & Cohen, 2009).
The original protocol for PE was developed using Emotional Processing Theory (e.g. Foa & Kozak, 1986), according to which avoidance perpetuates PTSD (e.g. Foa, 2006). However, the cognitive theory of PTSD (Ehlers & Steil, 1995) focuses on one’s catastrophic interpretation of the traumatic event. In line with this, CT has been shown to specifically target intrusive thoughts in PTSD, in both individual (Tarrier et al., 1999) and group (e.g. Antoni et al., 2009) psychotherapy.
To date, intervention studies looking at individual PTSD clusters have yielded mixed findings (e.g. Taylor et al., 2003). Also, some of these studies have failed to clearly define treatment protocols (Ironson, Freund, Strauss, & Williams, 2002). The present study, which is based on a secondary analysis of a previously published RCT (Shalev et al., 2012), aimed to fill these gaps by capitalizing on a large RCT that compared, head to head, CT (without the exposure component) and PE in recent civilian trauma survivors. Our main research questions were: (1) Do CT and PE have a differential effect on PTSD symptom clusters? (2) Do specific PTSD symptom clusters contribute differentially to the effect of CT/PE on PTSD severity? and (3) Do baseline levels of PTSD symptom clusters moderate the effects of CT and PE on total PTSD symptom severity?
METHOD
This report is based on data from the previously published Jerusalem Trauma Outreach and Prevention Study. For a complete and elaborated description of methods please see Shalev et al. (2012).
Participants
Participants were adult (ages 18–70) trauma survivors (mostly MVAs and terrorist attacks), who were admitted to a general hospital’s emergency services in Israel, between 2003–2007. They were contacted within 21 days of admission. Following initial telephone screening for acute posttraumatic symptoms, 756 participants have agreed to undergo a clinical assessment.
Measures
The Clinician Administered PTSD scale (CAPS; Blake et al., 1995) is a structured interview assessing the frequency and intensity of PTSD symptoms (APA, 2000) diagnostic criteria. A PTSD diagnosis required meeting DSM-IV-TR diagnostic criteria A through F, save the 1-month duration, as well as a CAPS total score of at least 40. The CAPS has established psychometric properties (Blake et al., 1995).
Procedure
Initial Clinical Assessment
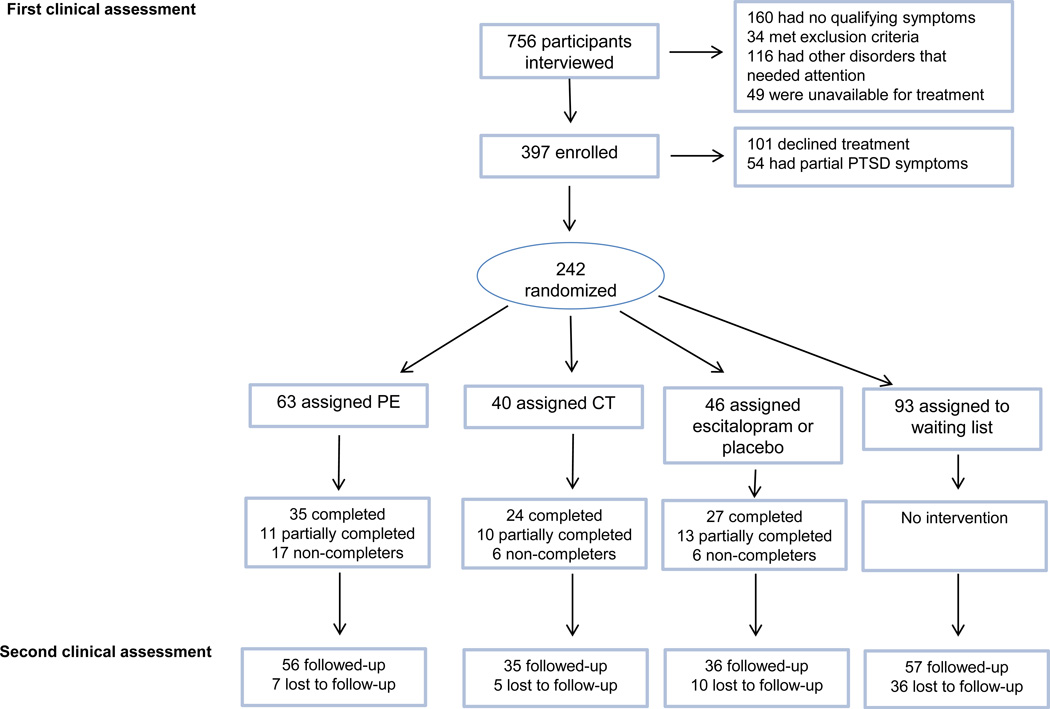
756 trauma survivors attended a first clinical assessment (CA-1). 242 participants with full PTSD, save the 1-month duration criterion, were randomized to treatment groups using equipoise-stratified randomization (Trivedi et al., 2006). Out of 4 original treatment conditions (PE, CT, treatment with SSRI vs placebo, and WL and subsequent delayed PE) we have compared here only participants from the PE (N=63 at CA-1) and CT (N=41 at CA-1) arms. See figure 1 for flow diagram of the full RCT.
Figure 1.
Patient flowchart of survivors of trauma for study comparing exposure-based, cognitive, and pharmacological interventions for PTSD.
Interventions
PE was administered according to the protocol in Hembree, Foa, and Dancu (1999). PE includes psychoeducation, breathing training, imaginal exposure, and in vivo exposure. CT was administered according to the protocol in Marks, Lovell, Noshirvani, Livanou, and Thrasher (1998). It includes identifying and challenging negative automatic thoughts and modifying underlying cognitive schemas. Importantly, the protocol contains no exposure. Clinical psychologists administered 12 weekly 1.5-hour sessions of PE/CT. Protocol adherence was found to be excellent.
Second Clinical Assessment
The second clinical assessment (CA-2) took place a mean (SD) 144.1 (35.2) days post-trauma. We have decided to analyze data from all participants allocated to treatment, whether they completed the entire therapy or not, as we have found that treatment completion was not associated with CAPS scores at CA-2. During CA-2, all CA-1 participants who could be contacted (N=56 for PE and N=33 for CT) were re-evaluated.
RESULTS
Baseline differences between the PE and CT groups
As can be seen in table 1, the PE and CT groups at baseline did not differ in age, duration of stay in ER, number of days from event to first and second clinical interview, and baseline CAPS scores.
Table 1.
Means, SDs and test statistics for baseline differences between the PE and CT groups
| PE (N=56) | CT (N=33) | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t(df) | p | |
| Age | 40.29 | 12.20 | 40.27 | 13.26 | t(87)=.01 | 1.00 |
| Duration of stay in ER | 4.79 | 4.25 | 8.93 | 13.37 | t(29.26)=−1.53 | .14 |
| # of days from event to first clinical interview | 18.32 | 4.49 | 19.18 | 4.40 | t(87)=−.88 | .38 |
| # of days from event to second clinical interview | 140.98 | 27.70 | 152.58 | 30.42 | t(87)= −1.84 | .07 |
| Total CAPS score at baseline | 73.11 | 21.21 | 70.09 | 13.61 | t(86.3)=.82 | .42 |
| CAPS score for avoidance/numbing symptoms at baseline | 29.73 | 8.76 | 29.67 | 6.68 | t(87)=.04 | .97 |
| CAPS score for intrusion symptoms at baseline | 21.11 | 8.34 | 19.00 | 5.67 | t(85.11)=1.42 | .16 |
| CAPS score for arousal symptoms at baseline | 22.27 | 7.44 | 21.42 | 5.77 | t(87)=.56 | .58 |
Additionally, there were no significant differences between the two groups in trauma type (χ2=2.21, df=2, p=.33) and inpatient department of admission (χ2=6.49, df=6, p=.37). The groups differed, however, in gender, with more females in the CT (78.8%) vs. the PE (46.4%; χ2=8.95, df=1, p<.01) group.
Differential effects of PE and CT on PTSD symptom clusters
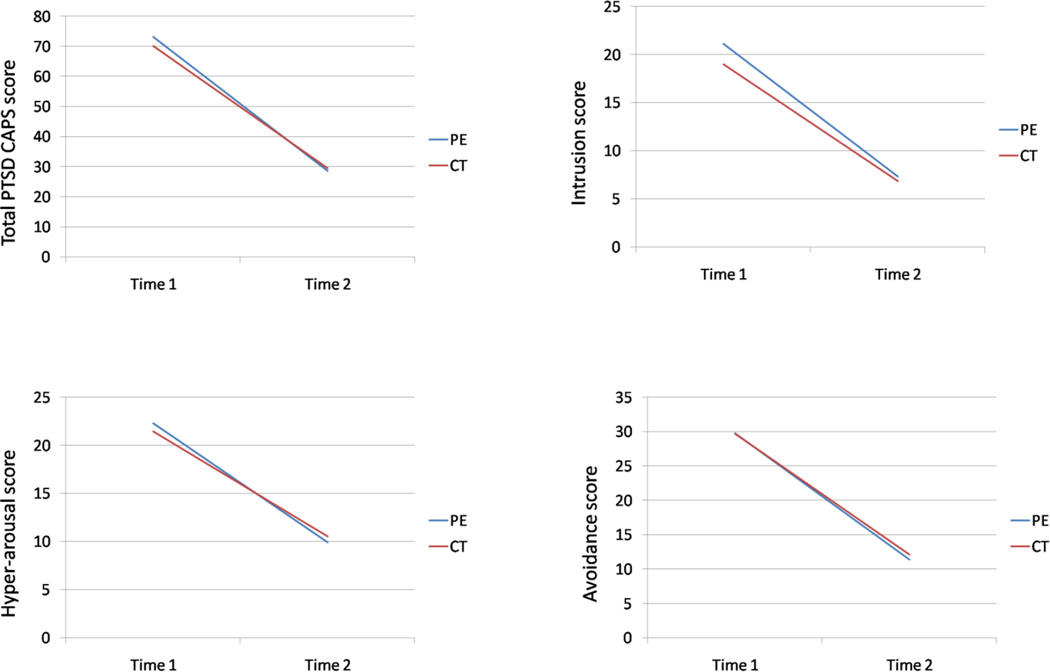
Repeated measures ANCOVAs, with gender as the covariate (Table 2), showed a significant main effect for time (pre- vs. post treatment), a non-significant group main effect (CT vs PE) and no group X time interactions for both total CAPS score and all underlying PTSD symptoms clusters (see Figure 2). Cohen’s d effect sizes (Cohen, 1988) were high (1.34 and higher for all significant effects).
Table 2.
Means, SDs, and test statistics for repeated-measures ANCOVAs (time, treatment type, and PTSD symptoms)
| PE (N=56) | CT (N=33) | F Time (1, 86) |
Cohen’s d (Time) |
F Treatment type (1, 86) |
F Time X Treatment type (1,86) |
|||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Total CAPS score T1 | 73.11 | 21.21 | 70.09 | 13.61 | 26.30*** (p=.000) |
1.73 |
.01 n.s. (p=.917) |
.20 n.s. (p=.659) |
| Total CAPS score T2 | 28.59 | 25.02 | 29.48 | 23.03 | ||||
| Avoidance/numbing CAPS score T1 | 29.73 | 8.76 | 29.67 | 6.68 | 18.67*** (p=.000) |
1.56 |
.22 n.s. (p=.644) |
.04 n.s. (p=.845) |
| Avoidance/numbing CAPS score T2 | 11.36 | 11.27 | 12.12 | 10.39 | ||||
| Intrusion CAPS score T1 | 21.11 | 8.34 | 19.00 | 5.67 | 30.57*** (p=.000) |
1.67 |
.29 n.s. (p=.593) |
.23 n.s. (p=.631) |
| Intrusion CAPS score T2 | 7.32 | 7.44 | 6.85 | 5.71 | ||||
| Hyper-arousal CAPS score T1 | 22.27 | 7.44 | 21.42 | 5.77 | 14.74*** (p=.000) |
1.34 |
.05 n.s. (p=.821) |
.31 n.s. (p=.578) |
| Hyper-arousal CAPS score T2 | 9.91 | 8.65 | 10.52 | 9.23 | ||||
p<.001
Figure 2.
Differential effects of PE and CT on total PTSD scores and individual PTSD symptom clusters
The moderating role of baseline symptom cluster levels
Next, we set out to examine the moderating role of baseline levels of avoidance/intrusion/hyper-arousal in the effects of PE and CT on participants’ total PTSD CAPS scores. First, participants were categorized as high/low in each symptom cluster, using the median CAPS cluster score as the cut-off point. Next, a series of 3 repeated-measures three-way ANCOVAs was conducted, with baseline (CA1) levels of avoidance/intrusion/hyper-arousal (alternately), treatment type and time as the independent variables (IVs), total CAPS score as the dependent variable (DV), and gender as the covariate. No significant three-way interaction was found intrusion (F(1,102)=0.358, P=.55), avoidance (F(1,102)=3.83, P=.053) and hyper-arousal (F(1,102)=0.07, P=.79), thus indicating that PE and CT had no differential effect on total PTSD score as a function of baseline levels of neither of the specific symptom clusters.
Cluster difference score between time 1 and 2
Next, we set out to examine whether the reduction in a specific PTSD symptom cluster plays a significant role in the overall reduction in PTSD scores. To examine this question, we first created 3 new variables, referring to the difference (Δ) in avoidance/intrusion/hyper-arousal scores between time 1 and time 2. This new variable signifies the magnitude of change in each cluster following treatment. Next, we conducted a series of 3 two-way ANCOVAs, with time and treatment type as the IVs, avoidance/intrusion/hyper-arousal (alternately) as the DVs, and both gender and the difference (Δ) score as covariates. The aim of this examination was to see whether controlling for the reduction in a specific symptom cluster would differentially weaken the effects of either PE or CT on total PTSD CAPS scores, thus yielding a significant Time X Treatment interaction (Moldovan & Pintea, 2015; Reeder et al., 2006). Our analyses showed that no such interaction was found, even when controlling for avoidance (F(1, 103)=1.220, p=0.272), intrusion (F(1, 103)=0.056, p=0.814) and hyper-arousal (F(1, 103)=1.514, p=.221) difference scores.
DISCUSSION
As previously reported (Shalev et al., 2012), exposure-based therapy and cognitive-elaboration based therapy in this study were associated with significant and similar reductions in PTSD symptoms. This work further explores the possibility of a differential effect of each interventions on specific PTSD symptoms as per the interventions' theoretical background and technical implementation. For that purpose, we first examined each symptom cluster as a separate outcome, and then assessed the moderating effect of baseline levels of each symptom cluster on the total reduction in PTSD symptoms. Lastly, we examined the contribution of symptom reduction in each cluster to the interventions’ effect on total PTSD score.
Contrary to expectations, PE and CT did not have a differential effect on specific PTSD symptom clusters. PE and CT similarly reduced the severity of PTSD symptoms among participants with either high or low baseline levels of intrusion, avoidance and hyperarousal. PE and CT also similarly reduced PTSD total symptom severity after controlling for their effect on each symptom cluster. Taken together, these findings seem to suggest that exposure- and non-exposure-based therapies do not necessarily affect different subsets of PTSD symptoms.
In line with a recent study (Cloitre et al., 2016), our findings show that baseline symptoms alone may not be good enough moderators of treatment response in PTSD. Thus, attempting to decide between PE and CT based on one's specific initial clinical PTSD picture may not be sufficient, and other factors, which have perhaps yet to be explored, should be considered.
Although our analyses did not directly examine mediating variables in the pure sense of the term (i.e., within or between therapy sessions), our findings indirectly suggest that a reduction in a specific PTSD cluster does not uniquely account for the reduction in PTSD total symptom score in either CT or PE. Thus, no specific cluster by itself had played a role as a major “engine” driving change in the severity of PTSD as a whole.
One possible explanation for our results is that the shared targets of these two treatments outweigh their differences. For example, while CT may not directly target avoidance as PE does, it may do so indirectly by targeting dysfunctional cognitions (Foa, 2000), which, in turn, often provoke avoidant behavior. Similarly, exposure therapy often allows one to confront intrusive thoughts that were hitherto avoided. In addition, in this study we have assessed individuals at the relatively early stages post-trauma. Evidence exists, for example, that CT may be superior to PE in the long- but not short-term following trauma (e.g. Tarrier & Sommerfield, 2004). Finally, both interventions may address underlying common dimensions of both avoidance and cognitive distortion, such as guilt, shame, or hopelessness (e.g. Gallagher & Resick, 2012).
The absence of a differential effect of CT and PE also echoes previous studies showing that PTSD clusters often align with each other over time and may increase/decrease as one “block” (Solomon, Horesh, & Ein-Dor, 2009). This notion is also in line with Horowitz’s (1976) conceptualization, according to which intrusion and avoidance symptoms represent two inter-related facets of post-traumatic reactions.
Recent studies have challenged the “one-size-fits-all” approach to trauma-focused psychotherapy (Cloitre, 2015; Steenkamp & Litz, 2014), arguing that trauma-exposed populations are heterogeneous and may differ in their therapy preferences, symptom profile and other clinical features (e.g., tolerance to intervention-embedded stress). Our finding that PE and CT work just the same given different baseline symptom profiles offers clinicians more freedom to choose between exposure- and non-exposure therapies, while expecting similar overall outcome.
Our study is limited by the sample of civilian survivors of single, short traumatic events, and the assessment of ER patients with possible physical injury. Also, more assessment points are needed to more accurately assess mediating variables that may be associated with change. Nonetheless, strengths include a large sample size and excellent protocol adherence.
Our finding that PE and CT have equivalent effects on PTSD symptom clusters should lead to treatment studies focusing on core components of PTSD and other stress disorders, to achieve improved therapeutic accuracy. In addition, and as noted earlier, our study design may not have accurately explored mechanisms of change underlying treatment effects. Future studies should include within-intervention measurements to further explore interventions’ putative mechanisms of change. Ultimately more research is needed in order to fine-tune existing psychotherapies and develop client–specific novel interventions (Cloitre, 2015).
Practitioner Points.
Despite their different theoretical backgrounds and techniques, the notion that PE and CT (without exposure) target different PTSD symptoms was not confirmed in this study. Thus, both interventions may in fact be equally effective for treating intrusion, avoidance and hyper-arousal symptoms.
Baseline levels of avoidance, intrusion and hyper-arousal may not be good a-priori indicators for PTSD treatment selection.
The effect of PE and CT on PTSD as a whole does not seem to depend on a reduction in any specific symptom cluster.
These findings indicate that exposure and non-exposure interventions may lead to similar results in terms of reductions in specific PTSD symptoms. It is quite possible that individual PTSD clusters may respond to therapy in an inter-related fashion, with one cluster affecting the other.
Acknowledgments
We would like to acknowledge the contribution of the following members of the Jerusalem Trauma Outreach and Prevention Study: Yael Ankri, M.A.; Rhonda Addesky, Ph.D.; Yossi Israeli – Shalev, M.A.; Moran Gilad, M.A; Pablo Roitman M.D.
Funding/Support:
This work was supported by a generous contribution from the Jerry Lee Foundation in Philadelphia, Pennsylvania, a service development grant from the Jewish Federation of New York, research grant MH071651 from the National Institute of Mental Health, and an investigator-initiated research grant from Lundbeck Pharmaceuticals Ltd (Denmark).
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders - 4th Edition, Text Revised (DSM-TR) Washington, DC: Author; 2013. [Google Scholar]
- Antoni MH, Lechner S, Diaz A, Vargas S, Holley H, Phillips K, Blomberg B. Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain, Behavior, and Immunity. 2009;23(5):580–591. doi: 10.1016/j.bbi.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: systematic review and meta-analysis. British Journal of Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. http://dx.doi.org/10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. http://dx.doi.org/10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM. Acute Stress Disorder Scale: a self-report measure of acute stress disorder. Psychological Assessment. 2000;12(1):61–68. http://dx.doi.org/10.1037//1040-3590.12.1.61. [PubMed] [Google Scholar]
- Cloitre M. The “one size fits all” approach to trauma treatment: should we be satisfied? European journal of psychotraumatology. 2015;6 doi: 10.3402/ejpt.v6.27344. http://dx.doi.org/10.3402/ejpt.v6.27344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Petkova E, Su Z, Weiss B. Patient characteristics as a moderator of post-traumatic stress disorder treatment outcome: combining symptom burden and strengths. British Journal of Psychiatry Open. 2016;2(2):101–106. doi: 10.1192/bjpo.bp.115.000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Ehlers A, Steil R. Maintenance of intrusive memories in posttraumatic stress disorder: a cognitive approach. Behavioral and Cognitive Psychotherapy. 1995;23:217–249. doi: 10.1017/S135246580001585X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB. Psychosocial treatment of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2000;61(5):43–48. [PubMed] [Google Scholar]
- Foa EB. Psychosocial Treatment of Posttraumatic Stress Disorder. Journal of Clinical Psychiatry. 2006;67(2):40–45. [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99(1):20–35. http://dx.doi.org/10.1037//0033-2909.99.1.20. [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd. New York: Guilford Press; 2009. [Google Scholar]
- Gallagher MW, Resick PA. Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: Preliminary evidence for the differential effects of hopelessness and habituation. Cognitive Therapy and Research. 2012;36:750–755. doi: 10.1007/s10608-011-9423-6. http://dx.doi.org/10.1007/s10608-011-9423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hembree EA, Foa EB, Dancu CV. Prolonged Exposure (PE) Manual, Revised Version. Philadelphia, PA: University of Pennsylvania; 1999. [Google Scholar]
- Horowitz MJ. Stress Response Syndromes. New York: Jason Aronson; 1976. [Google Scholar]
- Ironson G, Freund B, Strauss JL, Williams J. Comparison of two treatments for traumatic stress: A community-based study of EMDR and prolonged exposure. Journal of clinical psychology. 2002;58(1):113–128. doi: 10.1002/jclp.1132. http://dx.doi.org/10.1002/jclp.1132. [DOI] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of post traumatic stress disorder by exposure and/or cognitive restructuring. Archives of General Psychiatry. 1998;55:317–325. doi: 10.1001/archpsyc.55.4.317. http://dx.doi.org/10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- Moldovan R, Pintea S. Mechanisms of Change in Psychotherapy: Methodological and Statistical Considerations. Cognitie, Creier, Comportament/Cognition, Brain, Behavior. 2015;19(4):299. [Google Scholar]
- Paunovic N, Öst LG. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy. 2001;39(10):1183–1197. doi: 10.1016/s0005-7967(00)00093-0. http://dx.doi.org/10.1016/S0005-7967(00)00093-0. [DOI] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30(6):635–641. doi: 10.1016/j.cpr.2010.04.007. http://dx.doi.org/10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Rauch SAM, Eftekhari A, Ruzek JI. Review of exposure therapy: A gold standard for PTSD treatment. Journal of Rehabilitation Research and Development. 2012;49(5):679–688. doi: 10.1682/jrrd.2011.08.0152. http://dx.doi.org/10.1682/JRRD.2011.08.0152. [DOI] [PubMed] [Google Scholar]
- Reeder C, Smedley N, Butt K, Bogner D, Wykes T. Cognitive predictors of social functioning improvements following cognitive remediation for schizophrenia. Schizophrenia bulletin. 2006;32(suppl 1):S123–S131. doi: 10.1093/schbul/sbl019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Meadows EA, Resick P, Foy DW. Cognitive-behavioral therapy. In: Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York: Guilford; 2000. [Google Scholar]
- Shalev AY, Ankri Y, Israeli-Shalev Y, Peleg T, Adessky R, Freedman S. Prevention of posttraumatic stress disorder by early treatment: results from the Jerusalem Trauma Outreach and Prevention Study. Archives of general psychiatry. 2012;69(2):166. doi: 10.1001/archgenpsychiatry.2011.127. http://dx.doi.org/10.1001/archgenpsychiatry.2011.127. [DOI] [PubMed] [Google Scholar]
- Solomon Z, Horesh D, Ein-Dor T. The longitudinal course of posttraumatic stress disorder symptom clusters among war veterans. Journal of Clinical Psychiatry. 2009;70(6):837–843. doi: 10.4088/jcp.08m04347. http://dx.doi.org/10.4088/JCP.08m04347. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT. One-size-fits-all approach to PTSD in the VA not supported by the evidence. American Psychologist. 2014;69(7):706–707. doi: 10.1037/a0037360. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C. Treatment of chronic PTSD by cognitive therapy and exposure: 5-year follow-up. Behavior Therapy. 2004;35(2):231–246. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67(1):13–18. doi: 10.1037//0022-006x.67.1.13. http://dx.doi.org/10.1037//0022-006X.67.1.13. [DOI] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology. 2003;71(2):330–337. doi: 10.1037/0022-006x.71.2.330. http://dx.doi.org/10.1037/0022-006X.71.2.330. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Fava M. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: implications for clinical practice. American Journal of Psychiatry. 2006;163(1):28–40. doi: 10.1176/appi.ajp.163.1.28. doi/pdf/10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]