Abstract
This study examines dissociation and posttraumatic symptomatology in a sample of maltreated preschool-age children in foster care. Analyses compared Child Behavior Checklist subscale scores for the foster care sample and a community sample, and also examined differences between maltreatment subtypes. Exposure to any type of maltreatment was associated with greater dissociation and posttraumatic symptomatology in this sample. Preschool-age children with documented sexual abuse displayed high levels of posttraumatic symptoms, whereas children with documented physical abuse tended to use dissociation as a primary coping mechanism. The finding that physically abused children had high levels of dissociation confirms previous research with preschoolers.
Keywords: dissociation, PTSD, maltreatment, child abuse, preschoolers
Repeated childhood abuse has been extensively documented as resulting in serious long-term psychological effects, including the development of dissociation and posttraumatic stress disorder (PTSD; Briere, 1992; Freyd, 1996; Hornstein, 1993; Liotti, 1999; Putnam, 1997; Terr, 1991). However, there have been few studies of traumatic sequelae in early childhood. It is essential to consider how trauma may impact functioning at an early age to better target pathology with appropriate prevention and intervention strategies. The study of child maltreatment should thus be considered from a developmental psychopathology perspective, which emphasizes a transactional interplay between developmental challenges and trajectories, causal mechanisms, risk and protective factors, and ecological influences (Cicchetti & Lynch, 1993). Because pathology results from sequential deviations from a normal trajectory, early childhood is a particularly important period to study due to the possibility of cascading developmental problems.
Briere (1992) described dissociation as “a defensive disruption in the normally occurring connections among feelings, thoughts, behavior, and memories…invoked in order to reduce psychological distress” (p. 34). Dissociation is often conceptualized as a coping mechanism, enabling the child to deal with the distress of maltreatment. However, dissociation may be considered pathological when it has a negative impact on functioning and well-being in other areas of the individual’s life. Abuse survivors often exhibit abrupt, maladaptive changes in mannerisms, access to knowledge, and age-appropriate behavior (Putnam, 1997). High levels of dissociation in childhood appear to result in problems negotiating developmental challenges and are frequently comorbid with other psychopathological symptomatology (Putnam).
According to Putnam (1997), there are three major categories of dissociation: behavior automatization, affect/information compartmentalization, and identity alteration. Behavior automatization allows for the “redirection of conscious awareness away from a repetitive or procedural activity” (Putnam, p. 68). Within the context of experiencing trauma, behavior automatization appears to allow the child to push the repeated acts of disturbing, painful, and/or distressing abuse out of conscious awareness. Affect/information compartmentalization involves the separation of awareness from memory through which emotionally charged information is stored separately from other types of information (Putnam). According to Freyd’s (1996) betrayal trauma theory, a child blocks the knowledge and pain of abuse by a caregiver through the process of isolating explicit knowledge of trauma away from awareness. By “forgetting” the abuse, the child can protect the relationship to the parent. Lastly, identity alteration may be manifested in several ways. Depersonalization, for example, is the feeling of being detached from oneself and one’s thoughts, or not being able to remember certain aspects of one’s identity (Putnam). Dissociative identity disorder (DID), formerly known as multiple personality disorder (MPD), is another more extreme form of identity alteration.
Posttraumatic stress disorder symptomatology is also found in maltreated children (Pfefferbaum, 1997). Widom (1999) estimated that one-third of individuals who experienced child maltreatment meet criteria for lifetime PTSD. There are three main symptom clusters of PTSD: intrusion, hyperarousal, and avoidance (American Psychiatric Association [APA], 2000). Intrusion symptoms include recurrent nightmares/flashbacks or distress toward cues that are reminders of the traumatic event. Signs of hyperarousal may be manifested as sleep difficulties, increased vigilance/anxiety, or irritability. Finally, the individual with PTSD demonstrates avoidance of triggers that may precipitate a memory of the traumatic event (APA). Avoidance may seem to be conceptually similar to dissociation; however, it does not encompass the full nature of disturbances that occur to the integrated systems of consciousness, memory, identity, and perception (APA). Although the main focus of the current study is on dissociation, it will also examine PTSD symptomatology.
Dissociation in Childhood
Research on adult samples has shown a strong link between childhood maltreatment by a caregiver and the experience of pathological dissociation. Chu and Dill (1990) found that childhood abuse was related to high levels of dissociation in adulthood as measured by the Dissociative Experiences Scale (DES; Bernstein & Putnam, 1986). In particular, subjects abused by family members had significantly higher scores on the DES, suggesting that betrayal may have a central component in the development of dissociation. Chu and Dill also found main effects for physical and sexual abuse but not neglect, indicating that the experience of abuse itself is associated with greater dissociation. Scores on the DES were highest for those who reported a combination of physical and sexual abuse. However, it is important to note that the literature shows mixed results as to whether certain types of maltreatment are related to dissociation and which subtypes are more predictive of dissociation. Although many studies have demonstrated a relationship between sexual abuse and later dissociation, the association between physical abuse and later dissociation is less clear due to inconsistent findings (e.g., Briere & Runtz, 1988; Coons, 1996; Hornstein & Putnam, 1992; Irwin, 1994; Kirby, Chu, & Dill, 1993; Sanders & Giolas, 1991; Waldinger, Swett, Frank, & Miller, 1994; Zlotnick et al., 1996).
Much of the research on maltreatment and dissociation is retrospective in nature, examining dissociation levels in adulthood among individuals who report having experienced childhood maltreatment. One tool for assessing dissociation in children is the Child Dissociative Checklist (CDC; Putnam, Helmers, & Trickett, 1993), which is a 20-item caregiver-report measure. There is a range of items on the CDC that represent different types of dissociative symptoms. Putnam et al. examined the reliability and validity of the CDC in a study of girls aged 7–15. The authors compared scores across four different conditions: maltreated girls diagnosed with Multiple Personality Disorder (MPD; now known as Dissociative Identity Disorder), maltreated girls diagnosed with Dissociative Disorder Not Otherwise Specified (DDNOS), girls with a documented history of only sexual abuse and no diagnosis of a mental health disorder, and a control group. They found that the CDC measured dissociation along a continuum of severity, as scores ranged from very high levels in the MPD group (M = 25), followed by the DDNOS group (M = 16.5), the sexually abused group (M = 6), and the control group (M = 2.3). The authors note that similar patterns have been found using the DES in adult samples, indicating consistency between measures (Putnam et al.).
There have been few prospective studies of dissociation with preschool-age children, despite indications that it has profound effects in early childhood. Indeed, many adults with dissociative disorders describe onset at this time (Hornstein, 1993). There are a number of challenges to assessing pathological dissociation in young children. Preschoolers typically have higher levels of normative dissociation as compared to other age groups (Putnam, 1997). For example, they may enter a trance-like state when distressed; this is likely due to a lag in cognitive development, as they do not yet have the capability to use other defense mechanisms (Hornstein). In addition, preschoolers are more apt to incorporate fantasy into their daily lives. Assessing dissociation in preschoolers must therefore incorporate the context of age-appropriate behavior, taking into account how frequent, pervasive, and/or disabling the symptoms are (Hornstein).
Macfie, Cicchetti, and Toth (2001a) measured dissociation in preschool-age children with an innovative developmentally appropriate paradigm. Using dolls and other props, they elicited narratives from children by presenting story stems about stressful family situations. The children’s behaviors, affect, and language were coded for dissociative symptomatology. Macfie and colleagues found that maltreated children, particularly those who had been physically or sexually abused, showed more dissociation than nonmaltreated children. Indeed, maltreated children showed a significant increase in dissociation levels over a one-year period, illustrating the importance of detecting dissociation at an early age.
Ogawa, Sroufe, Weinfeld, Carlson, and Egeland (1997) also examined the impact of maltreatment on dissociation over time. Using prospective, longitudinal data from a sample of at-risk children, they found that maltreatment predicted dissociation at all developmental stages, from toddlerhood to adulthood. Adolescents who had been classified with a disorganized attachment in infancy and also experienced childhood trauma had the highest mean dissociation score compared with any other classification type. In addition, chronicity, severity, and age of onset of the childhood trauma were all significantly associated with dissociation. Children who experienced trauma in infancy tended to experience more chronic and severe trauma compared with participants who experienced trauma later in life; these individuals had high dissociation levels at all time points measured in the study. Significant predictors of dissociation during the toddler/preschool period in particular included prior experiences of physical abuse or neglect during infancy, and concurrent sexual abuse (Ogawa et al.).
Macfie, Cicchetti, and Toth (2001b) further considered the effect of maltreatment subtype on dissociation in preschool-age children. As has been demonstrated in other studies, they found that children who had experienced sexual abuse, physical abuse, or neglect had significantly higher dissociation levels than children who were neither abused nor neglected, and that severity and chronicity of maltreatment were both significantly associated with dissociation (Macfie et al.). Of the different maltreatment subtypes, physical abuse was the only form that was significantly associated with scoring in the clinical range on the Child Dissociative Checklist. This is quite noteworthy, as dissociation is commonly thought to be associated with sexual abuse (e.g., Kisiel & Lyons, 2001), while PTSD has been associated with both physical and sexual abuse (e.g., Widom, 1999). Taken together, the findings by Macfie et al. and Ogawa et al. (1997) indicate that dissociation may be a developmentally appropriate response to the experience of physical abuse in early childhood. In addition, their findings underscore the importance of examining not only maltreatment subtypes but also such factors as severity and chronicity.
Measuring Dissociation and PTSD Using Child Behavior Checklist (CBCL) Subscales
A number of recent studies have assessed dissociation as well as PTSD in children using scales derived from the Child Behavior Checklist (CBCL; Achenbach, 1991). This is an important development in that the CBCL is a widely used behavior assessment tool and the use of such scales could expand the number of studies of traumatic sequelae in children. However, it is important to acknowledge that the CBCL was not designed to measure dissociation or PTSD. Many of the symptoms associated with these types of pathology are difficult to observe and report. Nevertheless, these scales may be useful to professionals for screening or research purposes. All of the following scales can be found in Table 1 and are described in more detail in the Method section.
Table 1.
Items from Previously Published Subscales
| Malinosky-Rummel and Hoier (1992) |
| Dissociation |
| 1. Acts too young for his/her age |
| 5. Behaves like opposite sex |
| 8. Can’t concentrate, can’t pay attention for long |
| 13. Confused/Seems to be in a fog |
| 17. Daydreams or gets lost in thoughts |
| 80. Stares blankly |
| 87. Sudden changes in mood or feelings |
| Ogawa et al. (1997) |
| Dissociation |
| 1. Acts too young for his/her age |
| 8. Can’t concentrate, can’t pay attention for long |
| 13. Confused/Seems to be in a fog |
| 17. Daydreams or gets lost in thoughts |
| 18. Deliberately harms self or attempts suicide |
| 36. Gets hurt a lot, accident-prone. |
| 40. Hears sounds/voices that aren’t there |
| 80. Stares blankly |
| 87. Sudden changes in mood or feelings |
| 91. Talks about killing self |
| Sim et al. (2005) |
| Dissociation |
| 13. Confused/Seems to be in a fog |
| 17. Daydreams or gets lost in thoughts |
| 80. Stares blankly |
| PTSD |
| 9. Can’t get mind off certain thoughts |
| 29. Fears certain animals, situations, places |
| 45. Nervous/high-strung/tense |
| 47. Nightmares |
| 50. Too fearful or anxious |
| 76. Sleeps less than other children |
| 100. Trouble sleeping |
| PTSD/Dissociation |
| 8. Can’t concentrate, can’t pay attention for long |
| 9. Can’t get mind off certain thoughts |
| 13. Confused/Seems to be in a fog |
| 17. Daydreams or gets lost in thoughts |
| 29. Fears certain animals, situations, places |
| 40. Hears sounds/voices that aren’t there |
| 45. Nervous/high-strung/tense |
| 47. Nightmares |
| 50. Too fearful or anxious |
| 66. Repeats certain acts over and over |
| 76. Sleeps less than other children |
| 80. Stares blankly |
| 84. Strange behavior |
| 87. Sudden changes in mood or feelings |
| 92. Talks or walks in sleep |
| 100. Trouble sleeping |
Malinosky-Rummel developed a six-item subscale for the CBCL whose content corresponds to items from the CDC (Malinosky-Rummel & Hoier, 1991). The subscale was originally used to measure dissociation in a sample of 7- to 12-year-olds. Although Malinosky-Rummel and Hoier determined that the CBCL subscale has adequate item generalizability, they did not use it to distinguish between maltreated and nonmaltreated groups in their study.
Ogawa et al. (1997) created a Dissociation subscale using a similar method. They chose items from the CBCL and the CBCL Teacher Report Form that correspond with CDC items. The subscale was used in the study described above, to measure dissociation during infancy, preschool, elementary school, adolescence, and young adulthood.
Lastly, Sim et al. (2005) published a 7-item PTSD subscale, a 3-item Dissociation subscale, and a 16-item PTSD/Dissociation subscale that contains items from the PTSD and Dissociation subscales and several other items. These subscales were created using CBCL item ratings by 16 clinical child psychology experts from across the country. Sim et al. used these subscales to examine dissociation and PTSD in a sample of 4- to 12-year-olds, comparing normative, psychiatric, and sexually abused samples. Analyses showed that the psychiatric and sexually abused groups had significantly higher levels of dissociation and PTSD than the normative sample, although the subscales did not distinguish between these clinical samples (Sim et al.).
Although the CBCL subscales developed by these three research groups are not identical, it may be possible to develop a set of coherent, empirically based factors from them. In addition, none of the subscales have yet been used with a preschool population; therefore, it is important to determine whether they can adequately assess these constructs in early childhood.
Current Study
The main focus of the current study was to examine dissociation in a population of maltreated preschool-age children. Because CDC data were unavailable, we estimated dissociation levels using the CBCL. All of the CBCL subscales reviewed contain several core items (items 13, 17, 80), yet there are also items unique to each. Furthermore, the scales have different theoretical backgrounds. Sim et al. (2005) proposed a combined PTSD/Dissociation scale in addition to a Dissociation scale, suggesting that the two constructs are difficult to distinguish from one another. We were therefore interested in how best to use the information in the proposed subscales to measure dissociation and whether we could establish discriminant validity between dissociation and PTSD symptomatology.
In the first part of the study, we used an empirically grounded approach to determine the appropriate factors for assessing dissociation and posttraumatic symptomatology. All items from the CBCL subscales described above were combined. Based on the degree of relationship between these theoretical constructs, items that had high face validity for either factor (i.e., dissociation and PTSD) were modeled using confirmatory factor analysis (CFA). We expected that the CFA would confirm the existence of these two separate factors.
In the second part of the study, dissociation and PTSD levels for the sample were estimated using the two subscales that emerged from this process. We set out to determine how different types of maltreatment might impact dissociation in early childhood. Although previous researchers have examined this (e.g., Macfie et al., 2001a, 2001b), they grouped subtypes using a hierarchical system based on deviation from social norms and did not incorporate severity information. In these studies, the sexual abuse category included children who also experienced physical abuse or neglect, the physical abuse category included children who also experienced neglect, and the neglect category included children who only experienced neglect.
In the current study, we used groups that were established in prior research for this sample (Pears, Kim, & Fisher, 2006). Children were classified into groups based on the dimensions of type and mean level of maltreatment severity using latent profile analysis (LPA). The LPA was conducted to determine whether naturally occurring groups of children with similar maltreatment experiences, in terms of type and severity within type, could be identified. This approach is in contrast to other approaches that emphasize a single type of maltreatment that a child has experienced. The study identified four unique profiles in this sample of maltreated preschoolers (Pears et al.). The first group, supervisory neglect/emotional maltreatment, experienced moderate-to-high severity levels of supervisory neglect and emotional maltreatment but low levels of physical neglect (e.g., failure to provide food and medical care) and almost no physical or sexual abuse. The second group, sexual abuse/emotional maltreatment/neglect, experienced high levels of sexual abuse and emotional maltreatment, moderate levels of neglect, and almost no physical abuse. The third group, physical abuse/neglect/emotional maltreatment, experienced moderate-to-high severity levels of physical abuse in addition to neglect and emotional maltreatment but very low levels of sexual abuse. The fourth group, sexual abuse/physical abuse/emotional maltreatment/neglect, experienced all of the maltreatment types at moderate-to-high levels.
In the current study, these profiles are treated as known groups. Using the CBCL scales to measure dissociation and PTSD, we examined the following hypotheses: (a) children who had experienced any maltreatment were expected to have higher levels of dissociation than those who had not; and (b) based on the research shown by Macfie et al. (2001b), children who had experienced moderate-to-high severity physical abuse, alone or in addition to other maltreatment subtypes, would exhibit high dissociation levels. We also expected that children who had experienced all three subtypes at moderate-to-high severity levels would be more likely to have higher levels of dissociation than other subgroups due to their greater need to cope.
Method
Participants
Data for this study were collected at the Oregon Social Learning Center. The participants were 177 preschool-age children (ages 3 to 6) and their caregivers, who were part of the Multidimensional Treatment Foster Care-Preschool study (Fisher, Burraston, & Pears, 2005). Children in foster care (FC; n = 117) were randomly assigned to regular foster-care services or treatment foster-care services. There were no baseline differences between the treatment and control groups on the outcome variables of interest; therefore, the groups were combined in the current study. A group of age- and SES-matched children with no known history of maltreatment were also recruited from the community (CC; n = 60). The ethnicity of the sample is as follows: 87% European American, 6% Latino, 4% Native American, 3% African American, and 1% Asian/Pacific Islander.
The FC group was composed of children entering new foster placements who were referred to the study through the local child welfare system. This included children new to foster care, children re-entering foster care, and children being moved from a prior foster placement. Children had spent an average of 170 days in foster care before entry into the study (range=17–860 days), with an average of three prior foster placements. Families in the CC group were recruited via posted flyers at Head Start classrooms, local supermarkets, and daycare centers and via advertisements in local newspapers. CC families were accepted into the study if they fit the following criteria: the child lived consistently with at least one biological parent, household income was no more than $30,000, parental education level was less than a 4-year college degree, and there was no prior child welfare system involvement.
Assessments of behavioral, developmental, and emotional regulation outcomes for the MTFC-P study were conducted at 3-month intervals for two years. The assessments of foster care samples began three to five weeks after placement in a new foster home. Foster parents in the FC group and parents or primary caregivers in the CC group completed the CBCL every six months for two years; however, this study examines differences in dissociative symptoms at the baseline assessment only. CBCL data were missing for six FC group children and one CC group child, resulting in a total sample size of 170.
Maltreatment Coding
The maltreatment experiences of the children in the study were coded from case files using the Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993). Training in the use of the MCS was conducted by one of the MCS authors (Manly). This system codes for severity information and several different types of maltreatment, including physical abuse, sexual abuse, failure to provide, lack of supervision, emotional maltreatment, educational maltreatment, and moral-legal maltreatment.
Two coders coded the case files. To qualify as a maltreatment incident, an event had to fit the definitions of maltreatment given in the code and either be reported by a reliable reporter or be considered to be founded by the child protective services caseworker. Coders did not solely rely on the caseworker’s determination of whether an incident was founded or unfounded to give a more complete picture of the child’s history of maltreatment.
Each incident of maltreatment was coded for severity level on a scale ranging from 1 (less serious maltreatment) to 5 (severe or potentially life-threatening maltreatment). For example, for physical abuse, a score of 1 would indicate that minor marks had been left on the child’s body (but not neck or head) while a score of 5 would indicate that the caregiver had inflicted an injury on the child that required hospitalization and/or was permanently disabling or disfiguring. Incidents were also coded for the type of perpetrators involved in the incident and the type of maltreatment that they had inflicted upon the child. Children who did not experience a particular type of maltreatment received a score of 0 for that category.
Preliminary analyses indicated that the base rates for moral-legal maltreatment and educational maltreatment (because the children were below school age) were extremely low. These two categories were therefore dropped from further score calculation and analyses. For each child, a total mean severity score for each category of maltreatment was calculated. All of the individual incidents were summed for a total number of incidents of maltreatment score. Finally, for each child the number of different types of maltreatment that the child experienced was computed.
During data collection, 20% of the files were double-coded to compute interrater reliability. Agreement on the identification of incidents was high (80%), and interrater agreement was similarly high for the severity of each type of abuse. The average kappa was .72 across all of the categories, and kappas within each category were moderate to high (physical abuse κ = .82; sexual abuse κ = .67; failure to provide κ = .65; lack of supervision κ = .65; emotional maltreatment κ = .79).
In the current study, we used maltreatment subgroups that had been established by subjecting the results of the MCS to LPA (Pears et al., 2006). By incorporating multiple dimensions of maltreatment simultaneously, ecologically valid maltreatment groups were distinguished, allowing for better specification of the sequelae of particular profiles of maltreatment.
Measures
Child Behavior Checklist
The CBCL is a 113-item behavior rating scale for children ages 4–18 (Achenbach, 1991). Caregivers rated their child’s behavior over the prior 6-month period on a 3-point scale ranging from 0 (not true) to 2 (very true/often true). Dissociative and PTSD symptoms were assessed using four subscales of the CBCL that have been published in the developmental psychopathology literature (see Table 1 for subscales). Subscale 1 was developed by Malinosky-Rummel (Malinosky-Rummel & Hoier, 1991) to assess dissociative symptomatology using seven CBCL items that correspond with CDC items. After running an item analysis, one item was dropped to improve the internal consistency of the scale, resulting in a 6-item scale (Malinosky-Rummel & Hoier).
Subscale 2 was developed by Ogawa et al. (1997) to assess dissociation using twelve items from the CBCL and the CBCL Teacher Report Form. The authors chose items that corresponded to the CDC, excluding those items related to inappropriate sexual behavior. In the present study, we used a 10-item version of the scale; teacher-reported data were not available because the children were not school-aged.
Subscales 3 and 4 were developed by Sim et al. (2005), who published a 7-item PTSD subscale, a 3-item Dissociation subscale, and a 16-item PTSD/Dissociation subscale. For the purposes of the present study, analyses were completed using the Dissociation sub-scale and the PTSD/Dissociation subscale. In the Sim et al. study, only subscales 3 and 4 correlated with child self-reports as measured by the Trauma Symptom Checklist. The subscales were created through a process involving item ratings by a panel of sixteen clinical child psychology experts from across the country. Items were included in subscales if at least two-thirds of experts rated the item as indicative of PTSD or dissociation. The authors also performed a CFA and examined coefficient alphas to determine reliability of the constructs. The PTSD subscale had an alpha coefficient of .74 and a CFI of .91. The Dissociation subscale had an alpha of 0.71; they were unable to calculate the CFI due to the small number of items. Finally, the combined PTSD/Dissociation subscale had an alpha of 0.85 and a CFI of 0.91. Cronbach’s alphas for the three Sim et al. subscales were between 0.74 and 0.88.
Data Analytic Strategies
Exploratory analyses showed that the four CBCL subscales were similar and that the items from each were highly intercorrelated (Cholankeril, Freyd, Becker-Blease, Pears, & Fisher, 2006). Items from the Malinosky-Rummel and Hoier Dissociation subscale, the Ogawa et al. Dissociation subscale, and the Sim et al. PTSD/Dissociation subscale were combined, and two groups of items were chosen based on face validity for either dissociation or posttraumatic symptomatology. A systematic data reduction process was applied through testing the internal consistency of these scales.
Using the scales that emerged, we performed a CFA to test model fit. By determining whether a valid factor structure exists, we planned to replicate and extend previous work to identify CBCL scales of dissociation and PTSD. The CFA is discussed in greater detail in the Results section. One-way ANOVAs were then conducted with these scales to compare the foster and community samples, and to compare dissociation and posttraumatic symptomatology across maltreatment subgroups.
Results
Scale Analyses and Model Fit
Correlational analyses were run on the four subscales, and all four were found to be significantly correlated at the 0.01 level (see Table 2). In particular, the three Dissociation subscales were the most highly correlated, with r values ranging from 0.83 to 0.97. The Combined PTSD/Dissociation subscale (Sim et al.) was less highly correlated with the other three subscales, but this was expected as it contains items assessing PTSD symptoms. Due to the level of item overlap and high correlations between subscales, we used an empirically grounded approach to determine whether coherent measures of dissociation and PTSD were obtainable from these subscales.
Table 2.
Correlations between CBCL Subscales
| Malinosky-Rummel | Ogawa et al. | Sim et al. Dissociation | Sim et al. PTSD/Diss | |
|---|---|---|---|---|
| Malinosky-Rummel | 1.0000 | |||
| Ogawa et al. | 0.9711 | 1.0000 | ||
| Sim et al. Dissociation | 0.8563 | 0.8254 | 1.0000 | |
| Sim et al. PTSD/Diss | 0.7560 | 0.7916 | 0.6192 | 1.0000 |
Note. All of the above correlations are based on listwise deletion and are significant at the 0.01 level.
Items from the Malinosky-Rummel and Hoier Dissociation subscale, the Ogawa et al. Dissociation subscale, and the Sim et al. PTSD/Dissociation subscale were combined. Reliability analysis showed that the items (n = 21) together had a Cronbach’s alpha of 0.833. Based on the empirical literature as well as our hypotheses, items were chosen that had face validity for either dissociation or PTSD symptomatology. Several items (i.e., 1, 76, and 92) were not included, as they were not considered specific to either construct. We employed a data reduction process by systematically improving the level of internal consistency as measured by Cronbach’s alpha, and two scales emerged (see Table 3). The first subscale, representing dissociation, was identical to the Sim et al. Dissociation subscale. This provided support for using this scale (α = 0.85) as a valid measure of dissociation. The second subscale, with an alpha of 0.78, contained PTSD items from primarily intrusion and hyperarousal symptom clusters.
Table 3.
Scales Based on Internal Consistency Analysis
| Standardized Beta |
Unstandardized Beta |
Critical ratio | |
|---|---|---|---|
| Dissociation component (Identical to Sim et al. (2005) Dissociation subscale; chosen from items 5, 8, 13, 17, 40, 66, & 80.) | |||
| 13. Confused/Seems to be in a fog | .778 | 1 | 0 |
| 17. Daydreams or gets lost in thoughts | .726 | 1.048 | 7.097 |
| 80. Stares blankly | .883 | 1.179 | 5.177 |
| Posttraumatic arousal/intrusion component (Chosen from items 9, 18, 29, 36, 45, 47, 50, 66, 84, 87, 91, 100.) | |||
| 9. Can’t get mind off certain thoughts | .509 | 1 | 0 |
| 18. Deliberately harms self or attempts suicide | .454 | .628 | 2.520 |
| 29. Fears certain animals, situations, places | .371 | .704 | 2.144 |
| 45. Nervous/high strung/tense | .535 | 1.143 | 3.563 |
| 47. Nightmares | .550 | 1.124 | 3.753 |
| 50. Too fearful or anxious | .589 | 1.350 | 4.027 |
| 66. Repeats certain acts over and over | .307 | 0.562 | 1.964 |
| 84. Strange behavior | .496 | 0.699 | 4.578 |
| 87. Sudden changes in mood or feelings | .515 | 1.059 | 3.642 |
| 100. Trouble sleeping | .459 | 0.968 | 2.929 |
The adequacy of the hypothesized factor structure was examined using Mplus 4.2 (Muthén & Muthén, 2004). We used full information maximum likelihood with robust standard errors (MLR) estimators to take into account the interdependence of sibling data as well as nonnormality of items. This also allowed for the inclusion of participants with partial data on dependent variables. The residual errors of three pairs of items were allowed to covary: Item 100 (Trouble sleeping) with Item 47 (Nightmares), Item 50 (Too fearful or anxious) with Item 29 (Fears certain animals, situations, places), and Item 66 (Repeats certain acts over and over) with Item 9 (Can’t get mind off of certain thoughts). These item pairs were chosen because they are likely to have common sources of variance due to similar content and high correlations. In addition, items for each pair were located on the same factor.
Standardized and unstandardized coefficients and critical ratios for the items are presented in Table 3. All thirteen items significantly loaded on the two latent factors, and the model fit the data very well: χ2(61) = 74.997, p = 0.11, CFI = 0.95, TLI = 0.93, RMSEA = 0.045, suggesting that they are adequate measures of two latent factors of traumatic symptomatology for maltreated children.
ANOVA Comparisons Using CBCL Scales
One-way ANOVAs using the Welch approximation (to account for unequal cell sizes and variances) were conducted to compare the FC and CC sample scores on the Sim et al. Dissociation subscale and the new Posttraumatic arousal/intrusion subscale (see Figure 1). Histograms and descriptive statistics for FC and CC groups were examined for equality of variance and outliers. To deal with violations of normality in the dataset, several steps were taken. First, outliers were recoded to be within two standard deviations of the mean. A natural log transformation was then performed to correct for positive skew.
Figure 1.
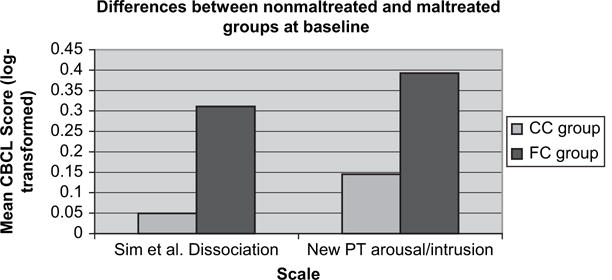
Differences between FC and CC.
Analyses showed that the FC group (M = 0.46, SD = 0.58) had a significantly higher level of dissociation than the CC group (M = 0.06, SD = 0.18), F(1, 156.97) = 48.87, p < 0.01. The FC group (M = 0.39, SD = 0.26) also showed higher levels of posttraumatic arousal/intrusion symptoms than the CC group (M = 0.21, SD = 0.14), F(1, 167.72) = 66.18, p < 0.01. Analyses on the untransformed data set indicated similar findings.
We next conducted one-way ANOVAs to compare maltreatment profiles using the CBCL subscales. Means and standard deviations are presented in Table 4 for the maltreatment profiles: sexual abuse/physical abuse/emotional maltreatment/neglect (n = 11), physical abuse/neglect/emotional maltreatment (n = 19), sexual abuse/emotional maltreatment/neglect (n=13), and supervisory neglect/emotional maltreatment (n = 68). These groups will be abbreviated as moderate–high all types, moderate–high PA, high SA, and moderate neglect in the following section.
Table 4.
Descriptive Statistics of Maltreatment Subgroups, After Log Transformation
| Subscale | Moderate–high All types |
Moderate–high PA |
High SA
|
Moderate neglect
|
||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Sim et al. Dissociation | 0.4079 | 0.4268 | 0.5383 | 0.3686 | 0.2747 | 0.3577 | 0.2300 | 0.2941 |
| New Posttraumatic arousal/intrusion | 0.4402 | 0.2033 | 0.3108 | 0.2289 | 0.5473 | 0.3159 | 0.3367 | 0.2239 |
Outliers were again recoded, and a natural log transformation was performed to correct for skew. Tests indicated homogeneity of variance between groups. ANOVAs were then performed (see Figure 2). Results indicated that groups differed significantly on the Sim et al. Dissociation subscale, F(3,107) = 4.753, p = 0.004. Tukey’s HSD test revealed that the moderate–high PA group (M = 0.54, SD = 0.37) had a significantly higher mean dissociation level than the moderate neglect group (M = 0.23, SD = 0.29), p = 0.0026. The new Posttraumatic arousal/intrusion subscale also showed a significant difference between maltreatment subgroups, F(3,107) = 3.643, p = 0.015. Tukey’s HSD test indicated that the high SA group (M = 0.44, SD = 0.2) had a significantly higher mean arousal/intrusion level than the moderate neglect group (M = 0.34, SD = 0.22), p = 0.02. Additionally, the high SA group had a significantly higher mean arousal/intrusion level than the moderate–high PA group (M = 0.31, SD = 0.23), p = 0.03. Analyses performed on the untransformed data were similar.
Figure 2.
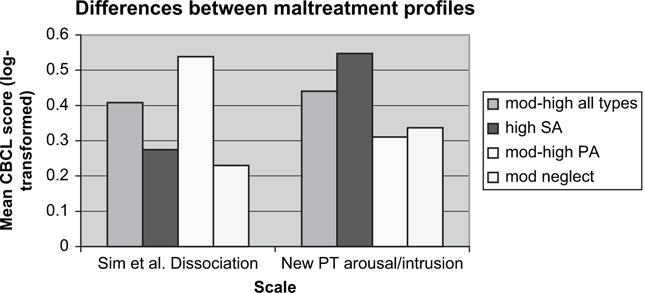
Differences between LPA groups.
Discussion
This study examined dissociation and posttraumatic arousal/intrusion in a sample of maltreated foster preschoolers and a nonmaltreated community control group. Using a systematic data reduction process, two scales emerged that measure these constructs. The CFA confirmed good model fit, providing support for the use of the Sim et al. Dissociation subscale and a new scale of posttraumatic arousal/intrusion symptoms. The process we used suggests that dissociation is a separate construct from other posttraumatic symptomatology. It is important to note that this may be due to the limitations of the CBCL, as the new scale did not contain items from the avoidance cluster of PTSD. We therefore encourage the examination of other PTSD subscales that have been proposed in the literature. Furthermore, this process may have been influenced by the characteristics of the current sample; thus, we also encourage replication and validation on future samples, keeping in mind that the CBCL may be best used as a screening rather than diagnostic tool.
Dissociation and posttraumatic arousal/intrusion levels were estimated using the two CBCL subscales. As there have been few studies of dissociation during this developmental period, one of our aims was to provide more information about dissociative phenomena in early childhood. Our analyses indicated that children in the foster care sample had significantly higher levels of dissociation as well as PTSD symptomatology, compared to a nonmaltreated community sample. Thus, it appears that exposure to any type of maltreatment is associated with greater dissociative and posttraumatic symptomatology. In terms of maltreatment profiles within the foster care sample, the new posttraumatic arousal/intrusion scale showed that the group who had experienced high severity sexual abuse had a significantly higher mean level of PTSD symptomatology than the moderate-to-high severity physical abuse group as well as the group who had primarily experienced neglect. The Sim et al. (2005) Dissociation subscale revealed a statistically significant difference in dissociation level between children who experienced moderate-to-high severity physical abuse compared with the neglect group.
One of our hypotheses was that children who had experienced all types of maltreatment at moderate-to-high severity would show the highest levels of dissociation as they might have the greatest need for a coping mechanism to block out the mental and physical distress of abuse. These children showed the second highest mean scores but did not show a statistically significant difference from other groups. Rather, the highest mean scores were found in the moderate-to-high severity physical abuse (plus neglect) group. Interestingly, these findings are consistent with previous studies of preschoolers. Macfie and colleagues (2001b), who used a hierarchical strategy to create mutually exclusive subgroups, determined that preschool children in the sexual abuse category, who may have also experienced physical abuse, did not have the highest levels of dissociation. Rather, it was the children in the physical abuse category (which included children who also experienced neglect) who had the highest levels and tended to score in the clinical range. Our study therefore replicates the findings by Macfie et al. of high dissociation among physically abused preschool aged children.
Furthermore, our research indicates that although preschool-age children who had been severely physically abused tend to use dissociation as a primary coping mechanism, children who had been sexually abused display high levels of posttraumatic arousal symptoms. This implies a distinct difference between the experiences of sexual abuse versus physical abuse during this developmental period. The literature has typically linked dissociation with the experience of sexual abuse, and while this recognition is certainly essential, our research points to the importance of also acknowledging that dissociation may be present in physically abused children, particularly during the preschool years.
It is possible that because they were removed from the situation in which they were abused, children who primarily experienced sexual abuse did not develop more seriously pathological dissociation. The maltreated children in our study were placed in foster care before age 6. Thus, children who experienced sexual abuse may not have had the type of chronic exposure that would lead to more persistent dissociative tendencies. In contrast, physical abuse rather than sexual abuse is more likely to occur to children before the age of 4 (Administration for Children and Families, 2004), perhaps leading to earlier-onset pathological dissociation. These findings underscore the significance of properly assessing for these types of symptomatology early to provide proper treatment.
Prior research has made clear that abuse types rarely occur alone and that severity plays an important role in terms of predicting later pathology. Rather than subsuming categories according to a hierarchy of abuse types, the use of latent profiles (Pears et al., 2006) allowed us to utilize ecologically valid distinctions between groups. Because many of the maltreated children in the current study were subsequently involved in an intervention program, we plan to examine whether the program was able to decrease pathology in these subgroups.
Additional research will be important in further clarifying the relationship between maltreatment, PTSD, and dissociation during the preschool years. A major limitation of the study is that it utilized subscales of the CBCL to assess for PTSD and dissociative symptomatology. Although these scales are supported by the empirical literature, we must take caution in their interpretation, in part because the items assess a limited range of these constructs. Studies to establish convergent validity of the scales to the Child Dissociative Checklist are therefore planned. Other future directions may include studies on attachment and dissociation, so as to evaluate the prediction from betrayal trauma theory (Freyd, 1996) that abuse by a caregiver is particularly likely to lead to dissociation. Finally, with the longitudinal data we have collected we plan to measure changes in dissociation and other traumatic symptomatology over time. How might the impact of maltreatment at an early age affect the coherence of the self at later developmental stages?
The current study provides evidence that the experience of trauma is related to the development of dissociation and PTSD symptoms in preschool-age children. While these symptoms initially develop to help the child cope with maltreatment, they have lasting detrimental consequences. Because both pathological dissociation and PTSD symptomatology appear to have an early onset, it is clear that children should receive care as soon as possible after the discovery of maltreatment. Understanding these processes and their impact on the child can provide important information on how to minimize resulting academic, social, and psychological problems.
Acknowledgments
We are grateful to our participants and colleagues at Oregon Social Learning Center and the Freyd Dynamics Lab at the University of Oregon. Support for this research was provided by the following grants: DA021424 and DA017592, NIDA, US PHS; and MH059780, NIMH, US PHS. We would also like to acknowledge the Trauma and Oppression Research Fund at the University of Oregon.
References
- Achenbach TM. Integrative guide to the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington: University of Vermont, Department of Psychology; 1991. [Google Scholar]
- Administration for Children and Families. Child maltreatment annual reports: Reports from the States to the National Child Abuse and Neglect Data Systems. National statistics on child abuse and neglect. 2004 Retrieved August 25, 2006, from www.acf.hhs.gov/programs/cb/stats_research/index.htm.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth S, editors. Advances in applied developmental psychology: Child abuse, child development and social policy. Norwood, NJ: Ablex; 1993. pp. 7–73. [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease. 1986;174(12):727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Briere J. Child abuse trauma: Theory and treatment of the lasting effects. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Briere J, Runtz M. Symptomatology associated with childhood sexual victimization in an adult clinical sample. Child Abuse and Neglect. 1988;12:51–59. doi: 10.1016/0145-2134(88)90007-5. [DOI] [PubMed] [Google Scholar]
- Cholankeril A, Freyd JJ, Becker-Blease KA, Pears KC, Fisher PA. Examining dissociation in maltreated preschool children. Paper presented at the International Society for the Study of Dissociation International Fall Conference; Los Angeles, CA. 2006. Nov, [Google Scholar]
- Chu JA, Dill DL. Dissociative symptoms in relation to childhood physical and sexual abuse. American Journal of Psychiatry. 1990;147:887–892. doi: 10.1176/ajp.147.7.887. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry: Interpersonal and Biological Processes. 1993;56:96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Coons PM. Clinical phenomenology of 25 children and adolescents with dissociative disorders. Child and Adolescent Psychiatric Clinics of North America. 1996;5:361–373. [Google Scholar]
- Fisher PA, Burraston B, Pears KC. The Early Intervention Foster Care Program: Permanent placement outcomes from a randomized trial. Child Maltreatment. 2005;10:61–71. doi: 10.1177/1077559504271561. [DOI] [PubMed] [Google Scholar]
- Freyd JJ. Betrayal trauma: The logic of forgetting childhood abuse. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
- Hornstein NL. Complexities of psychiatric differential diagnosis in children with dissociative symptoms and disorders. In: Silberg JS, editor. The dissociative child: Diagnosis, treatment, and management. Baltimore; Sidran: 1993. pp. 27–46. [Google Scholar]
- Hornstein NL, Putnam FW. Clinical phenomenology of child and adolescent dissociative disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:1077–1085. doi: 10.1097/00004583-199211000-00013. [DOI] [PubMed] [Google Scholar]
- Irwin HJ. Proneness to dissociation and childhood traumatic events. Journal of Nervous and Mental Disease. 1994;182:456–460. doi: 10.1097/00005053-199408000-00006. [DOI] [PubMed] [Google Scholar]
- Kirby JS, Chu JA, Dill DL. Correlates of dissociative symptomatology in patients with physical and sexual abuse histories. Comprehensive Psychiatry. 1993;34:258–263. doi: 10.1016/0010-440x(93)90008-r. [DOI] [PubMed] [Google Scholar]
- Kisiel CL, Lyons JS. Dissociation as a mediator of psychopathology among sexually abused children and adolescents. American Journal of Psychiatry. 2001;158:1034–1039. doi: 10.1176/appi.ajp.158.7.1034. [DOI] [PubMed] [Google Scholar]
- Liotti G. Disorganization of attachment as a model for understanding dissociative psychopathology. In: Solomon J, George C, editors. Attachment disorganization. New York: Guilford Press; 1999. pp. 291–317. [Google Scholar]
- Macfie J, Cicchetti D, Toth S. The development of dissociation in maltreated preschool children. Development and Psychopathology. 2001a;13:233–254. doi: 10.1017/s0954579401002036. [DOI] [PubMed] [Google Scholar]
- Macfie J, Cicchetti D, Toth S. Dissociation in maltreated versus nonmaltreated preschoolers. Child Abuse and Neglect. 2001b;25:1253–1267. doi: 10.1016/s0145-2134(01)00266-6. [DOI] [PubMed] [Google Scholar]
- Malinosky-Rummel RR, Hoier TS. Validating measures of dissociation in sexually abused and nonabused children. Behavioral Assessment. 1991;13:341–357. [Google Scholar]
- Muthén LK, Muthén BO. User’s guide. 3rd. Los Angeles: Authors; 2004. Mplus: The comprehensive modeling program for applied researchers. [Google Scholar]
- Ogawa JR, Sroufe LA, Weinfeld NS, Carlson EA, Egeland B. Development and the fragmented self: Longitudinal study of dissociative symptomatology in a nonclinical sample. Development and Psychopathology. 1997;9:855–879. doi: 10.1017/s0954579497001478. [DOI] [PubMed] [Google Scholar]
- Pears KC, Kim HK, Fisher PA. Multiple facets of maltreatment as predictors of outcomes for preschoolers: A latent class analysis approach. Paper presented at the Society for Prevention Research; San Antonio, TX. 2006. May, [Google Scholar]
- Pfefferbaum B. Posstraumatic stress disorder in children: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(11):1503–1511. doi: 10.1016/S0890-8567(09)66558-8. [DOI] [PubMed] [Google Scholar]
- Putnam FW. Dissociation in children and adolescents. New York: Guilford Press; 1997. [Google Scholar]
- Putnam FW, Helmers K, Trickett PK. Development, reliability, and validity of a child dissociation scale. Child Abuse & Neglect. 1993;17(6):731–741. doi: 10.1016/s0145-2134(08)80004-x. [DOI] [PubMed] [Google Scholar]
- Sanders B, Giolas MH. Dissociation and childhood trauma in psychologically disturbed adolescents. American Journal of Psychiatry. 1991;148:50–54. doi: 10.1176/ajp.148.3.A50. [DOI] [PubMed] [Google Scholar]
- Sim L, Friedrich WN, Hobart Davies W, Trentham B, Lengua L, Pithers W. The Child Behavior Checklist as an indicator of posttraumatic stress disorder and dissociation in normative, psychiatric, and sexually abused children. Journal of Traumatic Stress. 2005;18:697–705. doi: 10.1002/jts.20078. [DOI] [PubMed] [Google Scholar]
- Terr L. Childhood traumas: An outline and overview. American Journal of Psychiatry. 1991;148:10–19. doi: 10.1176/ajp.148.1.10. [DOI] [PubMed] [Google Scholar]
- Waldinger RJ, Swett C, Frank A, Miller K. Levels of dissociation and histories of reported abuse among women outpatients. Journal of Nervous and Mental Disease. 1994;182:625–630. doi: 10.1097/00005053-199411000-00005. [DOI] [PubMed] [Google Scholar]
- Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. American Journal of Psychiatry. 1999;156:1223–1229. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Shea MT, Pearlstein T, Begin A, Simpson E, Costello E. Differences in dissociative experiences between survivors of childhood incest and survivors of assault in adulthood. Journal of Nervous and Mental Disease. 1996;184:52–54. doi: 10.1097/00005053-199601000-00009. [DOI] [PubMed] [Google Scholar]


