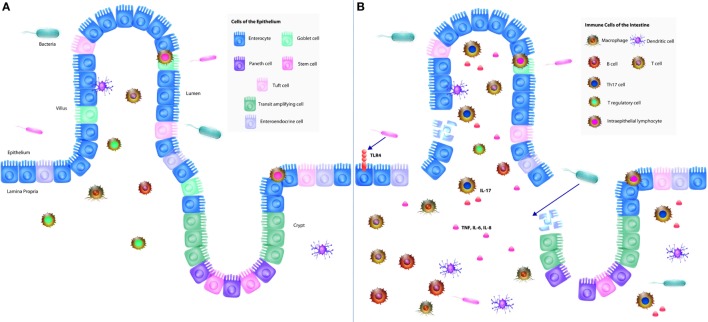
Figure 1.
The neonatal intestinal immune system and its interaction in the pathogenesis of necrotizing enterocolitis (NEC). (A) The intestinal mucosal immune system is comprised of the cells of the epithelium, immune cells, and commensal bacteria. The epithelium consists of villi and crypts. Enterocytes, goblet cells, enteroendocrine cells, and tuft cells exist within the villi, whereas Paneth cells and stem cells occupy the base of the crypts. Immune cells consist of intraepithelial lymphocytes, T regulatory cells (Tregs), T cells, B cells, macrophages, and dendritic cells, which reside predominantly in the lamina propria underlying the epithelium. Commensal bacteria inhabit the lumen of the gut, which constantly interact with the epithelium and immune cells to help maintain protection against pathogenic bacteria. (B) In NEC, lipopolysaccharide from Gram-negative bacteria interact with toll-like receptor 4 (TLR4) expressed by predominantly by enterocytes, which results in the breakdown of the gut barrier, allowing for pathogenic bacterial translocation. A pro-inflammatory response follows resulting in increased production of pro-inflammatory cytokines (IL-6, IL-8, and TNF) as well as increased Th17 cells and decreased Tregs. The combination of these cellular responses with TLR4 signaling results in a profound inflammatory response and subsequently NEC.