Abstract
More than 200 different surgical techniques exist for hallux valgus (HV). Some of them are designed for mild, moderate, or severe deformities depending on their correction power. Nevertheless, they all correct only the coronal and/or sagittal plane deformity. Just a handful of them correct the known axial malrotation that exists in most HV cases. This malrotation is one possible factor that could be the source of recurrence of an operated HV as it has been described. We describe a new technique which simultaneously corrects the metatarsal internal rotation and varus deformity by rotating the metatarsal through an oblique plane osteotomy. This is performed with no bone wedge resection. Also, there is a broader bone surface contact than on a transverse proximal osteotomy. This technique is easy to remember and relatively simple to perform in primary and revision cases. The authors results show that it is as safe and effective as other procedures, with some advantages to be discussed.
Levels of Evidence: Diagnostic Level 5. See Instructions for Authors for a complete description of levels of evidence.
Key Words: hallux valgus, surgical technique, osteotomy, rotational correction
HISTORICAL PERSPECTIVE
Hundreds of surgical techniques exist for hallux valgus (HV), arguably no technique being significantly better than the others. Osteotomies have been recommended for HV surgery since the last 2 decades, with good success rate and reliable over time.1 The recurrence rate of the deformity depends on the preoperative deformity and also on the postoperative sesamoid reduction quality, being higher if the HV angle is >37 to 40 degrees, and if postoperatively there is an incomplete reduction of the sesamoids.2–4 No osteotomy has been proven to be more effective than the others, and different modifications have been made to improve the outcomes of each individual technique.5 Most modifications try to address the deformity in just 1 plane, the coronal one. But there is another deformity not frequently discussed: the first-ray axial malrotation. Up to 87% of HV cases present with a metatarsal internal rotation, shown by an internally malrotated hallux (on clinical examination), visible metatarsal head condyles on a foot anteroposterior x-ray and by laterally subluxated sesamoids as seen on x-rays.6 Interestingly, in this same study, up to 25% of the cases with HV deformity presented with a pronated first metatarsal bone and with no sesamoid subluxation on computed tomographic scan, and no correlation was found between the metatarsal pronation and the HV or intermetatarsal (IMTT) angle. These facts highlight the importance of understanding the first metatarsal rotational deformity, as it is more frequently found in HV deformity than coronal deformities or sesamoid subluxation. It has been shown that this malrotation could play a role in HV recurrence rate and in postoperative clinical appearance.7
Any osteotomy performed should be powerful enough to align the metatarsophalangeal joint and to locate the first metatarsal as parallel as possible to the second metatarsal (correcting coronal plane deformity), but also to locate the first metatarsal on top of the sesamoids (correcting the axial plane deformity, ie, malrotation). Even when the metatarsal is placed perfectly parallel to the second metatarsal after a classic HV osteotomy, the sesamoids frequently remain laterally subluxated because no malrotation is addressed.
The rotational osteotomy we present here was initially described by Rab in 1988 for tibial Blount’s disease.8,9 In Blount’s disease there is a tibial varus and internal rotation deformity, therefore needing a 2-plane correction. Its main advantages are a broad bone contact, deformity correction capacity in 2 planes and no loss of bone length. Its main downside is that the orientation of the osteotomy is paramount to obtain the desired correction. It consists of a single oblique cut, through which rotation is corrected. Because of the oblique nature of this osteotomy, while rotating the bone through this oblique plane the coronal deformity is corrected. Mathematical models,10 graphical analysis,10,11 and 3-D planning12 have been used to prove its utility in correcting long bone multiple plane deformities. Even a small series of tibial osteotomies were published in 1989.13 In 1992 Waanders and Herzenberg14 published the same concept using Ilizarov external fixation. Probably given the appearance of hexapods that allowed bony correction in all possible planes, is that this technique lost its interest in the medical community. Currently, only a handful of orthopedic books keep describing it.
The osteotomy we present here was called the PROMO: Proximal ROtational Metatarsal Osteotomy. It is performed through a single proximal metatarsal oblique plane osteotomy, achieving any deformity correction through rotation. This is a concept infrequently described in literature. Any kind of deformity (sagittal or coronal deformity) can be corrected using bone rotation through a single oblique cut. A second cut to remove a wedge is not necessary. Just by rotating the bone through an oblique plane osteotomy any deformity correction can be achieved. The only requirement for this osteotomy to work, is the coexistence of a malrotation, given that only through rotation the coronal or sagittal deformities can be corrected. Of course, the direction of that oblique cut has to be carefully planned to perform it in the right direction.
We report the results of our first 6 patients we operated using this technique. Complete deformity correction was achieved in all patients with no relapse. A fast rehabilitation was allowed given the osteotomy high stability (oblique plane osteotomy, allowing a lag screw on cortical bone). A high reproducibility between surgeons has been evident given logic and easy osteotomy landmarks.
INDICATIONS AND CONTRAINDICATIONS
The main contraindication for this osteotomy is a HV mild deformity with no or minimal rotation. Mild HV usually is satisfactorily corrected using a Chevron osteotomy using just lateral translation. There are only a handful of cases, mostly in youngsters, of moderate to severe HV with no malrotation.
PREOPERATIVE PLANNING
Our aim in any HV surgery is to relocate the first metatarsal above the sesamoids. The IMTT angle is measured to evaluate the deformity severity on an anteroposterior foot x-ray. This angle is obtained by measuring the divergence between the first and second metatarsal. The angle to be corrected is also measured, to get a more precise measure of how many degrees are needed to place the metatarsal head over the sesamoid complex.15 The main downside of any angular measurement, is the limited capacity to evaluate metatarsal malrotation, demonstrated by sesamoid subluxation. Axial sesamoids x-rays can give a rough estimate of first-ray malrotation. Another option is to perform a preoperative computed tomographic scan, which could assess metatarsal rotation and sesamoid subluxation. The authors assess rotation by clinical examination of the great toe rotation. An easy way to perform this is to measure the great toe nail inclination relative to the floor using a goniometer.
A 30-degree great toe internal rotation will be taken for this example together with a 15-degree IMTT angle. The objective will be to correct 15 degrees of varus angulation (leave both metatarsals shafts parallel) and 30 degrees of internal rotation. After the metatarsal osteotomy is performed, an optional phalangeal osteotomy (Akin osteotomy) should be performed depending on the remaining interphalangeal deformity.
There are different ways for obtaining this ideal osteotomy direction (graphs, equations, etc.),10–12 but the easiest, fastest, and most practical way is utilizing an application available for handheld devices. It is available for free in the App-store (Apple) and Play-store (Android). It is called the “Multiplier” application. It gives the osteotomy direction with mathematical precision using published formulas.
Initially, this technique was tried on wax candles (Figs. 1–3). After this stage, this osteotomy was performed on 12 identical Synbone (Synbone AG, Malans, Switzerland) models. Each model consisted of a HV model, that included the first and second ray. They were modified so they had an IMTT angle of 15 degrees and a first-ray internal rotation of 30 degrees (Figs. 4, 5). Every osteotomy was performed with an electric oscillating microsagittal saw, and then fixed with a K-wire.
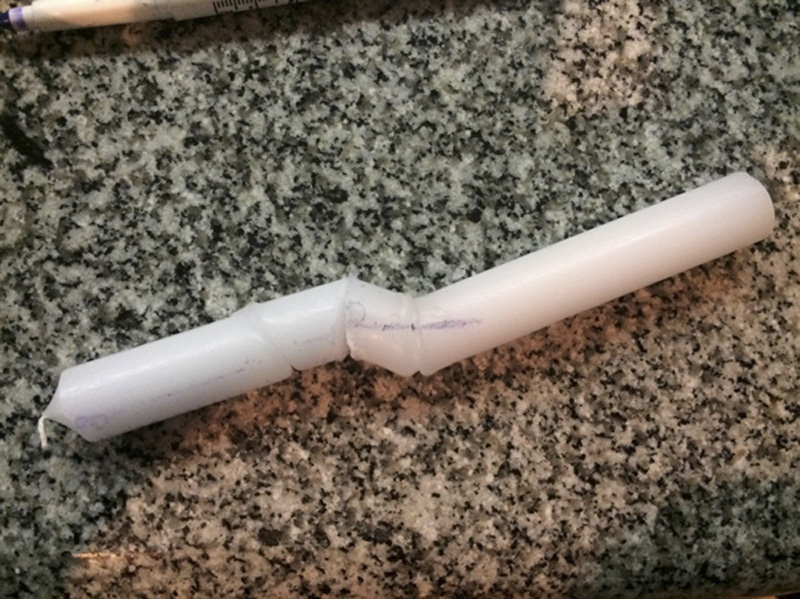
FIGURE 1.

Candlewax precut.
FIGURE 3.
Candlewax after rotating the distal part.
FIGURE 4.
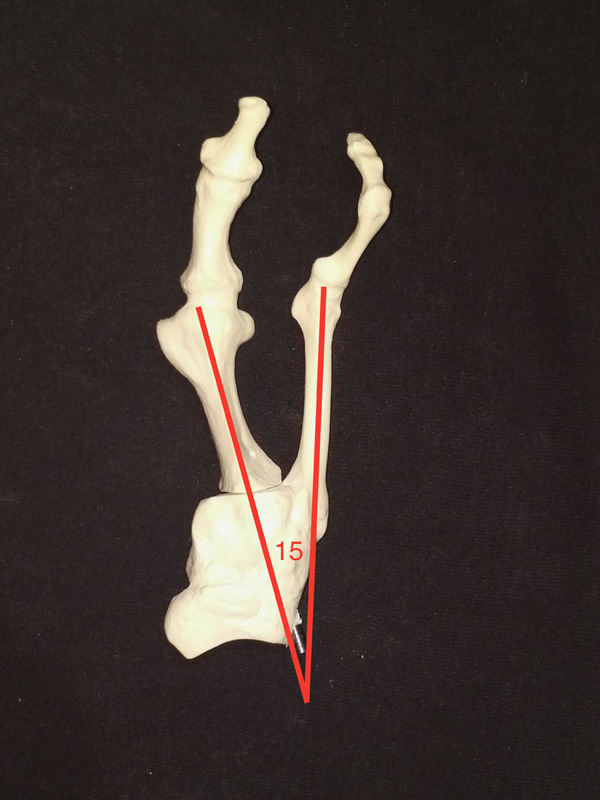
Model anteroposterior view, showing 15 degrees of intermetatarsal angle.
FIGURE 5.
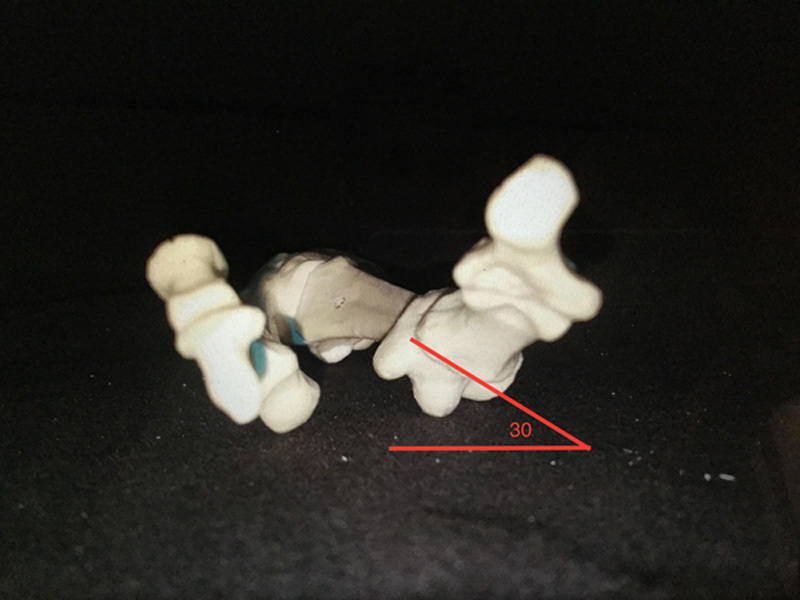
Model axial view, showing 30 degrees of internal rotation.
FIGURE 2.
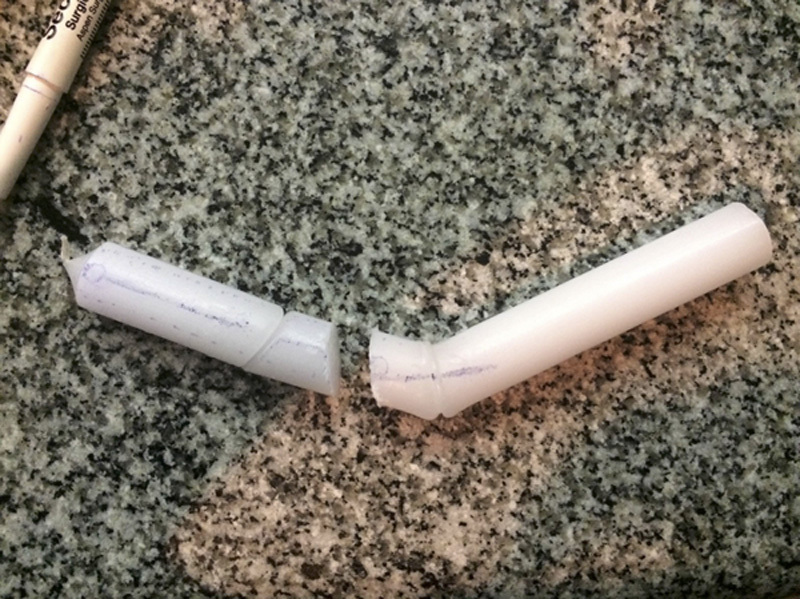
Candlewax postcut.
TECHNIQUE
The technique shown will consider a HV case with 15 degrees of IMTT angle and a metatarsal internal rotation of 30 degrees (Fig. 6).
FIGURE 6.

Foot anteroposterior x-ray showing a hallux valgus deformity, with 15 degrees of intermetatarsal angle.
Preoperatively the osteotomy direction has to be obtained. Using the Multiplier application, under the menu “Additional resources” and then “Inclined Osteotomy rotation angle,” the coronal plane and axial plane deformity values are entered: 30 degrees of internal rotation and 15 degrees of angulation (IMTT angle) (Fig. 7). For this case the following values will come up: (1) rotational orientation of the osteotomy: 15 degrees external (value 1); (2) vertical inclination of the osteotomy: 26 degrees (value 2) (Fig. 8). An easy way to follow this angulation is to use a sterile goniometer while performing the osteotomy (author’s choice).
FIGURE 7.
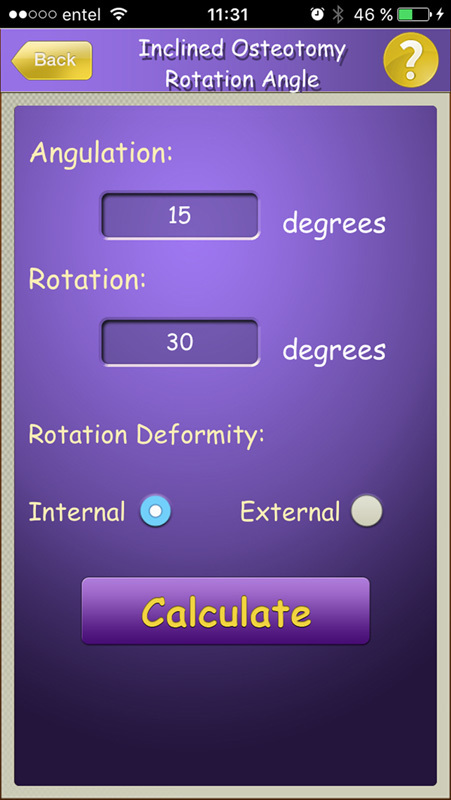
Multiplier application: entering deformity parameters.
FIGURE 8.
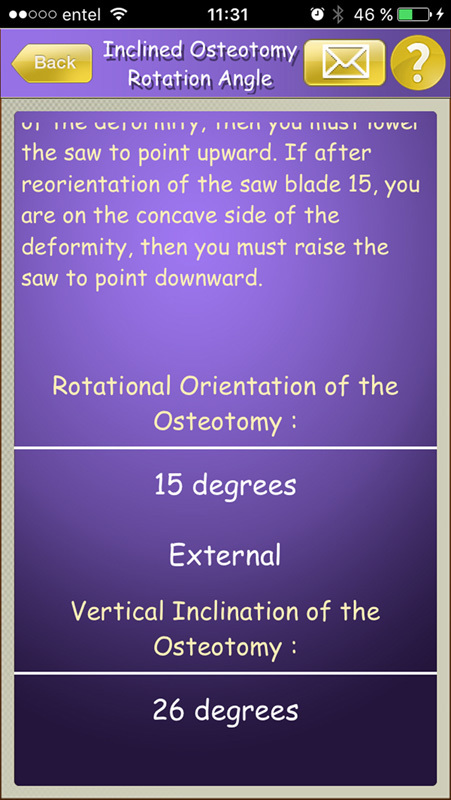
Multiplier application: osteotomy direction.
A longitudinal medial skin incision is made as usual over the metatarsophalangeal joint, carefully handling soft tissues. We perform a transarticular capsulotomy through the medial approach. This approach is our preferred technique, given that it has been shown that an open lateral release in severe HV cases does not add any correction power nor improve functional outcomes.16
Once the proximal metatarsal is exposed, draw a medial metatarsal midaxis line (A) using the electrocautery/marking pen. Draw another line (B) along the bone axis 5 mm dorsal to the medial midaxis line already drawn (Fig. 9). On a metatarsal with a 0.9 cm radius, 5 mm on the metatarsal’s periphery equals a 30-degree arc. This value (5 mm) depends on the rotational deformity that has to be corrected (30 degrees in this case). For 20 degrees of great toe internal malrotation, these lines should be 3 mm apart. For 45 degrees of malrotation this value should be 7 mm.
FIGURE 9.
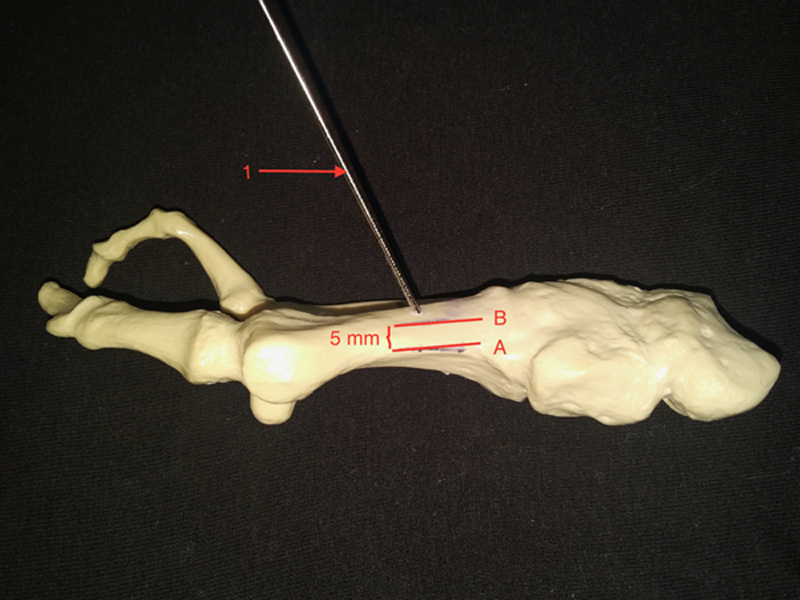
Model medial view, showing lines (A) and (B). Line (A) is midaxis medial line and (B) is 5 mm above (A). The numerical 1 is K-wire (1), showing its dorsal entry point.
A K-wire (1) is driven dorsal-distal to plantar-proximal in 26 degrees (value 2) off the metatarsal perpendicular line (or 74 degrees off the metatarsal axis), starting dorsally 2 cm distal to the tarsometatarsal (TMTT) (Figs. 9, 10). Another K-wire (2) is driven medial to lateral, starting on the medial metatarsal midaxis line 2 cm distal to the TMTT. It should be placed perpendicular to the bone in the frontal plane (Fig. 11) and in 15 degrees of elevation from the floor plane (value 1) (going dorso-medial to plantar-lateral) (Fig. 12). Next, following the same direction of K-wire (1) and (2), perform the osteotomy using a microsagittal saw (Fig. 13). Be careful not to erase lines (A) and (B). Perform the osteotomy slowly with a sharp blade and cool it frequently with saline solution. Once the osteotomy is performed, using a field clamp or Backhaus, grab the distal loose end of the metatarsal, and rotate it externally to match lines (A) and (B) (Fig. 14). Next, drive a K-wire (3) perpendicular through the osteotomy (as perpendicular as possible) as transient fixation (Figs. 14, 15). This is where the lag screw will be located (Fig. 16). Drive another K-wire (4) through the osteotomy to improve temporary fixation stability.
FIGURE 10.
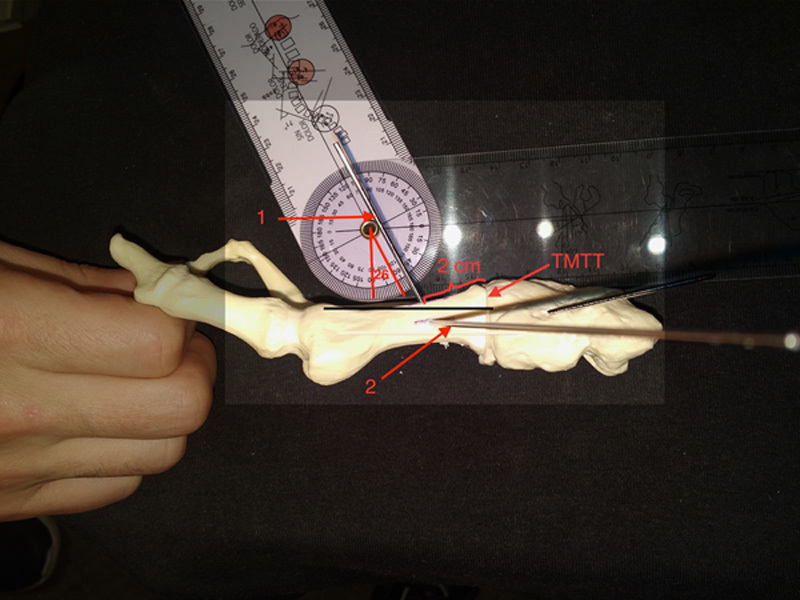
Model medial view showing 26 degrees of angulation of K-wire (1), from distal-dorsal to plantar-proximal. The numerical 2 is K-wire (2). Both K-wires entry point is located 2 cm distal to the tarsometatarsal joint (TMTT).
FIGURE 11.
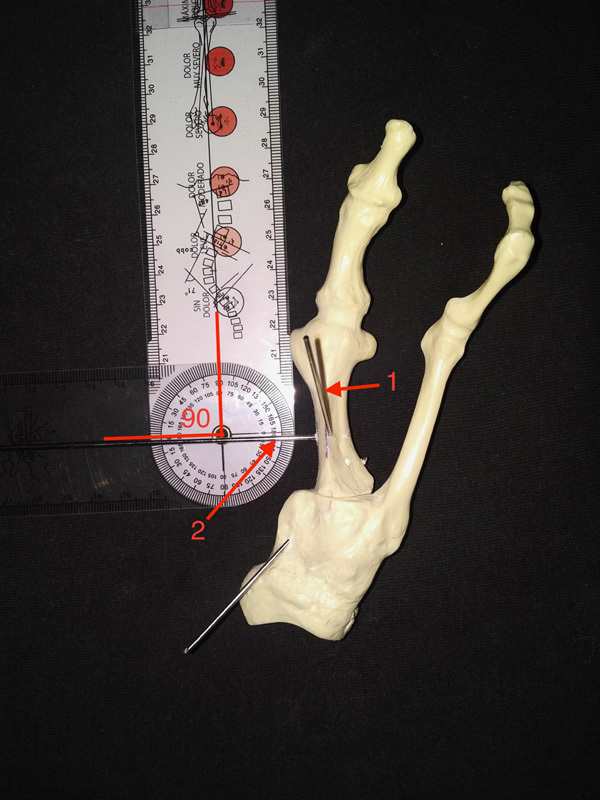
Model anteroposterior view showing perpendicular orientation of K-wire (2) to the first metatarsal.
FIGURE 12.
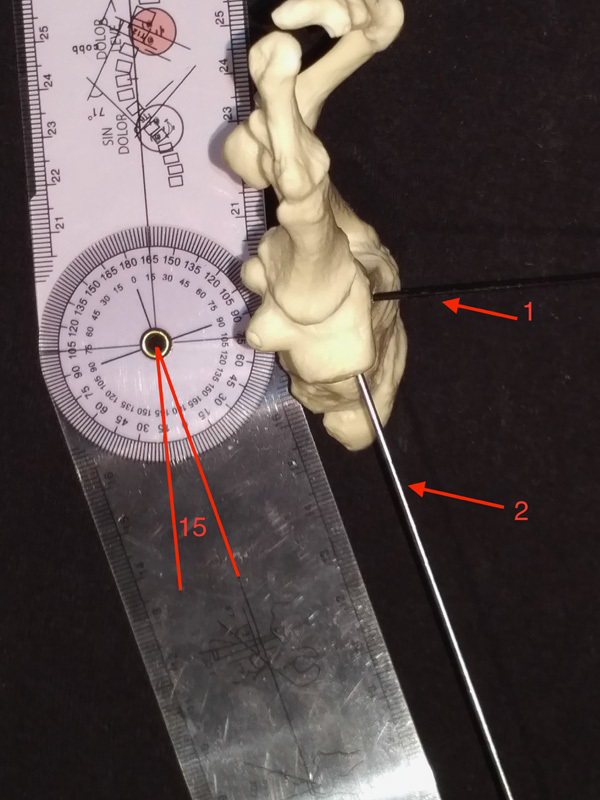
Model axial view showing K-wire (2) with 15 degrees of elevation from the ground.
FIGURE 13.

Model anteroposterior view showing the saw cut following both K-wires orientation.
FIGURE 14.
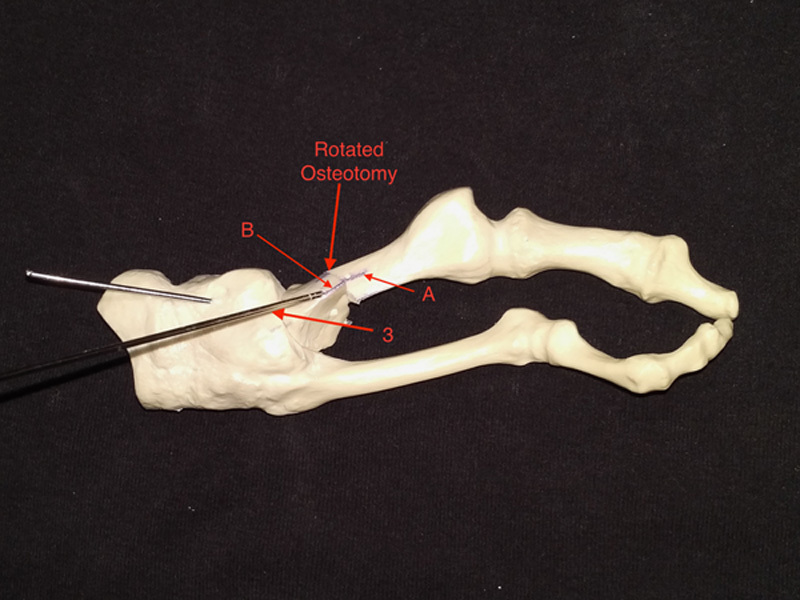
Model anteroposterior view after deformity correction, achieved through metatarsal external rotation. See how lines (A) and (B) match on the dorsum of the metatarsal. The numerical 3 indicates K-wire (3), which fixates the osteotomy.
FIGURE 15.
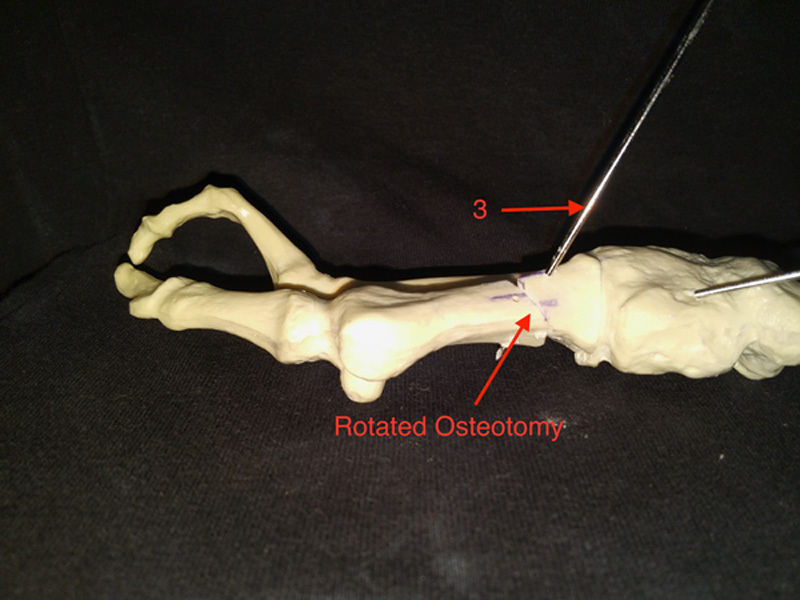
Model medial view after deformity correction. Note that there is neither metatarsal elevation nor depression.
FIGURE 16.
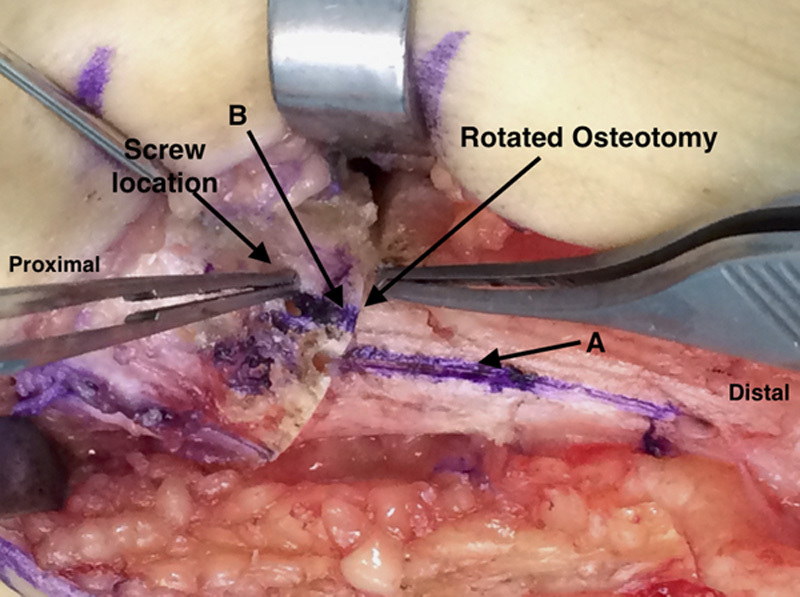
Medial in vivo foot view after osteotomy rotation. See how lines (A) and (B) match (there is a fake lines mismatch given the oblique direction of the picture). The proximal forceps shows the screw location. The distal forceps shows the osteotomy location.
Check under image intensifier a satisfactory deformity correction. First and second metatarsals shafts should be parallel (Fig. 17). Place a 2.7 lag screw using cannulated instruments through K-wire (3) (Fig. 18). Do not remove K-wire (4). Place a medially located locking plate, using 2 screws proximal and 2 screws distal to the osteotomy (Figs. 19, 20). Remove K-wire (4). Add an Akin osteotomy as needed depending on the interphalangeal angle and metatarsophalangeal soft tissue balance. Perform the bunionectomy at the end of the procedure as needed. Check the final toe rotation by clinical examination (Fig. 21).
FIGURE 17.
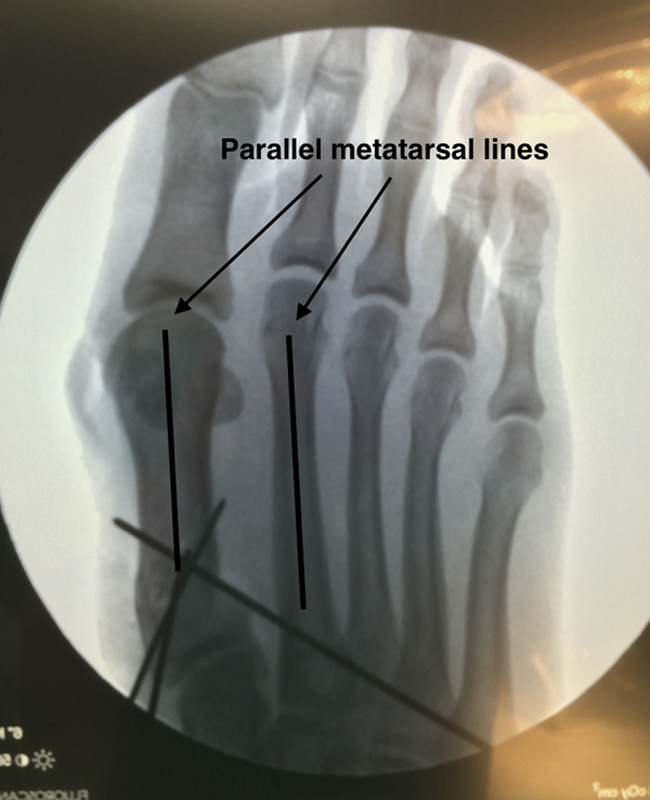
Anteroposterior foot fluoroscopy, showing metatarsal deformity correction with both metatarsals shafts parallel.
FIGURE 18.
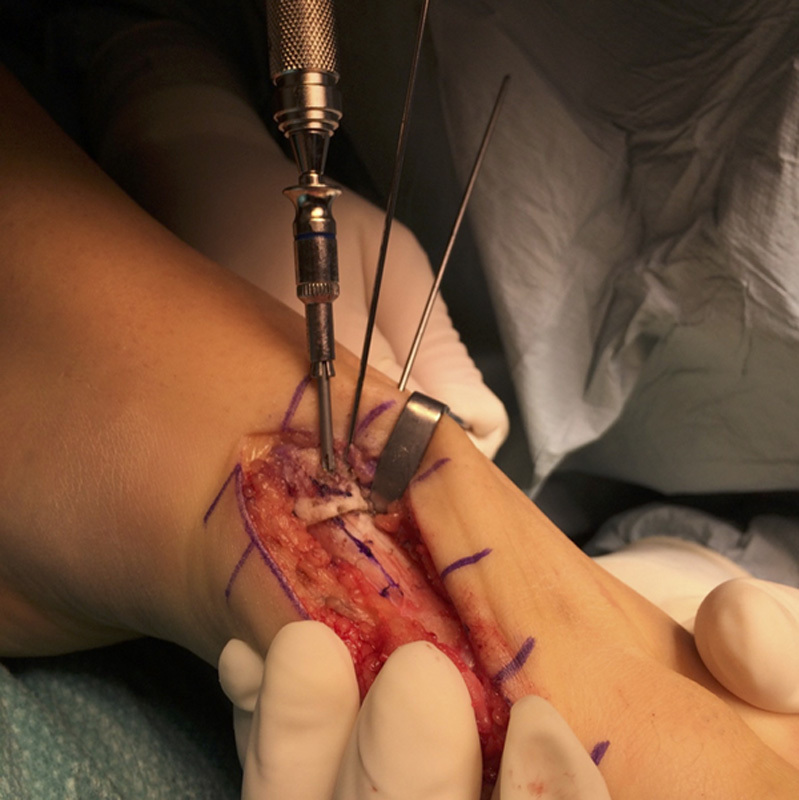
Medial foot view, showing screw insertion.
FIGURE 19.
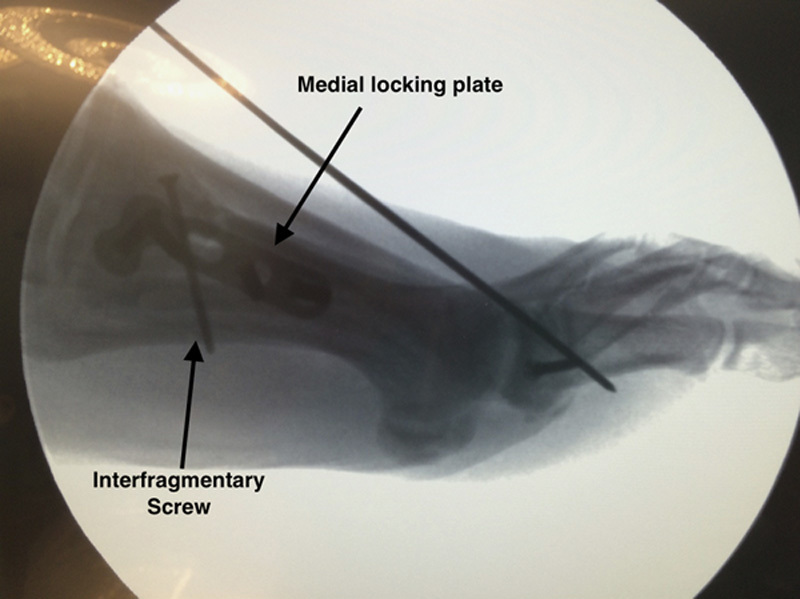
Lateral foot fluoroscopy, showing interfragmentary screw and medial plate location. The wire seen in the figure is holding an Akin osteotomy, not discussed in this research.
FIGURE 20.
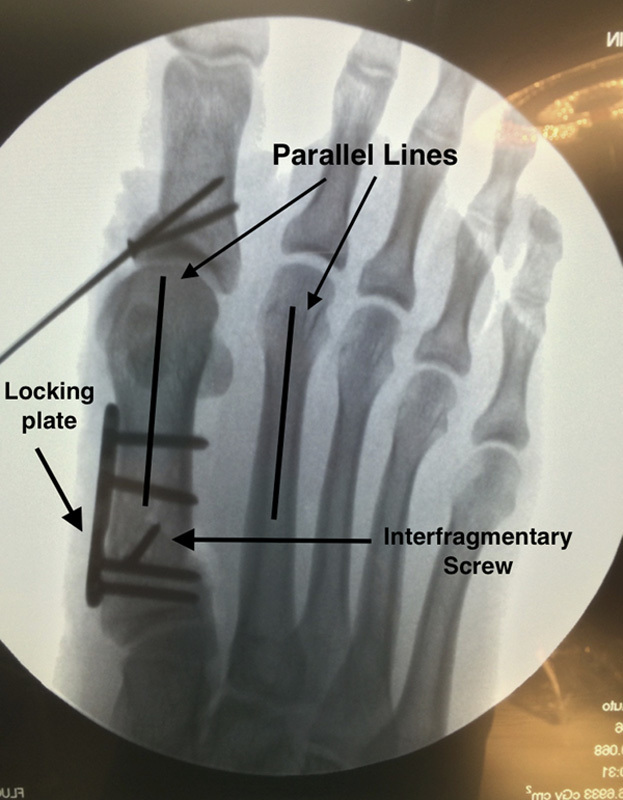
Anteroposterior foot fluoroscopy, showing a medial metatarsal locking plate, the interfragmentary screw position, and the metatarsal deformity correction.
FIGURE 21.

Model axial view, showing complete rotational correction.
RESULTS
We report the results of our first 6 patients we operated on after 7 months follow-up. The average preoperative/postoperative metatarsophalangeal angle was 35/5 degrees, the IMTT angle was 16/5 degrees, and the mean great toe internal malrotation was 35/5 degrees. No metatarsal shortening was observed whatsoever. The preoperative/postoperative AOFAS score was 55/85 after 7 months follow-up. All 6 patients were satisfied with the surgery. Because of the complete coronal and axial deformity correction achieved, no recurrence has been observed in our case series. A fast rehabilitation is allowed given its high stability (oblique plane osteotomy, allowing a lag screw on cortical bone) and a high reproducibility between surgeons has been evident given logic and easy osteotomy landmarks.
COMPLICATIONS
No complications were reported during this study follow-up, such as deformity relapse, infections or deep vein thrombosis, between others. The authors think that the complications would not differ from other classic HV surgery complications, that is, infection, wound dehiscence, deep vein thrombosis, between others. Deformity recurrence is probably going to be less frequent than in other metatarsal osteotomies for moderate-severe HV given this osteotomy rotational correction.
POSTOPERATIVE MANAGEMENT
Weight-bearing is allowed as tolerated immediately postoperatively using a hard sole postoperative shoe. Great toe range of motion exercises are encouraged once wounds are completely healed, fact that happened at 2 weeks on an average. Transition to a conventional shoe happens at 1 month postoperative.
POSSIBLE CONCERNS-FUTURE OF THE TECHNIQUE
For moderate and severe deformities for patients younger than 50 years old, the authors think that a PROMO osteotomy is the treatment of choice. In case of elderly patients or a grossly unstable TMTT joint, a Lapidus procedure should be the procedure of choice. This osteotomy is very powerful and can correct even severe deformities with substantial rotation. The PROMO technique should never be used if there is no malrotation. This is common in mild HV, where a pure translating osteotomy (Chevron) is enough to achieve a satisfactory correction.
Although this is a very small series of patients, the authors have seen a reliable and rapid bone consolidation. This could be due to a larger bone apposition area than in a classic transverse osteotomy and due to the lag screw, which gives better stability and compression.
The authors think that this new osteotomy is reliable, versatile, and easy to perform, and it combines coronal and rotational deformity correction without any bone resection. Hopefully addressing the HV deformity as a biplanar deformity will allow us to decrease the recurrence risk.
ACKNOWLEDGMENT
The main author would like to warmly acknowledge Dr. John E. Herzenberg, for his always kind, sage and invaluable support and advice.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Trnka HJ. Osteotomies for hallux valgus correction. Foot Ankle Clin. 2005;10:15–33. [DOI] [PubMed] [Google Scholar]
- 2.Deenik AR, de Visser E, Louwerens J-WK, et al. Hallux valgus angle as a main predictor for correction of hallux valgus. BMC Musculoskelet Disord. 2008;9:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okuda R, Kinoshita M, Yasuda T, et al. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011;16:760–764. [DOI] [PubMed] [Google Scholar]
- 4.Okuda R, Kinoshita M, Yasuda T, et al. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009;91:1637–1645. [DOI] [PubMed] [Google Scholar]
- 5.Wagner E, Ortiz C. Osteotomy considerations in hallux valgus treatment improving the correction power. Foot Ankle Clin N Am. 2012;17:481–498. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y, Kim J, Young K, et al. A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int. 2015;36:944–952. [DOI] [PubMed] [Google Scholar]
- 7.Okuda R, Kinoshita M, Yasuda T, et al. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2007;89:2163–2172. [DOI] [PubMed] [Google Scholar]
- 8.Rab GT. Oblique tibial osteotomy for Blount’s disease (tibia vara). J Pediatr Orthop. 1988;8:715–720. [DOI] [PubMed] [Google Scholar]
- 9.Rab GT. Oblique tibial osteotomy revisited. J Child Orthop. 2010;4:169–172. Epub December 20, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sangeorzan BJ, Sangeorzan BP, Hansen ST, Jr, et al. Mathematically directed single-cut osteotomy for correction of tibial malunion. J Orthop Trauma. 1989;3:267–275. [DOI] [PubMed] [Google Scholar]
- 11.Paley D. Principles of Deformity Correction. Berlin: Springer-Verlag; 2002:256–268. [Google Scholar]
- 12.Dobbe JG, Pré KJ, Kloen P, et al. Computer-assisted and patient-specific 3-D planning and evaluation of a single-cut rotational osteotomy for complex long-bone deformities. Med Biol Eng Comput. 2011;49:1363–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruse RW, Bowen JR, Heithoff S. Oblique tibial osteotomy in the correction of tibial deformity in children. J Pediatr Orthop. 1989;9:476–482. [PubMed] [Google Scholar]
- 14.Waanders NA, Herzenberg JE. The theoretical application of inclined hinges with the Ilizarov external fixator for simultaneous angulation and rotation correction. Bull Hosp Jt Dis. 1992;52:27–35. [PubMed] [Google Scholar]
- 15.Ortiz C, Wagner P, Vela O, et al. “Angle to Be Corrected” in preoperative evaluation for hallux valgus surgery: analysis of a new angular measurement. Foot Ankle Int. 2016;37:172–177. [DOI] [PubMed] [Google Scholar]
- 16.Wagner E, Ortiz C, Figueroa F, et al. Role of a limited transarticular release in severe hallux valgus correction. Foot Ankle Int. 2015;36:1322–1329. [DOI] [PubMed] [Google Scholar]


