Abstract
Significant progress in the field of nursing has contributed to the widening of range of functions and professional duties of nurses. More frequent lack of nursing personnel has an impact on negative reception of work, it decreases sense of professional satisfaction and increases the level of burden and fatigue. Methods. The study applied the non-experimental method – a descriptive comparative study without a control group. The data was collected on the basis of Polish-language version of a Japanese questionnaire. In order to evaluate the level of physical fatigue the pedometer was used. Results.158 respondents of a group of 160 were included in the statistical analysis. The study group was internally diversified. The research project assessed the usefulness of the multifactorial analysis in evaluating the main components of nursing fatigue. Multifactorial analysis has shown that mental fatigue concentrated with changes in activeness, motivation and physical fatigue are strongly correlated with age, professional experience and education. Conclusion. Nursing is a profession of a special character and mission. Regardless of the place of work, nursing staff should be given the possibility of pursuing their profession under conditions ensuring the sense of security and protecting them from harmful effects on health.
Keywords: Multifactorial analysis, Workload, Fatigue, Anaesthesiology, Intensive care unit, Nursing
1. Introduction
Significant increase in demand for beds in recovery units, post operative and intensive care units has long been observed, both in European countries and in the United States of America [1,2]. It has a connection not only with demographic changes of a society, but also with a substantial progress of diagnostic and therapeutic methods that leads to the prolongation of patient’s life [3,4]. Obviously, doctors play crucial role in the treatment and this is unquestionable. Nursing staff, however, provides the majority of care at the bedside [1]. Its shortage, together with an evident need of an intensified nursing care, may intensify fatigue and workload among this occupational group.
The explanation of the term “workload” is not easy because of many definitions. Each of them includes various characteristic qualities of workload. On the basis of the analyses that concern nursing staff’s workload, O’Breien–Pallas and Baumann suggested that each research method is appropriate when it considers features, such as patient’s condition, number of nursing interventions, or level of nursing care requirements [5]. Fagerstrom and co-authors were of the opinion that in time of nursing personnel’s workload measurement, the number of human resources should be taken into consideration [6]. Significant physical and psychological burden, that results in chronic level of fatigue, is frequently present in nurses’ daily work [7-9]. Current observations show that prolonged level of fatigue is the main factor which leads to the development of depression, decline in employee satisfaction, deterioration in quality of services provided and increase in absence [10]. Fatigue is also the main factor that affects the number of medical errors and accidents at work [11-13].
This research takes into consideration the serious problem of workload and fatigue among nursing personnel. Current scientific studies discuss this issue only to a small extent, especially in the context of anaesthetic or intensive care units. Tarnow – Mordi and co-authors found that risk-adjusted mortality rates were markedly higher in patients exposed to periods of high ICU workloads [14]. The research has also confirmed the connection between strain and the occurrence of Work-Related Musculo-Skeletal Disorder (WRMSD) [15]. The analysis of the level of workload in physical and psychological aspect is crucial considering worldwide shortage of nursing staff. According to recent studies, the number of nurses entering health care system is disproportionate to the number of these who leave the system. What is more, the number of nurses over the age of 45 rises every year [16].
The aims of the study was to: 1) study the usefulness of multifactorial analysis in evaluating the main variable of nursing fatigue 2) estimate the neurophysiological symptoms of fatigue in the anaesthetic and intensive care unit. So far, the research has extended and systematized the knowledge of factors that influence nurses’ workload in anaesthetic and intensive care units. These factors in a direct or indirect way might determine the level of fatigue and affect the efficiency and quality of actions taken.
2. Materials and methods
The study was conducted upon the approval of the study protocol by the Independent Bioethics Committee for Scientific Research of the Medical University of Gdansk, approval number NKBNE/45/2009. The study project was multicenter and it took over a year to collect data. The study was questionnaire-based. It used a questionnaire collecting demographic data of authorial interviewer design and the Polish version of the Japanese questionnaire (Yoshitake questionnaire) [17]. The questionnaire helps to calculate the percentage and point value of a physical and psychological fatigue on the basis of the subjective symptoms of fatigue. The scale includes thirty grouped positions of symptoms which are divided into three groups, 10 symptoms in each. Group A-concerns the decrease in the level of activity (drowsiness), group B-symptoms of weaken motivation (concentration problems), group C-symptoms of physical fatigue (pain, numbness) [17,18]. The Polish version of the Japanese questionnaire for the first time was used by Professor Ryszard Paluch from Wroclaw University of Technology [18]. The author gave his consent to use questionnaire in the study. The questionnaire was prepared in two identical versions for both groups of nurses. The questionnaire was filled during the 12-hour shift (day shift or night shift). Respondents were asked to answer all the questions once and to not change their answers. The questionnaire ended when the researcher, after respondent’s work, noted his/her distance traveled, number of steps and the value of the energy and calorie expenditure.
In order to evaluate the level of physical fatigue, the pedometer was used. The pedometer is a simple device that counts the number of steps, the distance and the value of energy and calorie expenditure [19]. The pedometer that was used in this research is designed to record the energy expenditure which is connected with the physical effort. The research with pedometer was performed in accordance with Welton’s study design [20].
The study included nurses from anaesthetic and intensive care units (n=160) in Poland, in the Pomerania and Warmia-Mazuria Provinces. The study was performed at the Medical University of Gdańsk Clinic of Anesthesiology and Intensive Therapy. 7 out of 10 hospitals took part in the research and granted their permission. Two hospitals from Warmia and Mazuria Provinece and one from Pemerania region did, not wat to participate in the study. The respondents were informed that the study was anonymous and the data collected would be used exclusively for scientific research. Participation in the study was voluntary.
3. Statistical analysis
The variables studied in the survey were summarized with frequency counts and percentages. The significance of differences between the two groups (unrelated variables model) was examined by means of significance tests: Student’s t-test or, for homogeneity of variation – Mann-Whitney U test. Associations among variables were evaluated using chi-square test (using Yates’ correction if necessary). In order to study how independent variables influence dependent variables, factor analysis was used. Kaiser test was performed to choose main components.
All the statistical calculations were performed using statistical package StatSoft, Inc. (2011) STATISTICA version 10.0 www.statsoft.com and Excel spreadsheet. The assumed significance level in all the calculations was p<0.05. p-value was calculated in Statistica statistical package.
4. Results
160 nurses from seven other hospitals took part in the research (Figure 1).158 correctly completed questionnaires were received. The group was internally diversified in terms of age, level of education, seniority and workplace. 65 people from the group (41,14%) worked in anaesthetic units and 93 people (58,86%) worked in intensive care units. Women were the largest group both, in anaesthetic and in intensive care units. The age of subjects was 24 to over 41.People at the age of over 41 were the biggest group in anaesthetic and intensive care units. The average seniority of anaesthetic nurses is 20,8 (SD ±8,3). The average seniority of nurses in intensive care units is 15,3 (SD ±8,3). Detailed summary of socio-demographic data is illustrated with Table 1 and Figure 2.
Figure 1.
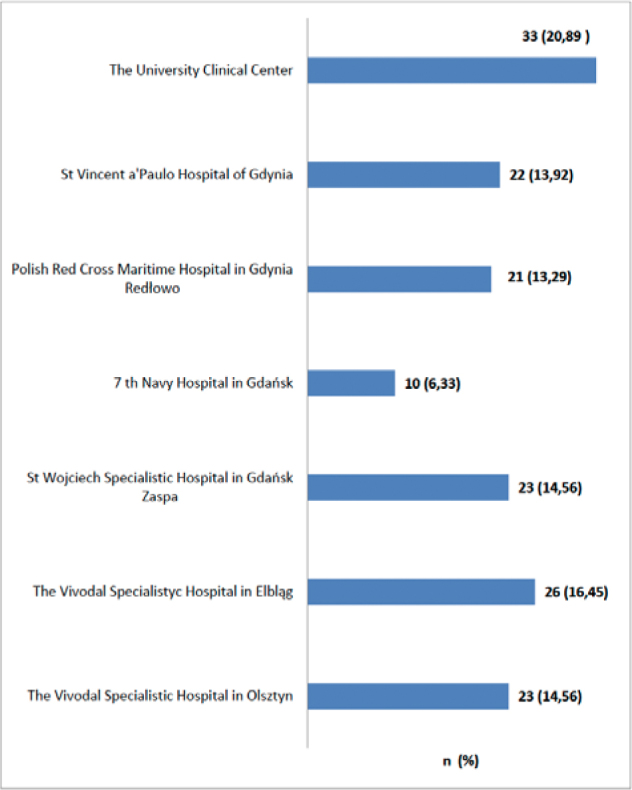
The centres participating in the study (n=158).
Table 1.
Socio-demographic characteristics of the nursing staff in anaesthesiology and intensive care units – sex, place of living, education, type of duty (n=158).
| Variable | Anaesthesiology | ICU | p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | |||||
| K | 59 | 90,77 | 91 | 97,85 | 0,103‡ |
| M | 6 | 9,23 | 2 | 2,15 | |
| Age | |||||
| 24-30 | 3 | 4,62 | 17 | 18,28 | |
| 31-35 | 8 | 12,31 | 24 | 25,81 | 0,0017*† |
| 36-40 | 18 | 27,69 | 24 | 25,81 | |
| >41 | 36 | 55,38 | 28 | 30,10 | |
| Place of living city | |||||
| >200 000 citizens | 38 | 58,46 | 36 | 38,71 | 0,0706* |
| 50 000-200 000 citizens | 20 | 30,77 | 36 | 38,71 | |
| 50 000 citizens | 2 | 3,08 | 8 | 8,60 | |
| village | 5 | 7,69 | 13 | 13,98 | |
| Education | |||||
| medical secondary school | 24 | 36,92 | 42 | 45,16 | |
| post-secondary school of nursing | 15 | 23,08 | 21 | 22,58 | 0,684* |
| bachelor’s degree nursing college | 14 | 21,54 | 18 | 19,35 | |
| master’s degree nursing college | 12 | 18,46 | 12 | 12,90 | |
| Supplementary course | |||||
| none | 58 | 89,23 | 78 | 83,87 | |
| qualification course in anaesthesiology and intensive care | 2 | 3,08 | 8 | 8,60 | 0,2062* |
| specialization in anaesthesiology and intensive care | 3 | 4,61 | 1 | 1,07 | |
| other | 2 | 3,08 | 6 | 6,46 | |
| Type of duty | |||||
| 12 hour day shift | 41 | 63,08 | 58 | 62,37 | 0,927* |
| 12 hour night shift | 24 | 36,92 | 35 | 37,68 | |
Source.Q 1-3 of the survey questionnaire (part one).
test chi-square with Yates correction
chi-square (x 2 ) test, significance level p<0.05
significance of differences between the study groups
chi-square (x 2 ) test, significance level p<0.05
chi-square (x 2 ) test, significance level p<0.05
chi-square (x 2 ) test, significance level p<0.05
chi-square (x 2 ) test, significance level p<0.05
Figure 2.
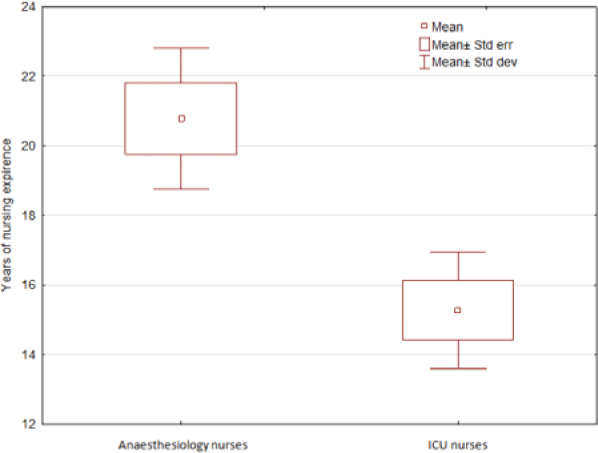
Professional experience of nurses in anaesthesiology and intensive care wards. Frame table – whiskers.
Source: Q. 5 of the survey questionnaire (part one).
*t-Student test, significance level of p<0.05., † significance of differences between the study groups.
Neurophysiological analysis of fatigue symptoms at a lower level, activity, decrease in the level of motivation and physical symptoms of fatigue has revealed statistically significant differences between the groups of subjects in answering the statement “My head feels heavy” (p=0,0378) and “I feel back pain” (p=0,0220) (Table 2).
Table 2.
The neurophysiologic fatigue symptoms (n=158).
| Items | Anesthesiology | ICU | p | |||
|---|---|---|---|---|---|---|
| n | n | % | n | % | ||
| A 1 I would like to lie down | 1 | 25 | 38,46 | 21 | 22,58 | |
| 2 | 21 | 32,31 | 38 | 40,86 | ||
| 3 | 4 | 6?15 | 4 | 4,30 | 0,2283 | |
| 4 | 9 | 13,85 | 20 | 21,51 | ||
| 5 | 6 | 9,23 | 10 | 10,75 | ||
| A 2. I feel sleepy | 1 | 11 | 16,92 | 17 | 18,28 | |
| 2 | 29 | 44,62 | 39 | 41,93 | ||
| 3 | 1 | 1,54 | 2 | 2,15 | 0,9764 | |
| 4 | 18 | 27,69 | 24 | 25,81 | ||
| 5 | 6 | 9,23 | 11 | 11,83 | ||
| A 3. I feel dizzy | 1 | 2 | 3,08 | 3 | 3,22 | |
| 2 | 2 | 3,08 | 11 | 11,83 | ||
| 3 | 4 | 6,15 | 2 | 2,15 | 0,1355 | |
| 4 | 24 | 36,92 | 24 | 25,81 | ||
| 5 | 33 | 50,77 | 53 | 56,99 | ||
| A 4. My eyes are tired | 1 | 19 | 29,23 | 28 | 30,11 | |
| 2 | 28 | 43,08 | 42 | 45,16 | 0,9869 | |
| 3 | 1 | 1,54 | 2 | 2,15 | ||
| 4 | 11 | 16,92 | 14 | 15,05 | ||
| 5 | 6 | 9,23 | 7 | 7,53 | ||
| A 5. I feel languid | 1 | 7 | 10,78 | 20 | 21,50 | |
| 2 | 33 | 50,77 | 36 | 38,71 | ||
| 3 | 4 | 6,15 | 1 | 1,08 | 0,1136 | |
| 4 | 17 | 26,15 | 30 | 32,26 | ||
| 5 | 4 | 6,15 | 6 | 6,45 | ||
| A 6. My legs are tired | 1 | 22 | 33,84 | 40 | 43,01 | |
| 2 | 27 | 41,54 | 31 | 33,33 | 0,1496 | |
| 3 | 3 | 4,62 | 0 | 0,0 | ||
| 4 | 12 | 18,46 | 18 | 19,36 | ||
| 5 | 1 | 1,54 | 4 | 4,30 | ||
| A 7. My movements are clumsy | 1 | 0 | 0,0 | 3 | 3,23 | |
| 2 | 7 | 10,77 | 15 | 16,12 | ||
| 3 | 6 | 9,23 | 5 | 5,38 | 0,3917 | |
| 4 | 38 | 58,46 | 48 | 51,61 | ||
| 5 | 14 | 21,54 | 22 | 23,66 | ||
| A 8. My whole body feels tired | 1 | 6 | 9,23 | 16 | 17,20 | |
| 2 | 25 | 38,46 | 36 | 38,71 | ||
| 3 | 2 | 3,08 | 6 | 6,45 | 0,2191 | |
| 4 | 28 | 43,08 | 26 | 27,96 | ||
| 5 | 4 | 6,15 | 9 | 9,68 | ||
| A 9. My head feels heavy | 1 | 1 | 1,54 | 12 | 12,90 | |
| 2 | 25 | 38,46 | 26 | 27,96 | ||
| 3 | 7 | 10,77 | 4 | 4,30 | 0,0378*† | |
| 4 | 22 | 33,85 | 38 | 40,6 | ||
| 5 | 10 | 15,38 | 13 | 13,98 | ||
| A 10. I yawn | 1 | 12 | 18,46 | 14 | 15,05 | |
| 2 | 15 | 23,08 | 30 | 32,26 | ||
| 3 | 5 | 7,69 | 1 | 1,08 | 0,2131 | |
| 4 | 22 | 33,85 | 32 | 34,41 | ||
| 5 | 11 | 16,92 | 16 | 17,20 | ||
| B 1.I am impatient | 1 | 4 | 6,15 | 6 | 6,45 | |
| 2 | 10 | 15,38 | 19 | 20,43 | 0,6397 | |
| 3 | 12 | 18,46 | 11 | 11,83 | ||
| 4 | 30 | 46,16 | 39 | 41,94 | ||
| 5 | 9 | 13,85 | 18 | 19,35 | ||
| B 2. I am undecided | 1 | 0 | 0,0 | 1 | 1,08 | |
| 2 | 4 | 6,15 | 9 | 9,68 | 0,5965 | |
| 3 | 4 | 6,15 | 10 | 10,75 | ||
| 4 | 38 | 58,46 | 46 | 49,46 | ||
| 5 | 19 | 29,24 | 27 | 29,03 | ||
| B 3. I cannot concentrate | 1 | 0 | 0,0 | 2 | 2,15 | |
| 2 | 11 | 16,92 | 18 | 19,36 | 0,6086 | |
| 3 | 2 | 3,08 | 6 | 6,45 | ||
| 4 | 31 | 47,69 | 40 | 43,01 | ||
| 5 | 21 | 32,31 | 27 | 29,03 | ||
| B 4. I feel indifferent | 1 | 2 | 3,08 | 3 | 3,22 | |
| 2 | 2 | 3,08 | 11 | 11,83 | ||
| 3 | 2 | 3,08 | 9 | 9,68 | 0,1312 | |
| 4 | 35 | 53,84 | 42 | 45,16 | ||
| 5 | 24 | 36,92 | 28 | 30,11 | ||
| B 5. I find it difficult to gather my thoughts | 1 | 1 | 1,54 | 2 | 2,15 | |
| 2 | 9 | 13,85 | 15 | 16,13 | 0,7200 | |
| 3 | 1 | 1,54 | 3 | 3,22 | ||
| 4 | 34 | 52,31 | 53 | 56,99 | ||
| 5 | 20 | 30,76 | 20 | 21,51 | ||
| B 6. I feel absent-minded | 1 | 0 | 0,0 | 2 | 2,15 | |
| 2 | 12 | 18,46 | 15 | 16,13 | ||
| 3 | 6 | 9,23 | 5 | 5,38 | 0,6105 | |
| 4 | 32 | 49,23 | 45 | 48,39 | ||
| 5 | 15 | 23,08 | 26 | 27,95 | ||
| B 7. My attention is distractec | 1 | 0 | 0,0 | 1 | 1,08 | |
| 2 | 14 | 21,54 | 21 | 22,58 | ||
| 3 | 2 | 3,08 | 5 | 5,38 | 0,8131 | |
| 4 | 35 | 53,84 | 44 | 47,31 | ||
| 5 | 14 | 21,54 | 22 | 23,65 | ||
| B 8. I feel anxious | 1 | 1 | 1,54 | 1 | 1,08 | |
| 2 | 8 | 12,31 | 11 | 11,82 | ||
| 3 | 6 | 9,23 | 1 | 1,08 | 0,1643 | |
| 4 | 30 | 46,15 | 44 | 47,32 | ||
| 5 | 20 | 30,77 | 36 | 38,70 | ||
| B 9. I get tired of speaking | 1 | 2 | 3,08 | 2 | 2,15 | |
| 2 | 13 | 20,0 | 15 | 16,13 | ||
| 3 | 8 | 12,31 | 5 | 5,38 | 0,4879 | |
| 4 | 25 | 38,46 | 43 | 46,24 | ||
| 5 | 17 | 26,15 | 28 | 30,10 | ||
| B 10. I am annoyed | 1 | 2 | 3,08 | 1 | 1,08 | |
| 2 | 15 | 23,08 | 22 | 23,65 | ||
| 3 | 6 | 9,23 | 2 | 2,15 | 0,2774 | |
| 4 | 26 | 40,0 | 40 | 43,01 | ||
| 5 | 16 | 24,61 | 28 | 30,11 | ||
| C 1. My shoulders are stiff | 1 | 3 | 4,62 | 10 | 10,75 | |
| 2 | 14 | 21,54 | 33 | 35,48 | ||
| 3 | 6 | 9,23 | 5 | 5,38 | 0,0788 | |
| 4 | 32 | 49,23 | 29 | 31,18 | ||
| 5 | 10 | 15,38 | 16 | 17,21 | ||
| C 2. I breathe quickly | 1 | 1 | 1,54 | 1 | 1,08 | |
| 2 | 5 | 7,69 | 9 | 9,68 | ||
| 3 | 6 | 9,23 | 2 | 2,15 | 0,3845 | |
| 4 | 34 | 52,31 | 52 | 55,91 | ||
| 5 | 19 | 29,23 | 29 | 31,18 | ||
| C 3.I have a headache | 1 | 2 | 3,08 | 10 | 10,75 | |
| 2 | 17 | 26,15 | 18 | 19,36 | 0,4110 | |
| 3 | 3 | 4,62 | 3 | 3,23 | ||
| 4 | 23 | 35,38 | 33 | 35,48 | ||
| 5 | 20 | 30,77 | 29 | 31,18 | ||
| C 4. My voice becomes hoars | e 1 | 2 | 3,08 | 4 | 4,30 | |
| 2 | 12 | 18,46 | 18 | 19,35 | ||
| 3 | 4 | 6,15 | 1 | 1,08 | 0,4421 | |
| 4 | 29 | 44,62 | 39 | 41,94 | ||
| 5 | 18 | 27,69 | 31 | 33,33 | ||
| C 5. I am thirsty | 1 | 25 | 38,46 | 37 | 39,78 | |
| 2 | 27 | 41,54 | 37 | 39,78 | ||
| 3 | 1 | 1,54 | 3 | 3,23 | 0,4605 | |
| 4 | 6 | 9,23 | 13 | 13,98 | ||
| 5 | 6 | 9,23 | 3 | 3,23 | ||
| C 6. My limbs feel shaky | 1 | 4 | 6,15 | 5 | 5,38 | |
| 2 | 7 | 10,77 | 10 | 10,75 | 0,9622 | |
| 3 | 3 | 4,62 | 6 | 6,45 | ||
| 4 | 31 | 47,69 | 40 | 43,01 | ||
| 5 | 20 | 30,77 | 32 | 34,41 | ||
| C 7. Sounds annoy me | 1 | 4 | 6,15 | 6 | 6,45 | |
| 2 | 21 | 32,31 | 29 | 31,18 | ||
| 3 | 4 | 6,15 | 6 | 6,45 | 0,9857 | |
| 4 | 25 | 38,46 | 39 | 41,94 | ||
| 5 | 11 | 16,93 | 13 | 13,98 | ||
| C 8. I am apathetic | 1 | 2 | 3,08 | 3 | 3,23 | |
| 2 | 15 | 23,08 | 21 | 22,58 | 0,9056 | |
| 3 | 7 | 10,77 | 6 | 6,45 | ||
| 4 | 28 | 43,07 | 44 | 47,31 | ||
| 5 | 13 | 20,0 | 19 | 20,43 | ||
| C 9. I feel pain in my back | 1 | 10 | 15,38 | 31 | 33,33 | |
| 2 | 29 | 44,62 | 35 | 37,64 | 0,0220*† | |
| 3 | 2 | 3,08 | 1 | 1,08 | ||
| 4 | 18 | 27,69 | 12 | 12,90 | ||
| 5 | 6 | 9,23 | 14 | 15,05 | ||
| C 10. My nerves are really tense | 1 | 6 | 9,23 | 11 | 11,83 | |
| 2 | 13 | 20,0 | 17 | 18,28 | 0,9219 | |
| 3 | 10 | 15,38 | 11 | 11,83 | ||
| 4 | 23 | 35,39 | 37 | 39,78 | ||
| 5 | 13 | 20,0 | 17 | 18,28 | ||
**answers on average 5-point Likert scale. A specific number of points was assigned to each answer: definitely not – 0; rather not – 1; no opinion – 2; rather yes – 3; definitely yes – 4.
chi-square (x2) test, significance level p < 0.05
significance of differences between the study groups
chi-square (x2) test, significance level p < 0.05
significance of differences between the study groups
In order to improve understanding of the interaction and relationships between particular variables of fatigue, factor analysis which reduces the set of variables was used in further analysis. Five main components were identified during the analysis. They explain the total variance of all questions in accordance with Kaiser test criterion and have eigenvalues bigger than 1 (Table 3). The first component explains 36,76% of total variance, the second 24,50%, the third 17,13%, the fourth 16,15% and the last 5,44%. Scree test (Figure 3) allowed to include three main components, which are below breakdown point, in further descriptive analyses (statistics). The data obtained that way were used to continue the analysis. Factor loadings of main components visibly divide the scale into three categories: symptoms typical for the feeling of tiredness that is connected with the activity and motivation decline (the first component), symptoms of physical fatigue (the second component), impaired concentration (the third component). Taking into account the degree of correlation of particular variables, it turns out that the first component (symptoms of tiredness connected with the activity and motivation decline) correlates 15 questions and has values from 0,607 to 0,891 on the scale. 9 variables correlate with the next component (symptoms of physical fatigue). Their loadings are from -0,936 to 0,606. 7 variables (0,755 do -0,604) has the strongest correlation with the third component (impaired concentration) (Table 4).
Table 3.
The principal component analysis.
| Value | Eigenvalues | % of Variance | Cumulative % |
|---|---|---|---|
| 1 | 9,927023 | 36,76675 | 36,7668 |
| 2 | 6,616100 | 24,50407 | 61,2708 |
| 3 | 4,625366 | 17,13098 | 78,4018 |
| 4 | 4,360702 | 16,15075 | 94,5526 |
| 5 | 1,470809 | 5,44744 | 100,0000 |
Figure 3.
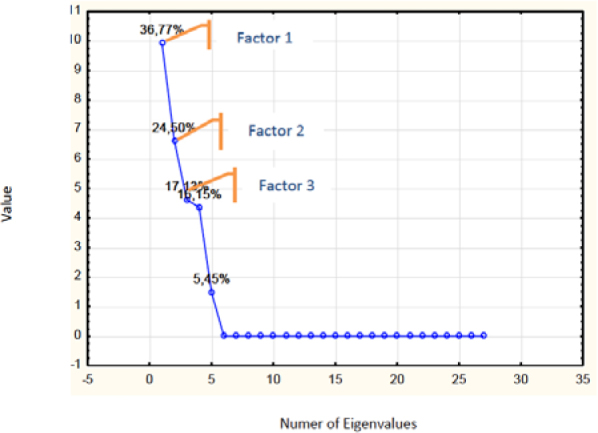
Factorial scree plot.
Table 4.
Results of principal components factor analysis with varimax rotation.
| Variable | Factor loadings | ||||
|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | |
| A1 | 0,891751 | 0,020745 | −0,384732 | 0,018132 | −0,236650 |
| A2 | 0,723738 | −0,009214 | −0,397587 | 0,490624 | −0,278085 |
| A3 | 0,168857 | −0,496668 | 0,668648 | −0,517047 | −0,101883 |
| A4 | 0,607115 | −0,376399 | 0,104855 | −0,075183 | −0,687814 |
| A5 | 0,312413 | −0,936373 | 0,090547 | −0,113560 | −0,067150 |
| A6 | 0,153607 | −0,823234 | −0,326526 | 0,317712 | 0,301879 |
| A7 | 0,854494 | −0,346828 | 0,327371 | −0,201554 | −0,041879 |
| A8 | 0,684952 | −0,288470 | −0,538856 | −0,391112 | 0,065512 |
| A9 | 0,343710 | −0,904490 | 0,149395 | 0,092191 | 0,181505 |
| A10 | 0,747901 | −0,302947 | 0,094019 | −0,074111 | 0,578391 |
| B1 | 0,822108 | 0,033605 | 0,550529 | 0,141159 | −0,001373 |
| B2 | 0,598216 | 0,053739 | 0,755337 | 0,251998 | 0,072200 |
| B3 | 0,673184 | 0,056414 | 0,688418 | 0,152793 | −0,215352 |
| B4 | 0,689030 | 0,408486 | 0,384818 | 0,409724 | 0,205956 |
| B5 | 0,535558 | −0,406032 | −0,673429 | 0,307343 | 0,018704 |
| B6 | 0,535558 | −0,406032 | −0,673429 | 0,307343 | 0,018704 |
| B7 | 0,559399 | 0,087290 | −0,621029 | −0,520493 | 0,151205 |
| B8 | 0,476087 | 0,410395 | −0,006184 | −0,775968 | 0,052462 |
| B9 | 0,487556 | −0,851102 | −0,021670 | 0,123747 | −0,148771 |
| B10 | 0,748375 | 0,026390 | 0,562679 | 0,217180 | 0,274705 |
| Energy expenditure | 0,685992 | 0,675619 | −0,135798 | 0,232329 | −0,023186 |
| Numer of steps | 0,700962 | 0,596598 | −0,216154 | 0,295324 | −0,137053 |
| Distance traveled (km) | 0,695162 | 0,634186 | −0,181039 | 0,260031 | −0,119021 |
| *Age | 0,656665 | 0,606907 | −0,412739 | −0,064737 | −0,160966 |
| *Education | −0,510297 | −0,856992 | −0,061821 | 0,036230 | 0,005170 |
| *Professional experience | 0,747588 | 0,533485 | −0,361003 | −0,149751 | 0,061291 |
| *Place of living | −0,573677 | −0,366930 | −0,604463 | −0,411857 | −0,035438 |
| *Type of shift | −0,491105 | −0,832532 | 0,032442 | 0,254270 | −0,000739 |
The pedometer tests indicated that the average distance traveled during the day shift, among the anaesthetic personnel, was 5,5 km (SD ± 2,3). When it comes to the nurses from the intensive care units, the distance was 4,9 km (SD± 2,9). Table 5 illustrates detailed summary of the data.
Table 5.
Comparison of day vs night shift (energy expenditure, number of steps, distance traveled).
| Anaesthesiology nurses | ICU nurses | p-value | |||
|---|---|---|---|---|---|
| day shift | night shift | day shift | night shift | ||
| Energy expenditure (kcal) | |||||
| Mean±SD | 328,8±135,1 | 147,2±89,4 | 294,9±136,2 | 187,5±103,6 | 10,0001*† |
| Median | 297,01 | 136,51 | 287,52 | 156,02 | 20,0004*† |
| Distance traveled (km) | |||||
| Mean±SD | 5,5±2,3 | 2,5±1,5 | 4,9±2,1 | 3,2±1,6 | 10,0001*† |
| Median | 5,01 | 2,41 | 5,02 | 2,82 | 20,0003*† |
U Mann-Whitney test, significance level p<0.05
significance of differences between the study groups
U Mann-Whitney test, significance level p<0.05
significance of differences between the study groups
U Mann-Whitney test, significance level p<0.05
significance of differences between the study groups
U Mann-Whitney test, significance level p<0.05
significance of differences between the study groups
5. Discussion
Among anesthesiology nurses, persons over 41 years old were the most numerous, followed by those aged 36-40. The nursing staff aged 24-30 was in the minority. At the intensive care units too employees over 41 years old were in the majority. The number of nurses in the next two age ranges was the same. Similarly to the anesthesiology units, the least persons belonged to the 24-30 year-olds’ group. These results demonstrate that nurses belong to a group of ageing professions. The results obtained are consistent with epidemiological data on the age and sex structure of nurses in Poland and in the world [16,21,22].
The most numerous group of nurses at the anesthesiology and intensive care units had secondary-level education. Relatively few of the respondents reported having a higher education bachelor’s or master’s degree. A small percentage of the nursing staff at the units studied reported having completed supplementary training in the form of qualification courses and specialization courses in anesthesiology and intensive therapy. This number is relatively small considering the regulations of the Minister of Health of 20 December 2012 on the standard of medical procedures in anesthesiology and intensive therapy for entities engaged in health care activities [23]. The regulation stipulates that nursing staff working in the department of anesthesiology and intensive care ought to complete the course or specialization in the field of anesthesiology and intensive care.Our own study also demonstrated that the anesthesiology unit employees had a much greater length of service than those of the intensive care unit.
It is not easy to compare the results of this research with other authors, results because of a small number of scientific publications. Most authors, who studied the problem of fatigue among nursing staff, used shortened or incomplete versions of Yoshitake questionnaire [24,25]. The present study used the complete Polish-language version of the Japanese questionnaire. The Japanese questionnaire was first prepared in 1967 for the Research Committee of the Japanese Industrial Society [17,28]. The Polish-language version of the questionnaire was used in studies of fatigue among nursing personnel [26] teachers, primary school pupils and industry workers.
This research revealed typical symptoms of physical fatigue and fatigue in aspects of activity and motivation. Among estimated symptoms, statistically important difference between the personnel in the anaesthetic and intensive care units concerned the answer to the statement “My head feels heavy” and “I feel back pain”. The differences between the groups may result from various working conditions in both units. So far, the results of studies that concern work environment and its factors that influence anaesthetic and intensive care units employees’ state of health, seem to be incomplete.The studies that elaborated on operating theatres work environment pay attention to the problem of environmental pollution of operating theatres. This pollution is caused by general anaesthetics and undoubtedly affects the state of health [27]. Studies that concern intensive care units focus on nursing staff duties and the risk of physical, chemical and ergonomic factors [28,29].
The analysis of main components indicated three major factors of fatigue. The study shows positive correlation between the subscale of activity and motivation decline and the subscale of seniority, age and distance. Another correlation was indicated between the subscale of physical fatigue and the subscale of age, education, the type of duty and distance.Current studies that focus on the issue of nurses’ fatigue have confirmed the correlation between the level of fatigue, seniority and education of nursing staff [30]. According to Barker and co-authors, nurses’ higher education (vocational, bachelor or master degree) correlates with the increase of feeling tired [31]. Similar correlation was indicated in relation to seniority. Winwood and co-authors [32] showed that more experienced nurses feel less tired. Better accommodative ability results from the change of expectations and the increased level of professional responsibility. Nurses with bigger work experience adapt to changing working conditions much faster. They also easier deal with stress [32,33]. Right after graduation or after the first year of employment, nursing personnel, as a rule, feels higher level of fatigue. According to the researchers, it is connected with the lack of work experience and adaptation to a new work environment [32,34,35]. The research also showed the relation between physical symptoms of fatigue and the type of shift. The results of the research are close to the results of other authors who deal with measuring fatigue among employees who work shifts. Youan S.C. et al. found that nurses who work shifts were more fatigued than nurses who work during the day [36].Other research found a significant positive association between insomnia, excessive sleepiness, excessive fatigue and shift work disorder [37].
A limitation of this research work was definitely the selection of the study group. The applied method involved neither random selection nor a control group. The choice of the study group and location was intentional and it was made on the basis of the results of studies published in Critical Care Nurse [38] .The results of the present study confirm the complexity of the problem of workload, especially in the assessment of fatigue. This study presents the respondents’ subjective opinions expressed in the form of assessment of the level of activity, motivation and physical symptoms, without a possibility of objective control. Opinions on the use of subjective methods of assessment of fatigue level are still inconclusive. Some authors question their credibility, whereas others think that the use of subjective methods for the evaluation of the fatigue level is justified [24,40-42].
Our evaluation of the fatigue rate did not take into account such indirect factors as the respondent’s emotional condition, professional satisfaction, family life, additional employment and monotony in the work environment [43-44]. The existing results of studies indicate that these factors are not insignificant, hence it is necessary to perform further in-depth analyses.
6. Conclusion
The results of the study indicated that: multifactorial analysis may be useful in measuring and interpreting the right components of nursing fatigue. Research showed that mental fatigue concerned with changes in activeness, motivation and physical fatigue are strongly correlated with age, professional experience and education of nurses. The study proved that physical fatigue in the anaesthetic and intensive care unit is highly related to the type of shift, which may increase the level of fatigue.
Nursing is a profession of a special character and mission. Regardless of the workplace, nursing staff should be given the possibility of pursuing their profession under conditions ensuring the sense of security and protecting them from harmful effects on health. In Poland for the last few months there has been an open discussion about the implementation of the minimum nurse patient ratio into Polish regulations. This legislation would force medical centers to check whether the hospitals have an adequate number of staff at the various wards. Although previous studies using NEMS and NAS scale gave the recommendation regarding the number of nurses per patient at the ICU ward - in practice this is not always observed. Lack of regulation creates room for interpretation. The problem is not insignificant and the latest research showed that workload and fatigue is the main barrier in pain management in the postoperative ward [45].
Acknowledgements
The authors wish to thank: Mrs. Agnieszce Mlynarczykowskiej, Mrs Magdalenie Szafranek and all the nurses for their co-operation in the study process.
Footnotes
Conflicts of interest: The authors declare no conflict of interest.
References
- [1].Adhikari N.K., Fowler R., Bhagwanjee S., Rubenfeld G.. Critical care and the global burden of critical illness in adults. Lancet. 2010;376:1339–1346. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rhodes A., Ferdinande P., Flaatten H., Guidet B., Metnitz P.G., Moreno R.P.. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- [3].Straker L., Mathiassen S.E.. Increased physical work loads in modern work – A necessity of better health and performance? Ergonomics. 2009;52:1215–1225. doi: 10.1080/00140130903039101. [DOI] [PubMed] [Google Scholar]
- [4].Alameddine M., Dainty K.N., Deber R., Sibbald W.. The intensive care unit work environment: Current challenges and recommendations for the future. J Crit Care. 2009;24:243–248. doi: 10.1016/j.jcrc.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].O’Brien-Pallas L., Baumann A.. Toward evidence-based policy decisions: a case study of nursing health human resources in Ontario, Canada. Nursing Inquiry. 2000;7:248–257. [Google Scholar]
- [6].Fagerström L, Rainio A-K, Rauhala A., Nojonen K.. Professional assessment of optimal nursing care intensity level. Scand J of Caring Sciences. 2000;14:97–104. [PubMed] [Google Scholar]
- [7].Wisner A.. Fatigue and human reliability revisited in the light of ergonomics and work psychopathology. Ergonomics. 1989;32:891–898. doi: 10.1080/00140138908966851. [DOI] [PubMed] [Google Scholar]
- [8].Trinkoff A.M, Lipscomb J.A, Geiger-Brown J., Storr C.L., Brady B.A.. Perceived physical demands and reported musculoskeletal problems in registered nurses. Am J Prev Med. 2003;24:270–275. doi: 10.1016/s0749-3797(02)00639-6. [DOI] [PubMed] [Google Scholar]
- [9].Jaworek M., Marek T., Karwowski W., Andrzejczak Ch., Genaidy A.M.. Burnout syndrome as a mediator for the effect of work-related factors on musculoskeletal complaints among hospital nurses. Int J of Industrial Ergonomics. 2010;40:368–375. [Google Scholar]
- [10].van Dijk F.J.H, Swaen G.M.H.. Fatigue at work. Occup Environ Med. 2003;60:I1–I2. doi: 10.1136/oem.60.suppl_1.i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lamberg L.. Long hours little, sleep. Bad medicine for physicians-in-training? JAMA. 2002;287:303–307. doi: 10.1001/jama.287.3.303. [DOI] [PubMed] [Google Scholar]
- [12].Carayon P., Gurses A.P.. A human factors engineering conceptual framework of nursing workload and patients safety in intensive care units. Intensive and Crit Care Nurs. 2005;21:284–301. doi: 10.1016/j.iccn.2004.12.003. [DOI] [PubMed] [Google Scholar]
- [13].Dorrian J., Tolley C., Lamnond N.. et al. Sleep and errors in a group of Australian hospital nurses at work and during the commute. Appl Ergon. 2008;39:605–613. doi: 10.1016/j.apergo.2008.01.012. [DOI] [PubMed] [Google Scholar]
- [14].Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356:185–189. doi: 10.1016/s0140-6736(00)02478-8. [DOI] [PubMed] [Google Scholar]
- [15].Eatough E.M., Way J.D., Chang C.-H.. Understanding the link between psychosocial work stressors and work-related musculoskeletal complaints. Appl Ergon. 2012;43:554–563. doi: 10.1016/j.apergo.2011.08.009. [DOI] [PubMed] [Google Scholar]
- [16].Simones S., Villeneuve M., Hurst J.. OECD Health Working Papers No.19 Tackling Nurse Shortage in OECD Countries. DELSA/ELSA/WD/HEA(2005)1. 2013 http://www.oecd.org/health/health-systems/34571365.pdf [Google Scholar]
- [17].Yoshitake H.. Three characteristic patterns of subjective fatigue symptoms. Ergonomics. 1978;21:231–233. doi: 10.1080/00140137808931718. [DOI] [PubMed] [Google Scholar]
- [18].Paluch R.. Fatigue evaluation based on subjective perception – the Japanese questionnaire. Bezpieczenstwo Pracy. 1985;7-8:3–6. in Polish. [Google Scholar]
- [19].Turner L.J., Huchen L., Williams J.. Reliability of pedometers to measure step counts in patients with chronic respiratory disease. Journal of Cardiopulmonary Rehabilitation and Prevention. 2012;32:284–291. doi: 10.1097/HCR.0b013e31825c49f2. [DOI] [PubMed] [Google Scholar]
- [20].Welton J., Decker M., Adam J., Zone-Smith L.. How far do nurses walk? Medical-surgical Nurses. 2006;15:213–216. [PubMed] [Google Scholar]
- [21].Camerino D., Conway P.M., van der Heiden B.I.. et al. Low-perceived work ability, ageing and intention to leave nursing: a comparison among 10 European countries. Journal of Advanced Nursing. 2006;56:542–552. doi: 10.1111/j.1365-2648.2006.04046.x. [DOI] [PubMed] [Google Scholar]
- [22].Chief Council of Nurses and Midwives. Preliminary assessment of human resources of nurses and midwives in Poland until 2020. 2010 http://www.izbapiel.org.pl/upload/Wstepna.ocena.zasobow.kadrowych.pdf [Google Scholar]
- [23].Regulation of the Minister of Health of 20 December 2012 on the standards of medical proceedings in anesthesiology and intensive care for health care entities. 2013 http://www.mz.gov.pl/wwwfiles/ma_struktura/docs/anestezjolog_20121221_rozpo.pdf [Google Scholar]
- [24].Barker L.M., Pasupathy K.S.. Identification of relationships between work system parameters and fatigue in registered nurses: a data mining approach. Proceedings of the Human Factors and Ergonomics Society. 54 th Annual Meeting September 2010:364–368. [Google Scholar]
- [25].Szczurak T., Kaminska B., Szpak A.. Estimation of the psychological load in the performance of nurses’ work based on subjective fatique symptoms. Adv Med Sciences. 2007;52:102–104. [PubMed] [Google Scholar]
- [26].Zysnarska M., Bernad D., Maksymiuk M., Adamek R., Kara I.. Specific elements of nurse overload. Family Medicine and Primary Care Review. 2008;10:1351–1355. [Google Scholar]
- [27].Downes J., Rauk PN., Vanheest AE.. Occupational hazards for pregnant or lactating women in the orthopaedic operating room. Journal of the American Academy of Orthopaedic Surgeons. 2014;22:326–332. doi: 10.5435/JAAOS-22-05-326. [DOI] [PubMed] [Google Scholar]
- [28].Mphil A.M., Cert G., Chaboyer W.. et al. Understanding the work of intensive care nurses: A time and motion study. Australian Crit Care. 2012;25:13–22. doi: 10.1016/j.aucc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- [29].Lee SJ, Faucett J, Gillen M, Krause N, Landry L.. Risk perception of musculoskeletal injury among critical care nurses. Nurs Research. 2013;62:36–44. doi: 10.1097/NNR.0b013e31827334d6. [DOI] [PubMed] [Google Scholar]
- [30].Hart S, Staveland L.. Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. Adv Psychology. 1988;52:139–183. [Google Scholar]
- [31].Barker L.M., Pasupathy K.S.. Identification of relationships between work system parameters and fatigue in registered nurses: a data mining approach. Proceedings of the Human Factors and Ergonomics Society. 54 th Annual Meeting September 2010:364–368. [Google Scholar]
- [32].Winwood P.C., Winefield A.H., Lushington K.. Work-related fatigue and recovery: the contribution of age, domestic responsibilities and shiftwork. J Adv Nurs. 2006;56:438–449. doi: 10.1111/j.1365-2648.2006.04011.x. [DOI] [PubMed] [Google Scholar]
- [33].Winwood P.C., Lushington K., Winefield A.H.. Further development and validation of the Occupational Fatigue Exhaustion Recovery (OFER) scale. J Occu Environ Med. 2006;48:381–389. doi: 10.1097/01.jom.0000194164.14081.06. [DOI] [PubMed] [Google Scholar]
- [34].Mc Neese-Smith D.K.. Job stages of entry, mastery, and disengagement among nurses. J Nurs Adm. 2000;30:140–147. doi: 10.1097/00005110-200003000-00006. [DOI] [PubMed] [Google Scholar]
- [35].Mc Neese-Smith D.K., van Servellen G.. Age, developmental, and job stage influences on nurse outcomes. Outcomes Management in Nursing Practice. 2000;4:97–104. [PubMed] [Google Scholar]
- [36].Yuan SC., Chou MC., Chen CJ., Lin YJ., Chen MC., Liu HH., Kuo HW.. Influences of shift work on fatigue among nurses. J Nurs Management. 2011;19:339–345. doi: 10.1111/j.1365-2834.2010.01173.x. [DOI] [PubMed] [Google Scholar]
- [37].Eldevik MF., Flo E., Moen BE., Pallesen S., Bjorvatn B.. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS ONE. doi: 10.1371/journal.pone.0070882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Schmalenberg C., Kramer M.. Clinical units with the healthiest work environments. Crit Care Nurs. 2008;28:65–77. [PubMed] [Google Scholar]
- [39].Barker L.M., Nussbaum M.A.. Fatigue, performance and the work environment: a survey of registered nurses. J Adv Nurs. 2011;1370;67 doi: 10.1111/j.1365-2648.2010.05597.x. [DOI] [PubMed] [Google Scholar]
- [40].Paluch R.. Ocena zmęczenia na podstawie subiektywnego odczucia-kwestionariusz japoński. Bezp Pracy. 1985;7-8:3–6. in Polish. [Google Scholar]
- [41].Babbie E.. Podstawy badań spotecznych. Wyd. PWN. Warszawa. 2008;196-198:287–288. in Polish. [Google Scholar]
- [42].Szczurak T., Kamińska B., Szpak A.. Estimation of the psychological load in the performance of nurses’ work based on subjective fatique symptoms. Advances in Medical Sciences. 2007;52:102–104. in Polish. [PubMed] [Google Scholar]
- [43].Winwood P.C., Winefield A.H., Lushington K.. Work-related fatigue and recovery: the contribution of age, domestic responsibilities and shiftwork. J Adv Nurs. 2006;56:438–449. doi: 10.1111/j.1365-2648.2006.04011.x. [DOI] [PubMed] [Google Scholar]
- [44].Ward-Griffin C, St-Amantr O, Brown JB.. [online] Compassion fatigue within double duty caregiving: nurse-daughters caring for elderly parents. Online J Issues Nurs. 2011;31:16–4. doi: 10.3912/OJIN.Vol16No01Man04. [DOI] [PubMed] [Google Scholar]
- [45].Mędrzycka-Dąbrowska W., Dąbrowski S., Basiński A., Pilch D.. Perception of barriers to postoperative pain management in elderly patients in Polish hospitals with and without a “Hospital Without Pain” Certificate – a multi-center study. Arch Med Sci. 2016;4:808–818. doi: 10.5114/aoms.2015.54768. [DOI] [PMC free article] [PubMed] [Google Scholar]


