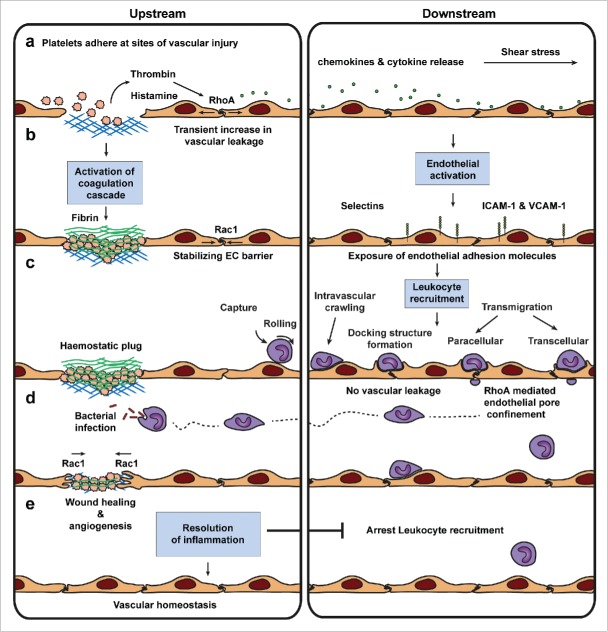
Figure 3.
Leukocyte diapedesis and vascular permeability are uncoupled events. Vascular injury in the skin is resolved by various sequential processes that initiate tissue repair and the clearance of pathogens and dirt to restore vascular homeostasis. (a) In the first step of the cascade, platelets adhere to exposed collagen forming a haemostatic plug of fibrin that arrests blood leakage (a-c). Activated platelets produce thrombin, a compound that activates the coagulation cascade to produce the haemostatic plug. Thrombin released by activated platelets and histamine released by tissue basophils and mast cells are thought to initiate endothelial activation, a transient increase in endothelial permeability provoked by RhoA-mediated actomyosin contractility, and local enhancement of blood flow. This results in chemokine and cytokine release by various cell types followed by inflammation close to the site of injury. (b) Downstream of vascular injury endothelial cells get activated and in turn expose a variety of adhesion molecules at their surface. Upstream the transient permeability increase is counterbalanced by Trio-Rac1-mediated JAILs that stabilize endothelial junctions. (c) Leukocyte recruitment downstream of vascular leakage and vascular damage is believed to follow the multistep paradigm of TEM. Vascular leakage during leukocyte diapedesis is prevented by RhoA-mediated endothelial pore confinement. (d) Infiltrating leukocytes scan and clear pathogens and dirt from the site of infection. Rac1-mediated wound healing and angiogenesis repair damaged tissue and vessels. (e) Finally, tissue macrophages secrete chemokines that resolve inflammation arresting leukocyte recruitment to restore vascular homeostasis.