FIG 1.
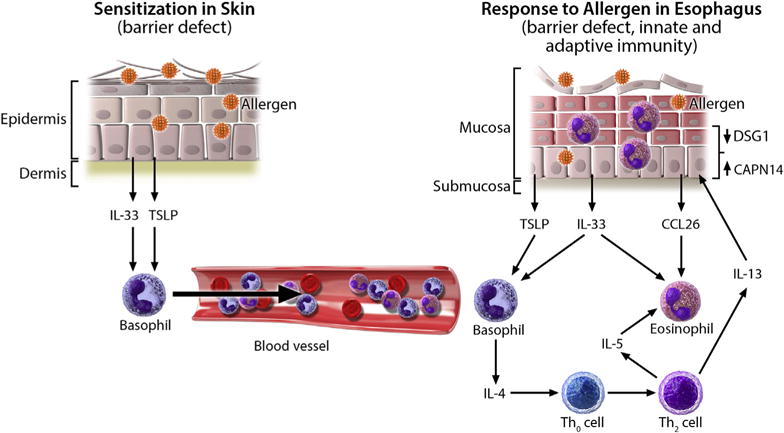
Proposed model for the development of allergic inflammation in patients with EoE. Impaired skin barrier integrity, such as that caused by injury or FLG mutations, allows for increased allergen penetration through the epithelium, causing allergic sensitization and release of IL-33 and TSLP from the epithelium. Secondary to activation by these cytokines, there is increased trafficking of basophils through the bloodstream to the esophagus. Later, direct exposure of allergens to the esophageal epithelium leads to the release of TSLP and IL-33, which induce IL-4 production from basophils and subsequent release of IL-5 and IL-13 from TH2 cells. IL-13 causes esophageal epithelial barrier impairment and increased allergen exposure by decreasing desmoglein 1 (DSG1) and increasing calpain 14 (CAPN14) expression. Additionally, IL-13 induces CCL26 production from the epithelium, which, in combination with IL-5, causes eosinophil infiltration into the esophagus.
